This process also produces an inflammatory response, so it makes sense also to measure white blood cell count.) This leads to an increase in erythrocyte sedimentation rate (ESR) through increased fibrinogen-sticking red blood cells.
Warfarin generally works by suppressing the liver’s production of factors that induce clotting. This process is extrinsic, as it is in the liver and outside the blood. It is also relatively slow, as it takes up to five days for warfarin to work.
The usual blood test for warfarin is the international normalised ratio (INR), which essentially measures how long it takes the blood to clot in a lab, converted to an arbitrary value of 1. If, following warfarin, the INR rises to 2, the blood is therefore taking twice as long to clot. Generally, an INR greater than 4 is problematic for bleed management, and may affect decisions about micro-surgery and injection interventions.
The INR is ultimately a marker of fibrinogen production, and thus liver function (as this is where fibrinogen is made). It is also used as a surrogate marker of liver function in patients who are not on warfarin. If INR is measured in an alcoholic patient (it is quick and cheap) and the result is 7, liver dysfunction would be highly likely.
Heparin, clexane, deltaparin and low molecular weight heparin work via an intrinsic pathway, inside the blood, by directly binding to (and thus deactivating) chemicals that induce a clot. These medications will therefore work very quickly (within a few minutes) and can also be used as a prophylaxis. In view of their quick action, they are often given as a dual therapy with warfarin, as the latter takes a few days to work. In primary care, blood tests are less likely to be ordered for patients on these types of therapies. The test to assess these interventions is called aPTT and is usually ordered before invasive intervention.
The final group of therapies work on the platelets so they are intrinsic and can be assessed by aPTT. These include aspirin and clopidogrel. The drugs are converted in the liver into pro-drugs, which remain in production for a few days after the oral base drug has ceased. The platelets express sticky surface proteins (like a Velcro coat), which enable them to stick together and clot. This protein is called Von Willebrand’s factor (VWF) and it is suppressed by the pro-drug. Once suppressed, it is likely that the platelets will have suppressed clotting ability for their lifespan of up to two weeks. Patients on high doses of such treatments may need platelet replacement to prevent bleeds – though not while the pro-drug is being made by the liver, as this will simply affect the newly transfused platelets.
Alcohol works on both intrinsic and extrinsic pathways. ESR can also be used to indicate cancer, myeloma and macrocytic anaemia and so could be being used for this reason. ESR also increases with age. Storytelling: Acutely, alcohol ‘gets the platelets drunk’ by suppressing their VWF activity. This makes them take off their sticky coats and reduces their ability to stick together. Hence, sword fighting after drinking wine is not a good idea! In alcoholic patients, this acute phase is augmented by liver dysfunction – the liver does not produce fibrinogen and clotting times increase significantly.
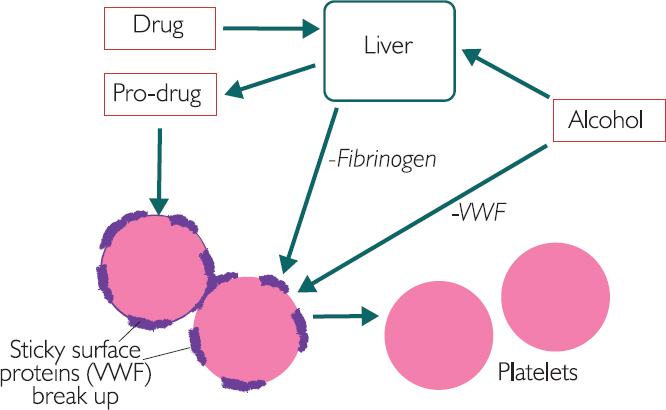
Figure 6.1: The interaction between alcohol, drugs and the liver
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree