Cutaneous T-cell and NK-cell lymphomas
Mycosis fungoides
MF variants and subtypes
Folliculotropic MF
Pagetoid reticulosis
Granulomatous slack skin
Sézary syndrome
Adult T-cell leukaemia/lymphoma
Primary cutaneous CD30+ lymphoproliferative disorders
Primary cutaneous anaplastic large cell lymphoma
Lymphomatoid papulosis
Subcutaneous panniculitis-like T-cell lymphoma
Extranodal NK/T-cell lymphoma, nasal type
Primary cutaneous peripheral T-cell lymphoma, unspecified
Primary cutaneous aggressive epidermotropic CD8+ T-cell lymphoma (provisional)
Cutaneous γ/δ T-cell lymphoma (provisional)
Primary cutaneous CD4+ small/medium-sized pleomorphic T-cell lymphoma (provisional)
Cutaneous B-cell lymphomas
Primary cutaneous marginal zone B-cell lymphoma
Primary cutaneous follicle centre lymphoma
Primary cutaneous diffuse large B-cell lymphoma, leg type
Primary cutaneous diffuse large B-cell lymphoma, other
Intravascular large B-cell lymphoma
Precursor hematologic neoplasm
CD4+/CD56+ hematodermic neoplasm (blastic NK-cell lymphoma)
Several guidelines to help clinicians to treat PCL have been published [3–7]. However, due to the rarity and heterogeneity of PCL, randomised clinical trials are usually lacking (with few exceptions) and levels of evidence are usually low.
Given that PCL can be easily reached, skin-directed treatments (alone or in combination with systemic agents) are frequently used (phototherapy, photochemotherapy, radiotherapy, topical treatments or intralesional infusion of several drugs). Skin-directed therapies are out of the scope of this chapter and will be treated elsewhere.
The choice of treatment will depend on the type of PCL and the stage of the disease. Some of our cases will need systemic approach from the beginning, and others will not be treated systemically, almost never.
Primary Cutaneous T-Cell Lymphomas
Mycosis Fungoides and Variants
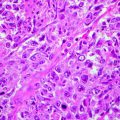
Mycosis fungoides (MF) is the most common primary cutaneous T-cell lymphoma, encompassing around 50 % of all PCLs. It characteristically evolves in patch, plaque and tumour stages and eventually can affect lymph nodes, peripheral blood and viscera. It is produced by proliferation of epidermotropic small to medium-sized T cells with cerebriform nuclei. Most of them are CD4+.
Before treating MF, doctors should have in mind that most cases have an indolent behaviour. Median survival of MF (in global) is not reached after more than 20 years. If we consider MF stages, in early MF (stages Ia–IIa), stage Ia MF does not have impact in survival; in stages Ib and IIa, 10-years survival is >90 % and around 80 %, respectively. In advanced MF, stages IIb–IVb, median disease-specific survival is reached in around 7 years for stage IIb, around 4 years for stages III and IVa1, around 3 years for stage IVa2 and around 2 years for stage IVb [8, 9] (Table 29.2).
Table 29.2
Staging of mycosis fungoides
Ia: Patches/plaques covering <10 % body surface area |
Ib: Patches/plaques covering ≥10 % body surface area |
IIa: Patches or plaques, any surface + palpable, nonspecific lymph nodes |
IIb: Tumoural stage |
IIIa: Erythrodermic without peripheral blood involvement |
IIIb: Erythrodermic with light peripheral blood involvement |
IVa1: Any skin involvement with severe peripheral blood involvement |
IVa2: Any skin involvement with lymph nodes infiltration |
IVb: Any skin involvement with visceral involvement |
On the other hand, to date, no treatment has demonstrated to be able to modify natural history of the disease, and no treatment has been able to cure MF (except probably radiotherapy in unilesional MF).
So, our main interest should not be to cure MF but to increase quality of life (QoL), to achieve and maintain complete response, if possible, and to produce minimal toxicities during and after treatment.
Three MF variants are considered, based on their outcome, different from classical MF. Pagetoid reticulosis is characterised by the presence of localised patches or plaques with an intraepidermal proliferation of neoplastic T cells. The neoplastic T cells are CD3+ and may have either a CD4+ or CD8+. Prognosis is excellent and almost never need systemic therapies [1].
Follicular MF is characterised by the presence of folliculotropic or syringotropic infiltrates, often sparing the epidermis. Most cases show follicular mucinous degeneration. Lesions are frequently located on the head and neck area. Prognosis of follicular MF is worst than classical MF. Perifollicular location of the infiltrates renders them frequently less responsive to skin-directed therapies. So, systemic treatments will be used earlier in follicular MF than in classical MF.
Granulomatous slack skin (GSS) is characterised by the development of folds of lax skin, mostly on the axillae or inguinal groins. Histology shows a granulomatous infiltrate with elastophagocytosis and clonal T cells. Usually GSS has a very indolent behaviour.
Immunomodulators
Cytokines
IFNα
Interferons (IFNs) are cytokines that exhibit pleiotropic cellular effects, including antiviral, immunomodulatory, antiproliferative and proapoptotic effects [10, 11].
IFNα is indicated (alone or in combination) in early MF as a second-line treatment and in advanced MF as first-line treatment.
IFNα has been used subcutaneously in monotherapy at doses between 3 and 36 MU, 3 times a week. As high doses have much more adverse events and do not provide clearly better responses, usually low to intermediate doses (3–9 MU) are preferred.
In monotherapy, overall response rate (ORR) is around 88 % for early MF and 66 % for advanced MF. Between 10 and 35 % of patients achieve complete response. Intralesional IFNα is used in tumoural lesions, combining systemic effect with very high local doses.
Time to response is 8–12 weeks (some patients need >6 months to respond) and mean duration of response is between 30 and 40 months [12, 13].
Most common adverse events are fatigue, anorexia and a flu-like syndrome, more intense at the beginning of treatment. Usually it is well controlled with acetaminophen but occasionally is dose limiting. Leukopenia, thrombopenia and hypertransaminasemia are common too. Thyroid function should be monitored. Long-term users can develop depression [12–14].
IFNα is frequently used in combination with PUVA, retinoids, rexinoids or extracorporeal photopheresis.
Combination with PUVA seems to increase RR of PUVA with a 90–100 % ORR and 62–84 % CRs [15–18]. Stadler et al. [19] conducted a randomised clinical trial comparing PUVA alone vs. PUVA + IFNα. They reported that the combination was able to save UVA irradiation and to increase duration or response vs. PUVA alone.
Combination of IFNα with etretinate or acitretin should not be recommended because it produces similar response rates to IFN alone [20] and worst results than combination IFN + PUVA [21].
Other cytokines have been used to treat MF, trying to reverse the TH1/TH2 imbalance typical of the disease. Experience with IFNγ is much more limited and efficacy seems to be lower than IFNα. Response rates of 30 % without CRs have been reported in a phase II study with 16 patients. Duration of response was 10 months [22].
A phase II clinical trial with interleukin 12 (IL12) in early MF with 23 cases reported 43 % of RR (lasting 3 to >45 weeks) without CRs. Main toxicity was asthenia, headache, fatigue, chills, arthralgia, myalgia and increasing of GOT and GPT [23].
Results with IL2 have been poor, with 18 % of RR without CRs in a phase II clinical trial including 22 heavily pretreated MFs [24].
Retinoids/Rexinoids
Retinoids are derivatives of vitamin A that inhibit proliferation and induce differentiation in different tumours. In MF, etretinate, its metabolite acitretin and mostly bexarotene have been used.
Combined treatment of acitretin + PUVA achieves the same response of PUVA alone (73 % vs. 72 % CRs, respectively), but the cumulative dose of PUVA to achieve CR was lower in the combined treatment group [25]. Combination is recommended as second-line therapy in MF stages Ia to IIa and as first line for MF IIb or III [4].
Bexarotene (Bxt) is a rexinoid (specific agonist of RXR receptors). Bxt has multiple activities (blocks tumour growth, induces apoptosis, blocks NFKB, modifies microenvironment, etc.). Oral Bxt has been approved by FDA for resistant, recurrent MF (EMEA label includes “advanced”).
It is recommended to start with 150 mg/m2 and increase to 300 mg/m2, if possible.
In monotherapy, response rates in refractory early MF are 54 %, with 7 % of CRs. Median time to response is about 8 weeks. Response rates in refractory advanced MF are 45 % with 2 % of CRs. Median time to response is >20 weeks [26, 27].
Most common adverse event is hypertriglyceridemia appearing between 80 and 100 % of cases. It is the most dose-limiting toxicity of Bxt. It usually starts 1–2 days after beginning and disappears 2–4 days after withdrawal of bexarotene. Second most common AE is central hypothyroidism, appearing between 70 and 80 % of cases. It starts and disappears 2–4 days after beginning and withdrawal of Bxt, respectively.
Other adverse events appearing in >20 % of cases are neutropenia (usually late), skin peeling, leukopenia, elevated LDH, headache and hypercholesterolemia. Very importantly, it does not produce photosensitivity, allowing combination with PUVA.
It is recommended to normalise serum lipids and thyroid function before starting Bxt. One or two hypolipidemic agents should be introduced one week before Bxt (fenofibrate ± statin are the most usual). Gemfibrozil is contraindicated because it produces paradoxical hypertriglyceridemia when combined with Bxt.
Most authors recommend to associate thyroid hormone replacement from the beginning (50μg/day) but is not always needed.
Blood tests should include lipid profile, free T4 (not TSH), muscle enzymes (to detect early myopathy induced by hypolipidemics) and pancreatic enzymes (to detect pancreatitis) and should be performed periodically, starting 1 week before and at 7, 14 and 28 days time points; after that, monthly [28, 29].
Bxt can be combined with different therapies as PUVA, IFN, extracorporeal photopheresis or denileukin diftitox.
Different series reporting combination of PUVA + Bxt have been published. In global, response rates vary from 60 to 78 % depending on the dosage of Bxt [30, 31]. A randomised clinical trial with PUVA + two different doses of Bxt (150 vs. 300 mg/day) (MILL-61896) did not find differences in response rate. Interestingly, patients included in the trial seemed to need less UVA irradiation than historical doses needed in the centre that performed the study [32]. The EORTC CLTF has finished a randomised clinical trial (EORTC 21011) comparing Bxt+PUVA vs. Bxt alone. The study was underpowered but no significant differences in response rate or response duration was observed. There was a trend towards fewer PUVA sessions and lower UVA dose required to achieve CCR in the combination arm (PUVA + bexarotene) [3, 19, 30, 80].
Extracorporeal Photopheresis (ECP)
ECP is an immunomodulatory therapy involving leukapheresis. Lymphocytes are treated ex vivo with 8-methoxypsoralen + UVA irradiation and reinfused to the patient. First reported in 1987 [35], it was approved by FDA 1 year later for treatment of CTCL. More than 1,000 patients have been published with CTCL treated with ECP. RRs of 43–100 % and CRs from 0 to 62 % have been reported. Recently, UK consensus on the use of ECP has been published [36].
Mechanism of action is not well understood, but clinical and laboratory findings support the hypothesis of a vaccination-like effect. It seems that malignant T lymphocytes suffer cell cycle stop and apoptosis. After that, phagocytosis, antigen presentation and elicitation of specific immune responses mediated through cytotoxic T lymphocytes with antitumour specificity would occur.
ECP should be restricted to erythrodermic CTCL, either stage III or IVa demonstrating a peripheral blood involvement with T-cell clone and/or circulating Sézary cells >10 % and/or CD4/CD8 ratio >10. Patch/plaque or tumoural stages are not suitable for ECP. Treatment of stage IVb or erythrodermic patients without peripheral blood involvement is not recommended following UK consensus, but there are some publications reporting response in some of these patients. Patients with very high tumour burden in peripheral blood respond poorly and should be considered for combination (e.g. alemtuzumab) or alternative treatments.
Schedule includes 1–2 cycles per month (two procedures performed on two consecutive days per cycle).
Adverse events are rare. Venous access can originate infections.
UK consensus recommends maintaining treatment for at least 6 months. If no response is achieved, combination with other drugs (Bxt, IFN or multiple combinations are frequently used) [37–39] is done for three additional months. If no response, treatment should be stopped. International guidelines are under preparation (several workshops held to date in Minden and Lisbon) that probably could modify these recommendations. ECP treatment is recommended early as patients become more immunosuppressed with time.
Median time to maximum response is 10 months. Patients achieving response should be maintained with the same schedule and eventually reduce frequency (every 6–12 weeks) before stopping. Median time to treatment failure is 18 months.
Transimmunisation is a modification of ECP consisting in incubating overnight at body temperature the buffy coat after photoactivation. This allows co-incubation of the apoptotic malignant T cells with the newly formed antigen-presenting cells prior to reinfusion [40].
Monoclonal Antibodies
Denileukin diftitox (Ontak™, Onzar™), DAB389–IL-2, is a recombinant fusion protein that selectively binds high-affinity IL-2 receptor (CD25). The molecule consists of sequences for the enzymatically active domain of diphtheria toxin and the IL2. After joining receptor, DAB389-IL2 is internalised in the cell, diphtheria toxin is released and protein synthesis is blocked, resulting in cell death.
Denileukin diftitox was approved by FDA in 1999 (not by EMEA) for resistant, recurrent MF expressing IL2. Dose schedule is 18 mcg/kg/day by IV infusion once daily for 5 days every 3 weeks for up to 8 cycles.
Phase III clinical trials [41, 42] including patients with stages Ib-IVa and at least 20 % of cells expressing IL2 have reported RRs between 30 and 49 % with 10 % of CRs. Median time to response is 3–4 months and median duration of response is 6.9 months.
Most common adverse events are fever, myalgia, chills, nausea and vomiting and a mild increase in transaminase levels. Acute hypersensitivity occurs in 60 %, always in the first 24 h and during the initial infusion. Vascular leak syndrome (hypotension, hypoalbuminaemia and oedema) occurs in 25 % of cases within the first 14 days of a given dose. Myelosuppression is very rare. Adverse events drop and response rates increase to 60 % if patients are pretreated with corticosteroids [43].
Response rate is higher in CD25+ MF cases. Different papers have reported 30–78 % of response in cases with >20 % of cells expressing CD25 and 20–30 % in cases with low CD25 expression. However, a recent review considering only patients achieving CR with denileukin diftitox did not find differences between CD25 +ve and −ve cases. More than 36 % of patients relapsing after a first course of denileukin diftitox treatment respond again to this drug [44–46].
Combination of denileukin diftitox with bexarotene is based on the rationale that Bxt can induce expression of IL2 on malignant T cells. A phase I clinical trial combining Ontak + Bxt reported 67 % of RR [47].
Alemtuzumab (Campath™) is a humanised monoclonal antibody that targets CD52. CD52 is found in normal and malignant B and T cells. Granulocytes, macrophages or thrombocytes do not express CD52. Alemtuzumab is usually administered at a dose of 30 mg intravenously three times per week, for up to 12 weeks.
A phase II clinical trial [48] with 22 patients with heavily pretreated MF or SS patients reported an ORR of 55 % with 32 % of CRs. Sézary cells were cleared from the blood in 6 of 7 (86 %) patients, and CR in lymph nodes was observed in 6 of 11 (55 %) patients. The effect was better on erythroderma (OR, 69 %) than on plaque or skin tumours (OR, 40 %) and in patients who had received 1 to 2 previous regimens (OR, 80 %) than in those who had received 3 or more prior regimens (OR, 33 %). Time to treatment failure was 12 months.
The main problem with alemtuzumab is the severe immunosuppression produced, with high-risk viral, bacterial and fungal infectious complications that may be life-threatening [49].
Patients should be monitored for CMV reactivation using periodically PCR studies every 2–3 weeks. If viremia is increasing, ganciclovir should be recommended. On the other hand, acyclovir and sulfamethoxazole trimethoprim to prevent herpes virus and Pneumocystis carinii pneumonia should be given to patients. Mantoux test with booster and chest X-ray to detect latent infection by Mycobacterium tuberculosis should be performed. Active or latent hepatitis B or C infections should be treated before using alemtuzumab. Serology for Strongyloides is recommended for patients living in endemic areas.
Recently, a new approach with low subcutaneous dose (10 mg s.c. eod) has been reported with very good results (14 patients, 3 CRs and 9 PRs) and very importantly, without infectious complications [50].
Finally, patients should have cardiac monitorisation. In a series of patients treated with standard IV dose, 4 of 8 patients with no prior history of cardiac problems developed significant cardiac toxicity (congestive heart failure or arrhythmia) that mostly improved after alemtuzumab discontinuation [51].
Other monoclonal antibodies are under investigation.
Zanolimumab is a fully human anti-CD4 antibody directed against CD4 molecules on surface of T cells. There are 2 phase II clinical trials finished, including 47 patients [52]. Patients were initially treated with intravenous zanolimumab at a dose of 280 mg/week, which was increased to 560 mg/week in early-stage patients and 980 mg/week in patients with advanced disease. In MF, RRs were low in the low dose (15 %) vs. high dose (56 % of RR with 2 CRs and 10 PRs). In SS, RR was only 22 % with high dose, showing a greater efficacy of zanolimumab in MF compared to SS.
In the high-dose arm, median time to response was less than 8 weeks and median response duration, 81 weeks. Most frequent adverse events are eczematous dermatitis, low-grade infections, flu-like symptoms and asthenia. Zanolimumab produces a very prolonged CD4 reduction, lasting even >24 months. There is an ongoing pivotal phase III clinical trial comparing 3 dose levels (4 vs. 8 vs. 14 mg/kg). The first two doses were stopped because of low RRs. Trial was stopped in Europe but is ongoing in the USA.
Recombinant CD3 immunotoxin (A-dmDT(390)-bisFv(UCHT1)) is composed of the catalytic and translocation domains of diphtheria toxin fused to two single-chain Fv fragments of an anti-CD3 epsilon monoclonal antibody. The drug was administered to 5 MF patients. Two of them had PR lasting 1 and >6 months [53].
SGN30 and a more active drug (SGN35, brentuximab vedotin (BV)) are anti CD30 monoclonal antibodies. Brentuximab vedotin is a chimeric protein targeting CD30 on cell surface. The molecule is conjugated with monomethyl auristatin E (MMAE), a microtubule disruptor. After joining receptor, MMAE is internalized and blocks mitosis. In two different trials recently reported, ORR is between 40 and 68 % depending on the level of CD30 expression. Time to response was 6-10.5 weeks. Most frequent adverse events are peripheral neuropathy, rash, fatigue and diarrhea. Neutropenia can be severe [54, 96, 97].
Mogamulizumab (KW-061), a humanized, defucosilated monoclonal antibody targeting CCR4 produces antibody dependent cellular cytotoxicity. ORR in a recent phase II clinical trial was 37 % (29 % in mycosis fungoides, 47 % in Sézary syndrome).
Inhibitors of Histone Deacetylases (HDACi)
HDACi are a new group of compounds involved in the balance of acetylation/deacetylation of proteins within the cell. Histones are the main proteic component of the chromatin. Its main function is to allow DNA strand to roll around and form nucleosomes. Protein queues of histones can suffer different chemical modifications (phosphorylation, methylation, acetylation, etc.). Depending on the level of histone acetylation, chromatin has a more or less relaxed or packed disposition. Relaxed chromatin allows gene expression, while packed chromatin does not. HDACi produce histone hyperacetylation, chromatin has a more relaxed disposition, and cells modify their behaviour.
Very importantly many other proteins in the cell can suffer acetylation/deacetylation (p53, bcl6, cMyc, NFKB, HSP90, etc.). In global all these proteins are called acetiloma. The final result of HDACi is a group of transcriptional and non-transcriptional effects with cell cycle stop, induction of apoptosis, increase of immunogenicity, antiangiogenic activity, chaperone inhibition, mitotic catastrophe, autophagy and senescence [55–57].
Vorinostat
Vorinostat (Zolinza™) is the first HDACi approved by FDA in 2006 (not approved by EMEA) for the treatment of CTCL progressive, persistent or recurrent after two systemic therapies. Recommended dose is 400 mg daily, oral [58, 59].
Phase IIb clinical trial with 74 patients (most of them stage at least IIb) showed a RR of 29.7 % without CRs (including 30 % of showed a RR in advanced disease, a 33 % of RR in Sézary syndrome and a 22 % of RR in tumoural stage). Median time to response was around 2 months and time to progression, 4.9 months (in cases with stage at least IIb median time to progression was 9.8 months).
The most common adverse events (AE) were diarrhoea (49 %), fatigue (46 %), nausea (43 %) and anorexia (26 %); most were grade 2 or lower but those grade 3 or higher included fatigue (5 %), pulmonary embolism (5 %), thrombocytopenia (5 %) and nausea (4 %).
Post hoc analysis has demonstrated safety of vorinostat after at least 2 years of long-term maintenance [60].
Immunohistochemical analysis of STAT1 and phosphorylated STAT3 (pSTAT3) in skin biopsies obtained from CTCL patients enrolled in the vorinostat phase IIb trial showed that nuclear accumulation of STAT1 and high levels of nuclear pSTAT3 in malignant T cells correlate with a lack of clinical response [61]. On the other hand, HR23B expression pretreatment is considered a biomarker for response to vorinostat [62].
Romidepsin
Romidepsin (Istodax ®) is the second HDACi approved by FDA (2009) for the treatment of adult patients with cutaneous T-cell lymphoma (CTCL) or peripheral T-cell lymphoma (PTCL) who have received at least one prior systemic therapy. Romidepsin is given IV at a dose of 14 mg/m2 on days 1, 8 and 15 every 28 days [63, 64].
Pooled analysis of 2 clinical trials included 167 (71 + 96) patients, 76 % of them at least stage IIb. RR was 41 % with 6 % of CRs. RR in Sézary syndrome was 58 %.
A clinically meaningful improvement in pruritus was observed in 43 % of patients, including patients who did not achieve an objective response.
Time to response was 2 months and median duration of response was 15 months.
Very interestingly, it has been shown that romidepsin increases CD25 expression, giving a rational basis to possible future treatments combined with denileukin diftitox.
Most common drug-related adverse events (AE), all grades, included nausea (67 %), fatigue (49 %), anorexia (37 %), ECG T-wave changes (29 %), anaemia (26 %), dysgeusia (23 %), neutropenia (22 %) and leukopenia (20 %).
Other HDACi are under investigation. Panobinostat (20 mg, oral, days 1, 3 and 5 of every week). A phase II clinical trial reported with Seventy-nine bexarotene-exposed and 60 bexarotene-naïve patients. The ORR was 17.3 % (15.2 % and 20.0 % in the bexarotene-exposed and -naïve groups, respectively). The most common adverse events were thrombocytopenia, diarrhoea, fatigue and nausea [65].
Proteasome Inhibitors: Bortezomib (Velcade™)
Bortezomib is a reversible inhibitor of the 26S proteasome in mammalian cells that degrades ubiquitinated proteins, thereby maintaining homeostasis within cells. Inhibition of the 26S proteasome can affect multiple signalling cascades within the cell, produces stress of the endoplasmic reticulum and can lead to cell death [66].
Bortezomib is FDA approved for the treatment of multiple myeloma patients and mantle cell lymphoma patients who have received at least 1 prior therapy.
In MF, a phase II study [67] with 12 previously treated CTCL (stage III or IVb) patients who received bortezomib as monotherapy for a total of six cycles (1.3 mg/m2 iv, days 1, 4, 8 and 11 out of 21). The overall response rate was 67 %, with two (17 %) CRs and six (50 %) PRs. All responses were durable, lasting from 7 to 14 or more months. The most common grade 3 toxicities were neutropenia (n = 2), thrombocytopenia (n = 2) and sensory neuropathy (n = 1).
Chemotherapeutic Agents
MF is relatively chemoresistant due to the low proliferative rate that frequently have the tumour cells. Both single and multiagent chemotherapy have been used in MF. Chemotherapy should be restricted for advanced MF (stages IIb–IV). There is evidence against its use in early MF. Kaye et al. reported a randomised clinical trial comparing chemotherapy: cyclophosphamide, adriamycin, vincristine and etoposide (CAVE) + total skin electron beam irradiation (TSEB) vs. conservative palliative therapy, consisting of topical mechlorethamine, superficial radiotherapy and phototherapy. RR was better in the chemotherapy group (38 % vs. 18 %), but very importantly, there were no significant differences in disease-free survival or overall survival between the two groups. Toxicity was much higher in the aggressive arm [68].
Single-Agent Chemotherapy
A systematic review including 526 MF patients treated with different single-agent chemotherapeutic agents reported a response rate of 66 % (median duration 3–22 months) with 33 % or CRs [69].
Gemcitabine is a pyrimidine nucleoside analogue that, after phosphorylation, inhibits ribonucleotide reductase and DNA synthesis. It is used IV 1,000–1,200 mg/m2 on days 1, 8 and 15 out of 28. RRs between 50 and 70 % with CRs between 8 and 16 % have been reported. Adverse events include myelosuppression that can oblige to dose reduction, haemolytic uremic syndrome, pulmonary embolism, congestive heart failure, acute myocardial infarction, angina, increased hepatic transaminases, mucositis, lethargy, fever, cutaneous hyperpigmentation, infusion-related maculopapular rash and radiation recall [70, 71].
Chlorambucil is a nitrogen mustard derivative that works as a bifunctional alkylating agent. It is recommended for erythrodermic MF or SS. Usual dose is 2–6 mg/day, combined with prednisone (20–40 mg/day). Other authors recommend pulses every 2 weeks consisting of chlorambucil 10–12 mg/day for 3 consecutive days + flucortolone 75 mg first day, 50 mg second day and 25 mg third day [72, 73].
Methotrexate (MTX) is an antineoplastic antimetabolite with immunosuppressant properties. It is an inhibitor of tetrahydrofolate dehydrogenase and prevents the formation of tetrahydrofolate, necessary for synthesis of thymidylate, an essential component of DNA. Oral weekly doses between 5 and 125 mg have been used.
In patch/plaque stage (Ib), Zackheim and colleagues reported 12 % patients with CR and 22 % of PR. Median time to treatment failure was 15 months [74].
However, MTX has been used mostly for erythrodermic MF or SS. PRs of 17–35 % with 40 % of CRs have been reported [75, 76].
Most common side effects of MTX include ulcerative stomatitis, leukopenia, abdominal distress, fatigue and decreased resistance to infection. Long-term use can produce hepatic fibrosis or even cirrhosis.
