Background
As with all other organ systems, the endocrine axes are subject to physiological and pathological changes with aging. The purpose of this chapter is to assist the reader in the diagnosis of the latter in the context of the former. That is, as physicians and laboratorians, we must be able to distinguish the normal effects of aging on the patient’s clinical presentation and biochemistry from those of disease states. Unfortunately, there are many contexts where normal aging and pathophysiology have phenotypic overlap to the point where the distinction between the two may become more philosophical than biomedical. To that end, this chapter will review the endocrine axes delineating some of the known physiological changes and their effect on reference intervals and diagnosis of specific disease entities. Particular attention will be paid to issues that commonly arise in clinical practice. Unfortunately some of the questions posed in clinical practice are generated from an industry of “wellness” and “antiaging” medicine that has found an entrepreneurial niche in some Western countries. Between the effects of trends in medical entrepreneurship and the rise in the average life span, these diagnostic challenges are becoming increasingly prevalent and the clinician must be prepared with a diagnostic strategy and approach in response to pressure to treat what may be entirely normal—where the treatment itself may have no proven scientific benefit and may pose risk of harm.
Hypothalamic-pituitary-gonadal/adrenal androgen axes
Menopause and its biochemical features
Menopause is defined clinically, not biochemically, though it has numerous biochemical correlates. Menopause is retrospectively determined after the cessation of the menses for a duration of 12 consecutive months without the identification of any underlying physiological stressor or pathological cause . The median age of menopause was determined to be 51.4 years from the Massachusetts Women’s Health Study . Frequency of ovulation decreases by age 40 years in most women before its ultimate cessation, during which time ovarian follicular numbers decline to the point where their function deteriorates. Menstrual cycle lengths become variable—either due to irregular follicular maturation with decreased responsiveness to gonadotropins or cycles may be anovulatory without evidence of a functioning corpus luteum .
Gonadotropins, inhibins, and anti-Müllerian hormone
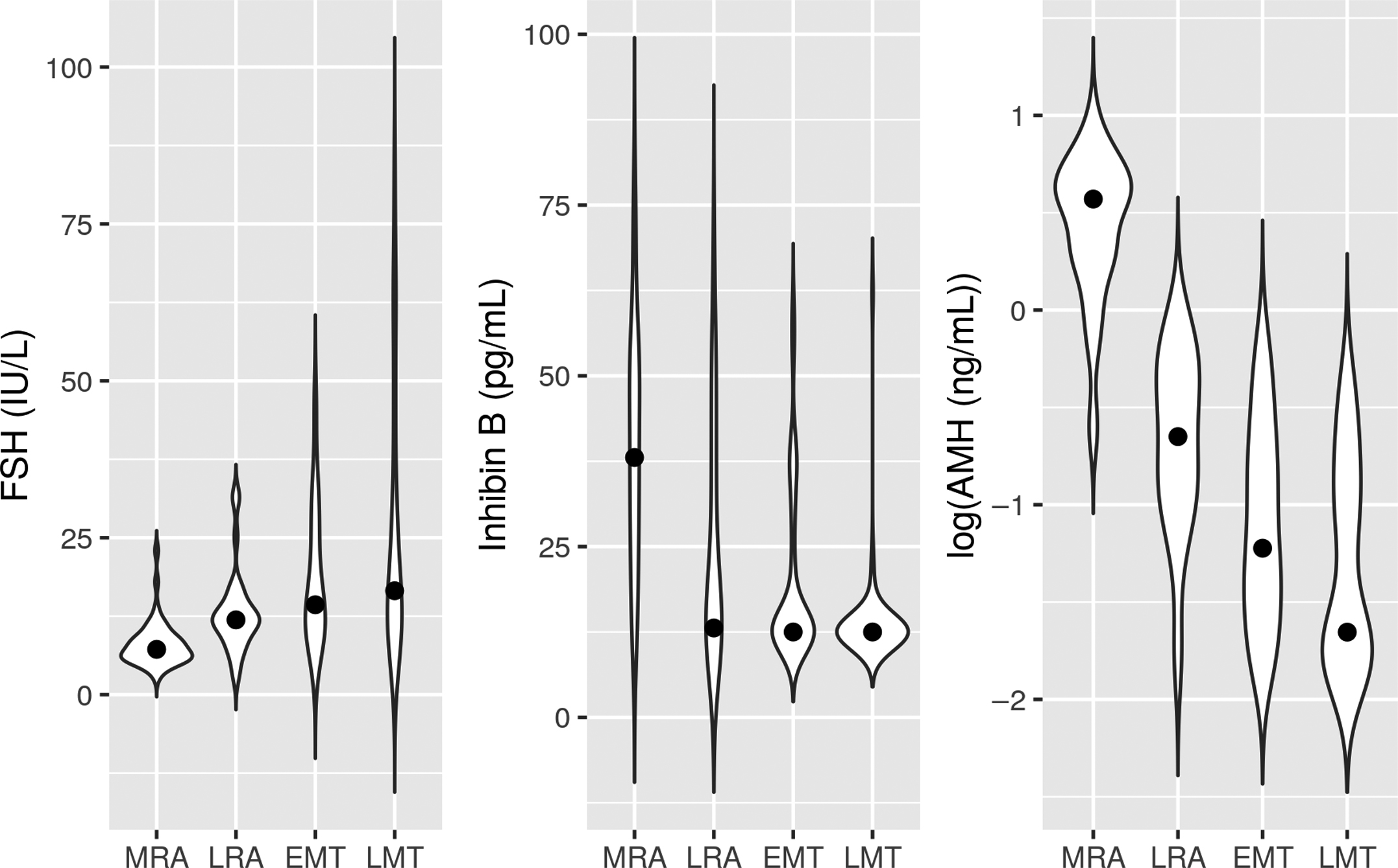
Irrespective of the phase of the ovulatory cycle in which measurements are taken, the gonadotropins, luteinizing hormone (LH), and follicle-stimulating hormone (FSH), rise as women transition from mid-reproductive ages to early and late menopause transition , though it has been observed that LH rises later than FSH when measured in the mid-follicular phase . Correspondingly, both inhibin B, a gonadal glycoprotein that inhibits the expression of the β-subunit of FSH at the level of the pituitary and anti-Müllerian hormone (AMH), a product of granulosa cells, and a marker of ovarian reserve are seen to drop during the same transition, the latter to a much greater degree (see Fig. 18.1 ). Notwithstanding the steep declines seen with aging, defining an AMH threshold indicative of a poor response to fertility interventions has proven challenging and is hampered by differences in available immunoassays .
FSH levels average of 60 IU/L are typical of postmenopausal women but range from 25–135 IU/L showing no overlap with levels seen in the ovulatory phase of fertile women. In contrast, LH levels range from 8 to 60 IU/L but may be eclipsed by levels seen in the ovulatory phase.
Estradiol and progesterone
In the same manner that FSH and LH decline throughout premenopause and menopause, so also estradiol and progesterone are seen to decline in the population overall. However, the menstrual phase hormonal patterns exhibited over the menopausal transition are complicated by marked variability within and between individuals and depend heavily on whether the menstrual cycle is short, long, ovulatory, or anovulatory. The interested reader is directed to studies exploring the overall and individual patterns observed .
Complicating the postmenopausal measurement of estradiol is the technical problem with immunoassay variability and cross-reactivity at low concentrations . This is of particular importance if estradiol is measured to follow breast cancer patients receiving aromatase inhibitors for estrogen receptor–positive disease. Many immunoassays have a functional sensitivity higher than the measurement range of 20–40 pmol/L (5–10 pg/mL) required in this clinical context but, even for immunoassays with adequate sensitivity, significant accuracy problems arise from results that are too high relative to liquid or gas chromatography and tandem mass spectrometry methods . In postmenopausal women, estradiol reference intervals by tandem mass spectrometry are reported to be 7–77 pmol/L (2–21 pg/mL) and <0.62 nmol/L (<0.19 ng/mL) for progesterone .
Sex hormone binding globulin
While sex hormone binding globulin (SHBG) levels in males increase steadily with age , in women SHBG levels decline until menopause and then, surprisingly, increase again after menopause . In both males and females, increases of SHBG with age are correlated to corresponding increases in body mass index and insulin resistance.
Pituitary human chorionic gonadotropin in females
As diagnostic medicine becomes increasingly protocolized with the use of standardized clinical order sets, inadvertent application of diagnostic tests to populations for which they are not intended is becoming commonplace. One of the unintended consequences of this is pregnancy testing in perimenopausal and early postmenopausal women.
Frequently found in this population of women are modest elevations in human chorionic gonadotropin (hCG), which, in a younger woman, might represent early evidence of pregnancy with hCG typically in the range of 5–20 IU/L where normal might be <2–5 IU/L. This finding is quite alarming to clinicians, who most often erroneously interpret it to represent evidence of lab error, pregnancy, or trophoblastic disease. All of these scenarios eventually result in laboratory medicine consultation whereupon steps can be taken to confirm the result through repeat testing on a different analytical platform, linearity studies, and reanalysis after incubation with a heterophile antibody blocking tube. In the majority of cases, the results are confirmed to be correct but importantly, the hCG will not be observed to rise from its original value.
As early as the 1970s there was evidence that hCG was present in the urine of nonpregnant and postmenopausal women and numerous subsequent immunohistochemical studies demonstrated the presence of hCG-immunoreactive substances in the pituitary. Eventually by examining pituitary tissue extracts using gel permeation and immunoaffinity chromatography followed by amino acid analysis and mass spectrometry, it was demonstrated unequivocally that hCG is expressed in the human pituitary. These studies established its tertiary structure, posttranslational modification, and demonstration of its in vitro bioactivity demonstrating that it was similar to hCG found in the urine of pregnant women but differed in its glycosylation, sialylation, and sulfation resulting in bioactivity about half of what is observed in the urine of pregnant women .
While bona fide elevations of hCG due to pregnancy or trophoblastic disease must be considered, false-positive “phantom” hCG due to heterophile antibody interference must also be excluded. Assumption that unexpected elevations of hCG are genuine has led to somewhat notorious inappropriate surgical and medical intervention. Having excluded false-positive hCG and the possibility of malignancy, benign pituitary hCG production associated with menopause is fairly easy to establish. Using retrospective chart review, Gronowski et al. showed that FSH can be used as a screening tool to identify women likely to have pituitary hCG—a level of >45 IU/L showing a 100% sensitivity and 80% specificity . Such a patient should be referred to an endocrinologist or an obstetrician-gynecologist. After the establishment of a compatible history, normal physical examination, and diagnostic imaging studies negative for evidence of hCG-producing neoplasm, these patients can be given a suppression challenge of hormone replacement therapy whereupon hCG can be remeasured . If pituitary in origin, hCG should become undetectable and the matter can be closed. In a recent cohort study, the prevalence of hCG <SPAN role=presentation tabIndex=0 id=MathJax-Element-1-Frame class=MathJax style="POSITION: relative" data-mathml='≥5′>≥5≥5
≥ 5
IU/L in women <SPAN role=presentation tabIndex=0 id=MathJax-Element-2-Frame class=MathJax style="POSITION: relative" data-mathml='≥55′>≥55≥55
≥ 55
years has been found to be about 8% and it was noted that hCG concentrations show neither an obvious age dependence nor a relationship to FSH concentrations . For these reasons, reference intervals of <SPAN role=presentation tabIndex=0 id=MathJax-Element-3-Frame class=MathJax style="POSITION: relative" data-mathml='≤14′>≤14≤14
≤ 14
IU/L for hCG all women <SPAN role=presentation tabIndex=0 id=MathJax-Element-4-Frame class=MathJax style="POSITION: relative" data-mathml='≥55′>≥55≥55
≥ 55
years have been proposed to avoid unnecessary investigation .
Testosterone deficiency in older males
In males, the population median total testosterone (TT) declines steadily from the second decade onward . Cohorts of young males have median TT concentrations of <SPAN role=presentation tabIndex=0 id=MathJax-Element-5-Frame class=MathJax style="POSITION: relative" data-mathml='≃15−25′>≃15−25≃15−25
≃ 15 − 25
nmol/L declining to <SPAN role=presentation tabIndex=0 id=MathJax-Element-6-Frame class=MathJax style="POSITION: relative" data-mathml='≃10−15′>≃10−15≃10−15
≃ 10 − 15
nmol/L by the ninth decade, depending on the analytical methodology employed. Because testosterone is avidly bound by SHBG and loosely bound by albumin, also of interest from the perspective of maintenance of secondary sexual characteristics are free testosterone (FT) and so-called “bioavailable” testosterone (BAT) concentrations (“bioavailable” referring to the sum of testosterone concentrations from the free and albumin-bound compartments) . FT can be calculated, typically using either the equations developed by Vermeulen , Södergard , and others or by means of equilibrium dialysis followed by immunoassay or mass spectrometry. Direct analog methods for FT are no longer recommended . BAT likewise can be calculated or directly measured after selective precipitation of the SHBG-bound testosterone fraction .
Both FT and BAT decline at a greater relative rate than TT due to rises in the SHBG concentration seen with age . There is an unequivocal requirement for age-dependent normal ranges for TT, SHBG, FT, and BAT, irrespective of whether FT and BAT are calculated or measured. Some studies suggest that most of the age-related decline in various testosterone measures is simply a reflection of cumulative, age-related diseases or obesity, which suppress the hypothalamic-pituitary-gonadal axis. When subjects recruited for a testosterone reference interval study are strictly selected based on “optimum” overall health, the decline in testosterone with age is not seen , thus raising a philosophical question as to how a reference interval should be determined for a population where age-related diseases are the norm rather than the exception. Another curious observation relates to the possibility that testosterone levels may be decreasing overall in populations, when comparing men born earlier in the 20th century versus men born in the mid-20th century, suggesting that the commonly reported age-related decrease in testosterone reflects a shift in population biology as opposed to necessarily just a function of human aging .
While the biochemical phenomena observed with normal aging are clear, as alluded to above, the diagnosis of pathological hypogonadism in older males is a more subtle matter due to an overlap of disease symptomatology with the findings of normal aging such as depression, decreased motivation and initiative, increasing body mass index, and decreased muscle mass and physical strength . Additionally, some disease states associated with increasing age, such as diabetes mellitus, have symptoms often associated with hypogonadism (e.g., erectile dysfunction) .
The decision to treat males experiencing symptoms suggestive of testosterone deficiency with exogenous testosterone is not based solely on TT, FT, or BAT levels but on (1) a clinical presentation consistent with hypogonadism; (2) the exclusion of secondary or reversible causes such as pituitary tumors, diabetes and metabolic syndrome, and hemochromatosis; (3) compatible biochemical findings .
While a full discussion of hypogonadism in the older adult male is beyond the scope of this chapter, if there is a clinical presentation compatible with testosterone deficiency (of any cause), TT is the recommended initial biochemical screening tool for further investigation. If the testosterone is equivocal (i.e., borderline-low), FT or BAT is recommended to clarify the TT result. Once a biochemical evidence of testosterone deficiency is established, ancillary testing with FSH, LH, prolactin, SHBG, thyroid-stimulating hormone (TSH), and ferritin is useful in establishing whether the cause is testicular (hypergonadotropic) or hypothalamic/pituitary (hypogonadotropic) in origin . Multiple clinical guidelines exist but are hampered by ongoing uncertainty in the clinical definitions of disease and the wide (but improving) variation in performance of testosterone assays.
Declines in dehydroepiandrosterone its sulfate ester
In both males and females, the Δ 5 steroid synthetic pathway [proceeding from pregnenolone and 17- α -hydroxypregnenolone leading to dehydroepiandrosterone (DHEA)] shows much more pronounced age-related decline than the Δ 4 synthetic pathway (proceeding from progesterone and 17-hydroxyprogesterone to produce glucocorticoids/mineralocorticoids). Both the DHEA and its sulfate (DHEA-S), which come from the Δ 5 pathway, show far less sex-dependent concentration differences than testosterone and are seen to decline in both sexes after age 20 years to levels of approximately 20% of their peak values in men and 30% of their peak values in women by the eighth decade of life . DHEA is converted to DHEA-S by hydroxysteroid sulfatases expressed in the adrenal cortex, liver, and small intestine and the massive adrenal production of DHEA-S makes it the most abundant circulating human steroid . In women, DHEA-S is produced nearly exclusively by the adrenal gland while in men, 5% of circulating DHEA-S is of testicular rather than adrenal origin. Because DHEA and DHEA-S are so strongly associated with the adrenal function, their decline is said to reflect “adrenopause.”
The nature of the observed age-related changes is unknown and the clinical consequences of the declines in DHEA and DHEA-S are not entirely certain but there has been substantial interest in the supplementation of DHEA to prevent or reverse the effects of aging—cognitive, musculoskeletal, metabolic, cardiovascular, and immunological . However, supplementation of DHEA in older men is likely only beneficial to body composition via its androgenic effects , which is perhaps unsurprising. Evidence for the benefit of DHEA supplementation to women with both adrenal insufficiency and normal adrenal function is uncompelling and long-term safety unknown.
From a diagnostic standpoint therefore, DHEA and DHEA-S certainly require age-dependent reference intervals. However, while DHEA and DHEA-S testing have a number of applications in the young, particularly for the investigation of hirsutism, the clinical need for DHEA and DHEA-S measures in older individuals is more or less confined to the investigation of possible adrenal carcinoma.
Hypothalamic-pituitary-somatotropic axis
Growth hormone
There is substantial evidence that the continued supplementation of growth hormone (GH) is of benefit to adult individuals who were born with congenital GH deficiency or who have acquired GH deficiency through an insult to the pituitary gland (i.e., trauma, tumor, infiltration, or irradiation). This situation does not pose a diagnostic challenge in the aging population. On the other hand, isolated adult-onset idiopathic GH deficiency is a very rare condition and its diagnosis and management are nuanced . Despite its rarity, the possibility of this diagnosis may be raised if an isolated insulin-like growth factor 1 (IGF-1) measurement is found to be low, even when the inciting motivation for testing was the possibility of acromegaly.
Many of the clinical findings of GH deficiency can be seen in with normal aging: obesity, sarcopenia, dysthymia, and dyslipidemia. Also important is the observation that sarcopenia, the major feature of elderly frailty, is associated with lower IGF-1 levels in males, whether accompanied by obesity or not . Further, it is established that GH supplementation of GH deficient adults improves lean body composition, improves lipid profiles, decreases carotid intima-media thickness, leads to a better sense of well-being , and leads to increases in bone mineral density , cardiac stroke volume, and glomerular filtration rate . These observations have encouraged the concept of “somatopause” among patients without established GH deficiency and have led some to treat these patients with recombinant GH as an “antiaging” strategy despite the lack of evidence for this practice .
Insulin-like growth factor 1
Because the magnitude and frequency of GH pulses decrease with normal aging , IGF-1 shows corresponding decline with age and the establishment of age-dependent reference intervals for IGF-1 is an absolute requirement for offering this test in a diagnostic laboratory.
Reference interval studies for IGF-1 in the adult population require large numbers of both male and female subjects because of both age dependence and sex dependence. These exist for all of the most popular automated IGF-1 methods, namely, the Siemens Immulite ( n =1499 subjects), the DiaSorin LIAISON ( n =1606 subjects), the Immunodiagnostic Systems ISYS ( n =15,014 subjects) , and the Roche Elecsys ( n =6698 subjects) .
Unfortunately, there is an additional problem of intermethod bias attributable to both methodological differences and traceability to different generations of the WHO/NIBSC standard reference materials (WHO IRR 87/518 purified vs WHO 02/254 recombinant) meaning that the reference intervals are method-dependent . There is some evidence that mass spectrometric (MS) methods may assist in methodological standardization and it should also be noted that high-resolution MS methods permit the identification and measurement of a fairly common IGF-1 polymorphism of indeterminate significance (A70T). The A70T polymorphism is not detected by at least one automated commercial IGF-1 method that therefore generates IGF-1 results of half their true value in heterozygotes .
Several statistical methodologies for the fitting of continuous reference intervals are available and these are far preferable to placing IGF-1 reference interval results into decade-wide bins (or other convenient n -year bins) because of the large steps induced in the reference interval when the patient passes from one age bin to the next.
IGF-1 measurement alone is not recommended for the diagnosis of isolated GH deficiency in adults but provocative testing with either the insulin tolerance test or with GH releasing hormone (where available) is recommended. While there is physiological basis to assume that age-related or body mass index thresholds for adequate GH stimulation would be reasonable, at present evidence for using such cutoffs is inadequate and generic GH thresholds for all adults are used to establish GH deficiency .
Hypothalamic-pituitary-adrenal axis
It is reported that there are a number of age-dependent physiological phenomena related to the hypothalamic-pituitary-adrenocortical axis—specifically involving responsiveness of the adrenal gland to hypothalamic/pituitary stimulation and, in turn, of the hypothalamus and pituitary to the negative feedback of the adrenal .
Plasma total cortisol concentrations themselves show only modest age dependence that is more significant in females than males. In males, the subtlety of age-related trends accounts for the fact that some studies observe no change or perhaps a modest increase or decline . The largest and most recent reference interval study ( n =4678 subjects) examining the morning concentrations of nine steroids across the human life span using MS did not show compelling trends in adult cortisol concentrations except perhaps a slight increase with age and for females, a notable decrease in the upper limit of normal with each 20-year age bin —possibly tied to decreases in binding cortisol globulin concentrations associated with decreased estradiol concentrations. In any case, there is some evidence for the use of age-dependent reference intervals for morning total cortisol concentration.
Dexamethasone suppression
It has been observed that after an overnight dexamethasone suppression that basal cortisol levels are higher in the older patients and that both adrenocorticotropic hormone (ACTH)- and cortisol-responses to corticotropin releasing hormone (CRH) stimulation are also higher . Similar observations have been made in other studies. For example, a modest but statistically significant trend was observed between log-transformed cortisol levels and subject age after low-dose (1 mg) dexamethasone in a cohort of 33 healthy individuals aged 51–96 years . It has also been suggested, based on isolated observations ( n =3 individuals >50 years) in a study of 60 healthy volunteers, that older subjects may have inadequate dexamethasone concentrations after a low-dose challenge . While a number of patient factors could account for this finding, the authors concluded that measurement dexamethasone levels should be considered in older individuals to confirm an 8 a.m. concentration of at least 5.6 nmol/L (220 ng/dL), the concentration required to achieve cortisol suppression .
This finding is subject to caveats related to the population observed and the means by which suppression is defined. For example, as summarized in a metaanalysis of age-related effects on hypothalamic-pituitary-adrenal (HPA) responses to stimulation and suppression challenges , age-related differences in the proportion of individuals achieving suppression (defined as cortisol <140 nmol/L or 5 μg/dL) may be absent, though increases in the mean cortisol response are seen with aging. Similar observations have been made in other studies of depressed individuals but not those with adrenal incidentaloma .
Twenty-four-hour urinary cortisol and salivary cortisol
There appears to be less information available for the effect of aging on 24 h urinary cortisol excretion. An older reference interval study using high performance liquid chromatography found a gradual decline with age and, surprisingly, no differences between sexes but more recent studies using both immunoassay and MS found males to have higher cortisol excretion but reported no trends with age. In the context of depression, studies of the effect of age on 24 h urinary free cortisol are either unconvincing or show no changes with age in a study of depressed individuals in both cases or controls .
Salivary cortisol
While some studies have observed higher salivary cortisol levels in older age groups of healthy subjects , others have not . Nevertheless, it has been concluded that there is inadequate evidence to support the use of age-dependent cutoffs for late-night salivary cortisol .
Conclusions on screening for Cushing’s syndrome
From a practical standpoint, age-related effects in diagnostic tests used to screen for Cushing’s syndrome are inconsistent and incompletely characterized and there is currently no recommendation from the Endocrine Society for age-specific cutoffs for any of the three screening tools for Cushing’s syndrome: dexamethasone suppression, 24 h urinary cortisol, or midnight salivary cortisol .
Adrenocorticotropic hormone stimulation
The 24 h cortisol secretion in response to ACTH stimulation has been observed to decrease with age in men and increase with age in women . However, a metaanalysis of the effect of gender on cortisol responses to various stimuli (pharmacological, hormonal, psychosocial) indicated that both sexes have increased responses but that the effect of age on cortisol secretion is almost threefold higher in women .
There is evidence of diminished cortisol-mediated feedback suppression of ACTH secretion with advancing age and that effect is more pronounced in women than men . This reduced glucocorticoid-mediated feedback on ACTH concentrations has been hypothesized to be reflective of generalized diminished HPA responsiveness to negative feedback signals that would normally lead to termination of the response to the instigating stimulus. The same mechanism thought to be the cause of the prolonged cortisol response to stimulation seen with aging . In contrast, it is important to note that cortisol responses to ACTH in the critically ill elderly are smaller than younger critically ill patients .
While these observations are fairly consistent among studies, there is no specific recommendation for age-specific cortisol cutoffs for ACTH-stimulation tests used for the diagnosis of adrenal insufficiency .
Hypothalamic-pituitary-thyroidal axis
Thyroid function tests are among the most commonly ordered biochemistries in medicine; true thyroid dysfunction (of varying degrees of severity) is common, especially in older adults and may associate with a lengthy list of potential symptoms, most noticeably, fatigue. For the aged in particular, patients with true thyroid dysfunction often have far more subtle clinical presentations or undifferentiated symptoms compared to younger patients with classical hypo- or hyperthyroidism . For this reason, interpretation of thyroid function testing becomes one of the most frequent challenges in both clinical and laboratory medicine.
With the development of third-generation TSH assays and easy access to free thyroxine and triiodothyronine measurements, a new problem has arisen in thyroidology: the need to differentiate the categories of (1) normal changes of the thyroid function with age, (2) subtle variations from normal of no clinical significance, and (3) true thyroid disease requiring intervention. Frequently thyroid function testing is ordered without a particularly strong clinical indication meaning that incidental and/or nonspecific biochemical abnormalities in thyroid function are common. It is natural for clinicians to worry about even minor abnormalities that have been uncovered, as they may portend future overt thyroid dysfunction that can have serious medical consequences.
Mild abnormalities: normal aging or disease?
At least two prior large-scale studies of thyroid function have suggested that there is a different distribution of TSH among older people (age 70+ years) with an upper reference limit approximately 13% higher than in younger persons. Such studies take pains to exclude subjects with clinical or biochemical evidence of thyroid dysfunction but are open to criticism on the basis of specific ethnicity of subjects, geographic location/iodine status, and possible healthy survivor bias. While a 13% upward shift of a true physiologic range might appear numerically small, clinicians tend to offer “treatment” to many/most patients with TSH values outside the reference interval; irrespective of clinical findings, this represents a very large number of clinical interventions that should not be assumed to be benign.
The difficulty lies in determining the line that separates “health” from “disease” (both clinically and biochemically) and because this distinction will necessarily encompass an asymptomatic subcohort, researchers have relied upon population studies attempting to correlate more clearly defined disease processes with various levels of thyroid test abnormalities, including substrata of thyroid function tests within the reference interval. Given the association between subclinical hypothyroidism (SCH) and cholesterol metabolism/hyperlipidemia , cardio- and cerebrovascular diseases have long been a potential interest for outcome studies. Thus far, such studies have yielded mixed results with some demonstrating a link to higher rates of cardiovascular disease (CVD) and cardiovascular mortality , though this has not been a consistent finding . Symptom checklist studies in persons with subtle biochemical abnormalities of lower thyroid levels show either no clear symptoms or a broad range of nonspecific findings .
At the other end of the spectrum of subtle dysfunction, namely subclinical hyperthyroidism, there is a well-established link, in elderly persons, to increased rates of cardiac arrhythmia , CVD , and future in-patient mortality , even with marginally abnormal biochemical indices of hyperfunction . Again extrapolating from the manifestations of clinically overt thyroid disease, population studies have suggested a possible association of slightly higher thyroid levels with bone loss and fracture , cognitive dysfunction , and mood disorders .
Against these association studies stands opposing evidence from both population health and intervention trials. Several studies have even suggested that higher TSH measures may confer survival benefit , even in the very elderly , although it is unclear whether this is a biologically protective effect or an epiphenomenon. Multiple prospective, blinded intervention studies for SCH have been reported but have uniformly failed to demonstrate reduced rates of cardiovascular disease or symptomatic improvements . This observation is strengthened by a study showing that “fine-tuning” thyroid hormone replacement in response to subtle biochemical abnormalities in patients with existing hypothyroidism also fails to improve symptoms or quality of life . Thyroid hormone treatments are harmful if accidentally used to excess and may move a patient from a position of uncertain harm (SCH) to a position of probable harm (subclinical or overt hyperthyroidism) .
Despite the stronger associations between adverse disease outcomes and endogenous subclinical hyperthyroidism, there are still no convincing studies proving a benefit to treatment (e.g., with antithyroid drugs) on any clinical outcome beyond surrogate measures such as bone density.
Paradoxes and presumed benefits
The conundrum facing the clinician who has a patient showing subtle thyroid-function abnormalities (usually marginally high or low TSH) should now be evident. An argument can be made that slightly high TSH results would be normal were the reference interval appropriately age-adjusted, which it frequently is not. However, even if the clinician could be convinced that the TSH was abnormal after age-adjustment of the reference interval, one might appeal to a possible survival benefit associated with nontreatment of such an individual. While placebo-controlled studies tend to show no benefit to treatment, patients themselves tend to report a benefit with treatment. This phenomenon makes it challenging for clinicians to rely on their personal experience to guide them in managing these patients. And yet, the association of SCH with hyperlipidemia and possible CVD continues to beg for further study to see whether the SCH population may be better understood in case there are some subgroups who may indeed benefit from thyroid replacement. Until then, the clinical interpretation of slightly high TSH in the aged patient remains a paradox.
Overt thyroid dysfunction
Overt thyroid dysfunction is usually characterized by undetectable TSH with overtly high free T4/T3 in the case of hyperthyroidism or markedly elevated TSH with overtly low free T4 in the case of hypothyroidism. The natural history of these overt disease states is poorly studied on account of the fact that such cases cannot knowingly be left untreated. However, severe hyperthyroidism (thyroid storm) and severe hypothyroidism (myxedema coma) may present with atypical (often called “apathetic”) clinical features in the elderly yet come with a very high associated short-term mortality . Myxedema coma may be particularly dangerous in the elderly given its usual slow onset and overlap with progressive cognitive decline. Myxedema coma is also more prevalent in the elderly given the higher risk for things like unintentional medication (thyroxine) omission or tendency to develop instigating events such as sepsis or congestive heart failure . Diagnosis of even overt thyroid dysfunction in the acute care setting may be particularly difficult in the sick patient due to overlap with the biochemical indices seen in the nonthyroidal-illness syndrome, which may be mistaken for either hyper- or hypothyroidism depending on the tests ordered and the stage of recovery at which they are ordered.
The effect of comorbidities
In addition to the above considerations, elderly patients often have coexisting conditions that may influence either the presentation or diagnosis of thyroid disease, with examples in Table 18.1 . Pituitary insufficiency (secondary hypothyroidism) may be a common confounding factor in the elderly, particularly given the link to intracranial disease processes affecting pituitary function or simple age-related pituitary insufficiency leading to rather unimpressive rises in TSH even in the face of profound thyroid gland hypofunction .