Pentostatin (2′-deoxycoformycin ) is a purine analogue and a potent inhibitor of adenosine deaminase, producing apoptosis of lymphocytes. Dose is 5 mg/m2 intravenous (IV) bolus for three consecutive days of every 3-week cycle. Most patients do not have toxicity but cardiac or pulmonary events can be life-threatening. Open studies in MF and SS have reported RRs of 35–71 % with 10–33 % of CRs [77, 78].
Pegilated liposomal doxorubicin (Caelyx™) is an anthracycline glycoside antineoplastic antibiotic. The drug’s precise mechanism of action is not fully understood, but it appears to be a DNA-damaging agent. Dose recommended is 20 mg/m2, days 1 and 14 out of 28 days. Several papers have been published in MF. The EORTC conducted a phase II clinical trial (21012) inclinding 49 patients and reported 40.8 % of response rate (6.1 % had complete responses and 34.7 % experienced PRs). Median time to progression and median duration of response were 7.4 and 6 months, respectively. Most frequent toxicity is palmoplantar erythrodysesthesia. Cardiomyo pathy should be monitored, but cardiac toxicity of liposomal doxorubicin is low [79, 80].
Pralatrexate (Folotyn ™) is a novel antifolate designed for preferential tumour uptake and accumulation. It inhibits dihydrofolate reductase (DHFR). Pralatrexate is given intravenously. Optimal dose is 15 mg/m2/week/6 weeks + vitamin B12 (1 mg i.m. every 8–10 weeks) + folic acid (1 mg/day orally). The subgroup of 12 MF patients included in the PROPEL study, central analysis showed 25 % of response rate with 1.7 months of disease free survival. Investigator analysis of the same group of patients reported a 58 % of response rate with 5.3 months of progression free survival [81, 82].
Most frequent toxicity was mucositis. Pralatrexate was approved by FDA in 2009 but asked post-marketing requirements (a clinical trial comparing pralatrexate + bexarotene vs. bexarotene alone).
Forodesine is a purine nucleoside phosphorylase inhibitor that selectively induces T-cell apoptosis. It is under investigation in CTCL. Recommended dose is 10 mg oral/12 h. There are reports about a phase I/II clinical trial with 64 cases (80 % were at least stage IIb). Overall RR was 39 % (with 3 CRs ). Importantly, erythrodermic MF had higher RR (65 %). Median time to response was 42 days and median duration or response was 127 days+. Main toxicities were nausea, headache, diarrhoea, fatigue, pruritus and peripheral oedema. Grade 3 adverse events were pneumonia, cellulites and diarrhoea [83].
Polychemotherapy
Multiagent chemotherapy should be restricted to advanced MF after failure of several other systemic treatments, including monochemotherapy. The exception is maybe stage IVb in which multiple-agent chemotherapy should be offered early to patients. As commented before, polychemotherapy in early MF achieves higher RR than conservative, skin-directed treatment but gives much higher toxicity without impact in overall survival [68]. Moreover, it is frequent that relapses after polychemotherapy are relatively rapid and frequently aggressive.
A systematic review including 331 patients treated with different combinations [69] reported 31 % of CRs. Median duration of responses was between 5 and 41 months.
Most popular multiple-agent chemotherapy is CHOP (cyclophosphamide, doxorubicin, vincristine and prednisone).
BMTransplantation
Autologous stem cell transplantation (SCT) is not recommended for MF because, although patients achieve response, usually it is very transient, with disease progression occurring within months after the procedure [84]. Even after careful manipulation of the stem cell harvest, most cases present the T-cell clone in the reinfusion sample. Interestingly, the presence or not of the clone does not predict duration of response [85]. A meta-analysis performed to compare the outcome of allogeneic vs. autologous SCT in patients with MF/Sézary syndrome showed a more favourable outcome of patients who received allogeneic SCT [86].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree