When managing cancer pain by interventions, it is important to distinguish between tumor-related pain and nontumor-related pain such as that following treatments (radiation therapy, chemotherapy, surgical resection of tumor). Indeed, many of the pain management issues seen in cancer survivors are similar to those chronic noncancerpain patients. However, in either situation, it is extremely important to establish a cancer diagnosis and treatment plan for the newly diagnosed cancer patient prior to initiation of any interventional pain management strategy. Failure to do so may result in inappropriate interventions (with associated risks) in these patients.
Clinicians managing terminally ill cancer patients with tumor-related pain generally turn to interventional pain management only after medication management has failed. Failure of therapy exists when the patient considers the pain relief inadequate and cannot obtain further relief without unacceptable side effects. In some situations, the use of an interventional modality can be less invasive and troublesome to the patient than continued aggressive medication management. Interventional strategies should be considered under the following headings: radiation, surgical, pharmacologic, and physical (heat/cold) ablation, and neuraxial therapy. Augmentative modalities for nontumor pain will also be briefly considered.
RADIATION STRATEGIES
The goals of radiation therapy may be considered curative or palliative. The aims of radiation palliation are to allow for a symptom-free period longer than the debilitation associated with curative treatment, prolong useful or comfortable survival, relieve distressing symptoms (eg, pain and obstruction), and avert impending problems (eg, spinal cord compression). Radiation therapy is generally considered a local-regional treatment modality. It has a pivotal role in the treatment of cancer pain caused by bone metastases (see
“Focused Management Strategies for Painful Bone Metastases,” page 306), epidural neoplasm (see
“Management of Epidural Spinal Cord Compression,” page 304), and cerebral metastases.
1 Especially when combined with cytotoxic chemotherapy, limited surgical excision, or both, radiation can control disease at the primary site and regional nodes without the need for surgical extirpation, as was frequently used in past years.
Approximately 40% of patients referred for radiation therapy have advanced cancer that does not respond to curative treatment and is accompanied by pain.
2 Rutten et al.
3 evaluated the pain characteristics that help to predict the pain-relieving efficacy of radiation therapy for cancer pain. In a study of 51 patients, they found a significant relationship between pain characteristics (the presence of radiating pain and a low pain score [<35/100] before radiation) and a complete response to palliative radiation therapy. Complete responses to treatment occurred within 21 days of the start of radiation.
Radiation therapy has become a mainstay in the treatment of both primary and metastatic disease of the spine and spinal cord. Although radiation therapy has proven effective in controlling tumors, side effects such as radiation-induced myelitis limit the safely deliverable doses and decrease its efficacy when treating previously irradiated areas. Stereotactic radiosurgery permits high dose treatment while minimizing exposure to surrounding healthy tissues, increasing the safety of initial treatment, and allowing additional radiation of recurrent spinal lesions.
Gerszten et al.
4 reported on the efficacy of Cyberknife treatment on patients with painful metastatic spinal lesions. Axial and radicular pain improved in 74 of 79 patients with a mean radiation treatment dose of 14 Gy. With similar doses for the treatment of painful solitary spinal metastases with or without cord compression, Ryu et al. noted that the median time to pain relief was 14 days and the earliest time of pain relief was within 24 hrs. Complete pain relief occurred in 46%, partial relief in 18.9%, stable symptoms in 16.2%, and relapse of pain at the treated spinal segment was 6.9%. The median duration of pain relief at the treated spine was 13.3 months and the overall pain control rate for one year was 84%
Radiation therapy also has a role in the management of painful, noncancer-related chronic conditions. The Gamma Knife has been used to treat patients with trigeminal neuralgia. Little et al.
5 noted that treatment failed in 33% within 2 years. Thirty-two percent of patients were pain free and off medication and 63% had at least a good outcome at 7 years. When Gamma Knife was used as the primary treatment, 45% of the patients were pain free at 7 years. By contrast, 10% of patients in whom previous treatment had failed were pain free. When needed, salvage therapy with repeat Gamma Knife, microvascular decompression, or percutaneous lesioning was successful in 70%. Posttreatment facial numbness was reported as very bothersome in 5%, most commonly in patients who underwent another invasive treatment. After Gamma Knife, 73% reported that trigeminal neuralgia had no impact on their quality of life.
SURGICAL STRATEGIES
There are a variety of different surgical strategies for symptom-directed interventional tumor pain control (
Table 21.1). Simple tumor resection of painful lesions
(e.g., intra-abdominal tumors or extremity tumors) may result in both resolution of painful lesions and potentially a cure of disease. In patients with advanced disease with evidence of widespread metastatic lesions, surgical resection might still be indicated as part of an effort to palliate symptoms by tumor debulking, decompression of innervated structures, relief of obstruction, or prevention such as intramedullary rodding of impending long bone fractures.
Although limb salvage has replaced amputation in the primary treatment of diseases such as sarcoma, recurrent or persistent disease remains a challenging problem. Pain, fracture, and significant neurologic impairment may accompany primary, recurrent, or metastatic tumors of the major joints. Palliative hemipelvectomy, forequarter amputation, and hip, knee, or shoulder disarticulation for the palliation of pain and symptomatic malignancy have been described as methods of improving quality of life. These procedures are relatively reliable, and may provide excellent pain relief in select groups of patients.
SURGICAL MANAGEMENT OF METASTATIC SPINAL LESIONS
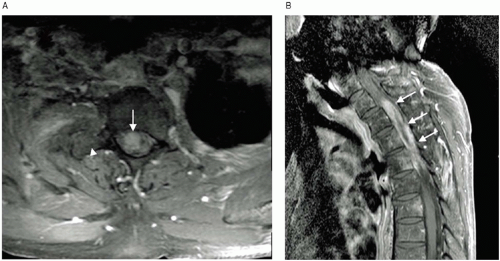
Surgical intervention plays an important role in the comprehensive care of patients with metastatic spinal lesions. Metastatic disease involving the axial skeleton is a common source of morbidity in patients suffering from various primary malignancies (
Fig. 21.1). Adult patients with cancers of the lung, breast, and prostate are most likely to be affected. The thoracic region of the spine is involved in approximately 70% of cases.
Multiple surgical options exist for the treatment of spinal metastases; selection is based upon the patient’s general condition, spinal stability, evidence of spinal cord and nerve root compression, pain, and tumor sensitivity to radiation and chemotherapy. Surgical approaches to the spine with metastatic disease include laminectomy, posterior decompression, posterolateral decompression via the pedicle, posterior instrumentation, anterior decompression, and anterior instrumentation. Sometimes a combined anterior and posterior procedure is indicated. Intraoperative radiation with shielding of the spinal cord has also been described.
6 Surgery is indicated particularly when the primary tumor is relatively radioresistant, current or previous radiotherapy has failed, or the origin of the lesion cannot be determined. Surgical intervention is also favored when neurologic deficits or intractable axial spinal pain are caused by tumor-related spinal instability or pathological fracture that results in retropulsed bone and disc material. Surgery has multiple potential benefits, including protection of the nervous system, stabilization of the spine, reduction of pain, and the ability to obtain a tissue sample for diagnosis.
Only 20% of spinal metastases involve the lumbar spine. The lumbar spine has several unique features that can potentially complicate successful regional decompression and stabilization, including the large size and high weight-bearing demand of the lumbar vertebral bodies, the transition between the kyphotic rib-fixated thoracic spine to a more mobile lordotic lumbar spine, and the restricted access to the lower lumbar segments because of the presence of the pelvic ring. The lumbar nerve roots also innervate muscles that play critical roles in ambulation and cannot be routinely sacrificed to enhance posterolateral access to the vertebral bodies as may be done in the thoracic spine. Also unique is the direct extension of retroperitoneal malignancies into this region of the spine.
Holman et al.
7 demonstrated that when surgical procedures are used for lesions exclusively involving the lumbar spine, significant and lasting reduction in pain due to tumor-related spinal instability, as well as improvement in neurologic status and restoration of ambulatory function, can result. Although the authors concluded that the risk of surgery-related complications was significant, it was also comparable with that obtained in studies involving cervical and thoracic lesions. The indications for surgery in patients with lumbar lesions are similar to those for patients with disease in other spinal regions. Impending or progressive neurologic deficits because of neural compression are not unusual.
Ibrahim et al.
8 reported on a multicenter study of 223 patients referred for surgery for metastatic spine diseases. Surgical therapies were effective in improving quality of life through better pain control and improved sphincter control; these patients also survived longer than those who did not get surgery. As the authors remarked, spinal surgery is not a treatment for the systemic cancer, it is a method of prolonging life and improving the quality of life.
NEUROSURGICAL PROCEDURES
Ablative neurosurgical procedures have been used for several hundred years in the attempt to treat pain associated with cancer.
9 The early operations were mainly peripheral neurectomies, but advances in anesthesia made subsequent intracranial and intraspinal procedures possible. The growth of the basic neurologic sciences that began in the late 19th century led to new surgical procedures based upon anatomical pathways. Most of the important clinical developments in ablative neurosurgery occurred in the first half of the 20th century, culminating in the publication of
Pain: Its Mechanisms and Neurosurgical Control in 1955 by White and Sweet.
10 Several more recent textbooks reviewing ablative neurosurgical procedures for pain are also available.
11,
12,
13The use of ablative neurosurgical procedures in the management of pain associated with cancer has been sharply curtailed in the past 30 years. The factors responsible for this include:
More aggressive care of the underlying malignant disease, eliminating some of the causes of pain
Major advances in the use of oral opioids and adjunctive medications for control of pain associated with cancer
More accurate reporting of operative morbidity and mortality and long-term follow-up of surgical patients
The development of implanted electrical stimulators for pain relief
Most significantly, the development of neuraxial medication delivery systems that have dramatically reduced the number of patients requiring ablative surgery for effective pain relief
By contrast, improvements in the science and art of neurologic surgery have made certain procedures safer and more readily available. Advances in the quality of imaging studies and improved anesthetic techniques have also played a significant role. The surgical microscope, improved lesion-making apparatus, neuronavigation, and endoscopic procedures have all brought new possibilities to the surgeon.
Surgical results will be optimized when the surgeon is a member of a comprehensive interdisciplinary team caring for the patient with cancer and pain.
14 Effective communication between the team members and the patient are a necessity if good surgical decisions are to be made. In general, the patient should have a life expectancy of greater than 3 months if an open (surgical) ablative operation is planned. Percutaneous ablative procedures are wiser for those with less than a 3-month life expectancy. Furthermore, the patient must have reasonable bleeding and clotting parameters (International Normalized Ratio [INR] <1.5, adequate platelet counts) and must be able to resist infection and heal the wound. Special care needs to be exercised if the surgical procedure involves a region of skin that has been previously treated with radiation therapy. The technical skill and experience of the neurosurgeon is an outcome factor that should not be overlooked. Surgeons who rarely perform operations for pain, particularly those requiring stereotactic approaches, cannot be expected to have the high success rates and low complication rates described in the literature by those who have performed hundreds of similar operations.
An important issue that accompanies a surgical procedure to alleviate pain is the management of the patient who is receiving large amounts of opioids at the time a surgical procedure is elected. It is not warranted to require
the patient to reduce or cease opioids before surgery. Such a patient will be very opioid tolerant, and the personnel involved in the perioperative care must be prepared to deal with this issue. If the operation successfully alleviates the preoperative pain, the patient’s need for opioids may be dramatically reduced and a previously well-tolerated dose may now lead to significant side effects, including respiratory depression and oversedation. If such events are anticipated, a careful taper of opioids should be planned accordingly.
The neurosurgeon’s contribution to the management of pain associated with cancer includes more than ablative surgery. Neuromodulation by means of implanted electrical stimulators and drug delivery to the cerebrospinal fluid via implanted catheters and pumps is also useful. All aspects of neuraxial medications are discussed in “Neuraxial Analgesia,”
Chapter 22 and will not be covered in this section. Electrical stimulation is discussed in “Neuromodulatory Treatments for Pain Associated with Cancer,” later in this chapter.
Peripheral Neurectomy
Peripheral neurectomy involves cutting a nerve distal to the dorsal root, external to the spine or cranium. The role of peripheral neurectomy in the management of pain due to cancer is very limited.
15 The theoretical advantages are the ease of surgery, complete denervation in the distribution of the cut nerve, and, that a preoperative nerve block with a local anesthetic will accurately reveal the extent of denervation and whether or not pain relief can be expected from the operation. The disadvantages of a peripheral neurectomy include the loss of all sensory modalities in the denervated region, the loss of motor function if the nerve to be cut is mixed, the re-innervation that will occur because of both peripheral and central sprouting, and the potential for growth of the neoplasm to go beyond the denervated region and lead to pain recurrence.
Surgical intercostal neurectomy may be useful in a patient with chest wall neoplasm too frail to undergo dorsal rhizotomy. The loss of intercostal muscle function in the denervated region is usually inconsequential. Denervation of abdominal segments may result in muscle weakness that produces an asymmetrical abdominal protuberance that the patient may find painful and embarrassing. Neurectomies in the extremities are usually unwise because of the paresis that ensues. Cranial rhizotomies are usually a better choice than neurectomies for pain due to cancer. Peripheral neurectomies can also lead to a painful neuroma or denervation pain; both can be difficult to manage.
Surgical Sympathectomy
Sympathectomy involves excision or cauterization of the paravertebral sympathetic chain and associated ganglia or their peripheral branches. Surgical sympathectomy plays a limited role in the management of pain secondary to cancer. Nociceptive afferents from the viscera travel in the sympathetic chains and vagus nerve and may be surgically interrupted. Splanchniectomy may be part of an abdominal operation and can provide relief of visceral-mediated pain. However, this is a formidable surgical procedure by itself that can usually be much more easily accomplished with neurolytic agents that are percutaneously administered.
Some of the pains associated with cancer are not nociceptive but arise from nerve injury by the neoplasm, surgery, or radiation therapy. This component of neuropathic pain may respond to sympathectomy. Therefore, if the patient’s pain persists after somatic blocks or ablative surgery, sympathetic block is warranted to ascertain if the pain can be eliminated. If so, a sympathectomy should be considered.
16 In addition to the traditional older methods for an open sympathectomy, there are now endoscopic and percutaneous methods of achieving sympathectomy. Neurolytic sympathetic blocks are probably a better choice than open sympathectomy in the cancer pain patient.
Dorsal Rhizotomy
A rhizotomy is a surgical procedure to cut nerve roots. Because most peripheral nociceptive impulses are conveyed through a mixed somatic nerve to the spinal cord via the dorsal root, dorsal rhizotomy was the most commonly performed operation for pain relief in the first 75 years of the 20th century. As better clinical trials with longer follow-ups were reported, the popularity of dorsal rhizotomy waned. This was initially because of the development of cordotomy and then the use of intraspinal opioids. The advantages of dorsal rhizotomy include: All modalities of sensation but no motor function is lost in the denervated area, large areas can be denervated by cutting many adjacent dorsal roots, and nerve blocks can be used to determine the required extent of denervation. The disadvantages include the fact that one cannot totally denervate an extremity without losing useful function, a laminectomy is required for each root to be cut, and sprouting, both peripheral and central, may cause pain relief to be temporary. This operation is particularly useful for thoracic and abdominal wall pain but it will not interrupt or attenuate visceral pain. From a practical perspective, it is always necessary to section two roots above and two roots below the region of pain to get reliable pain relief that may last for the duration of the patient’s life. This can lead to the need for very extensive laminectomies if an open procedure is contemplated.
Percutaneous dorsal rhizotomies have particular utility in the patient with pain due to cancer. This strategy does put at risk the artery that accompanies the dorsal root; particularly in the lower thoracic region this can lead to spinal cord infarction. Sacral rhizotomy via a laminectomy at S2 and epidural ligation of all the nerve roots in the cauda equina can effectively alleviate pelvic pain in the patient who has already had urinary and fecal diversionary procedures.
17It is unclear whether or not resection of the dorsal root ganglion adds to the likelihood of success for dorsal rhizotomy.
18 Most of this controversy relates to patients with lumbar rhizotomy for failed back surgery syndrome and cannot be extrapolated to patients with pain due to cancer. Ganglionectomy is frequently followed by a transient dysesthetic pain syndrome in the denervated area and patients should be warned of this. Ganglionectomy is an extradural procedure and the risk of cerebrospinal fluid (CSF) leak is far less than after intradural rhizotomy.
Cranial rhizotomy may be useful in patients with head and neck cancer that has not been controlled by other means. The traditional procedure has been a posterior fossa approach to the trigeminal, nervus intermedius, and glossopharyngeal and upper vagal nerves accompanied by section of the dorsal roots of C2 and C3 (there is no dorsal root of C1). Such an operation produces complete anesthesia of the face and pharynx and can only be done unilaterally. It can provide significant pain relief (75% success rate) in appropriately selected patients for the duration of the cancer patient’s life. Unfortunately, many patients with advanced head and neck cancers have extensive tumor involvement which overlaps dermatomal segments that reduces the likelihood of successful pain relief with single nerve cranial rhizotomy.
Cordotomy
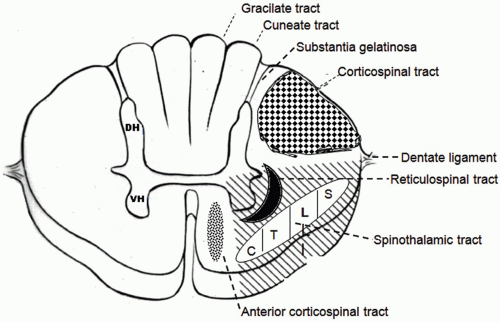
A cordotomy involves an incision or Radio Frequency (RF) lesion made in the anterolateral quadrant of the spinal cord to interrupt the axons of the spinothalamic tract (
Fig. 21.2). Cordotomy was the most commonly performed operation for cancer pain before the advent of intraspinal opioids. The advantages of cordotomy are that only pain and temperature sensation are abolished contralateral to the lesion in the spinal cord, commencing three segments below the level incised. This means that the level of the operation can be tailored to the region of pain. Motor loss is not expected and touch and position sense remain intact. The disadvantages include the tendency of the pain relief to fade after a year or so, the fact that bilateral lesions can lead to impairment of bladder function, and that bilateral high cervical cordotomy can lead to Ondine Curse, the failure to breath when the patient is asleep.
19 Cordotomy can be performed at the upper thoracic level for lower half of the body pains and at the high cervical level for pains below C5. Percutaneous cordotomy is performed at the C1-2 level and offers the possibility of surgical pain relief in a patient too debilitated to withstand an open procedure.
20 A computed to-mography (CT)-guided method has been developed that lowers the risks of an inappropriate lesion site. For most cancer pain patients, percutaneous C1-2 cordotomy is the procedure of choice, although bilateral lesions do have significant risks to both bladder function and loss of CO2 responsiveness. The quality of pain relief is identical with both the open and percutaneous operations. Raslan
21 described the use of percutaneous CT-guided radiofrequency ablation of upper cervical spinal cord pain pathways in the treatment of cancer-related pain. Fifty-one patients with cancer-related body or face pain were treated with computed tomography-guided radiofrequency ablation of the spinothalamic tract or trigeminal tract nucleus in the upper cervical region of the spinal cord. Forty-one patients underwent a unilateral cervical cordotomy, and ten patients underwent a trigeminal tractotomy-nucleotomy (TR-NC). Patients with somatic pain on one side of the body reaching to the midline and below dermatome C5 and patients with visceral pain restricted to one side of the body not reaching the midline were offered cervical cordotomy. Patients with somatic pain involving one side of the face, tongue, or inner mouth were offered the option of TR-NC. Forty-one patients underwent cervical cordotomy at C1-2 level, and ten patients underwent TR-NC also at the C1-2 level. The results from these procedures are shown in
Table 21.2.
Postoperatively, 98% of the patients were Grade I or II, which was categorized as a successful procedure. At 1 month postoperatively, 98% of the patients remained Grade I or II, which decreased to 80% at 6 months follow-up. One patient, who was Grade III at 1-month follow-up, dropped to Grade IV at 3 months follow-up and died before the 6-month follow-up contact. Despite two patients having only one lesion performed and the procedure halted, results in terms of pain relief in the first 3 months were not affected and most likely reflect the effect of a single lesion. No complications related to the procedures used were observed. No change in motor strength was recorded in any patient. No patient developed sleep apnea. There were no permanent or serious
complications such as respiratory depression and/or weakness in this series. Complications were transient and not severe. Hypotension occurred in three cases (two cordotomies and one TR-NC). All patients responded to treatment with 24-hour parenteral fluid administration and were discharged without event. Headache was reported in four patients (three cordotomies and one TR-NC). All were treated with analgesics and fluids for 48 hours and discharged without event. Dysesthesia occurred in two patients undergoing cordotomy and persisted in one patient for 3 days and in the other for 2 weeks, which completely resolved by the first month follow-up assessment.
Most other large series reveal an 80% success rate in cancer patients, although those who survive for several years may lose the cordotomy effect. Failure to get initial pain relief almost always means that the cordotomy lesion was not large enough or that it was not far enough above the source of pain. Midline or bilateral pain from the pelvis is better treated with a midline myelotomy than bilateral cordotomies.
Myelotomy
Myelotomy for pain is an operation to incise the spinal cord in the dorsal midline so as to transect the decussating spinothalamic fibers and/or damage the visceral afferent tract that ascends in the deep medial dorsal columns. On the basis of these novel pathways, midline myelotomy (either commissural or punctate), has been developed as treatment of visceral pain. Midline myelotomy has the advantage of producing bilateral pain relief from a single incision in the spinal cord. At first, this operation was thought to provide pain relief by sectioning the decussating spinothalamic fibers. However, the studies of Willis et al. and the clinical observations of Hitchcock have indicated that there is a visceral afferent tract that travels in the deep midline of the dorsal columns.
22 The axons of this pathway ascend in the ipsilateral dorsal column and terminate in the nucleus gracilis from where the nociceptive input is transmitted to the contralateral ventral posterolateral thalamus. This tract probably explains the observation that pain relief can be found in regions of the body below the level of pain and temperature loss. A midline myelotomy, whether longitudinal or punctate, has a very low risk of impairing motor function, although some proprioceptive losses in the lower extremities are not rare after this procedure. The procedure requires a low thoracic laminectomy and the duration of pain relief may not be more than a year in many patients.
Hwang et al.
23 reported on the use of a punctate midline myelotomy at the T3 vertebral level in a small number of patients with visceral pain associated with hepatobiliary or pancreatic cancer. Although only six patients were studied, their results suggest some use of this technique in the management of severe pain for these particular cancers. In an experimental animal model, Chang
24 reported on the use of a high cervical punctate midline myelotomy for intractable visceral pain due to abdominal or pelvic cancers. Similarly, Hitchcock
25 described a high cervical midline myelotomy that produced pain relief without sensory loss, but few have replicated his findings.
12 Nauta et al.
26 performed a punctate midline myelotomy in six cancer patients with intractable refractory visceral pain and noted good pain relief with significant opioid reductions postprocedure.
Dorsal Root Entry Zone Lesions
Dorsal root entry zone (DREZ) lesions require destroying the central projections of nociceptive afferents where they enter the spinal cord. DREZ were first performed by Nashold in 1975, although Sindou described sectioning the lateral root fibers going to the Lissauer tract in 1972. In North America, the Nashold strategy has been the most commonly utilized. This operation has the advantages of producing complete sensory loss in the segments incised, has a long-lasting effect, does not produce any motor loss, and is most effective for neuropathic pain states. Its disadvantages include requiring a laminectomy for each level to be lesioned, risk to spinal cord function with ipsilateral motor and dorsal column function loss (about 10% of patients), and being a major operation with significant surgical stress. The lesion in the root entry zone can be made with a radiofrequency electrode, a laser, or a knife. In the management of pain due to cancer, it is not clear that this operation is any better than dorsal rhizotomy, which certainly has less risk of spinal cord dysfunction.
An analogous operation can be performed on the descending trigeminal nucleus and root entry zone in the
medulla to treat chronic pain in the face and pharynx; this is much more commonly used for neuropathic pains than those due to cancer.
27 Only pain and temperature sensation is lost; corneal anesthesia does not ensue. The operation can be performed bilaterally if necessary.
Medullary or Mesencephalic Spinothalamic Tractotomy
This is an open operation with direct visualization of the brain stem and the localization of a lesion in the spinothalamic tract by anatomic features. This permits a higher section of the spinothalamic tract and a higher level of analgesia that includes the cervical region. The operation has been most frequently performed for cancer pain involving the shoulder and neck on the opposite side of the body. The success rate has been around 50% with a 15% complication rate, and the pain relief often does not last for more than a year.
28 This is a major surgical procedure and is rarely performed today; stereotactic surgical procedures and aggressive use of opioids have superseded this operation.
Stereotactic Mesencephalic Spinothalamic Tractotomy
Open mesencephalic tractotomy had a much-too-high neurologic complication rate; in 1962 Spiegel and Wycis described stereotactic mesencephalic tractotomy. This operation has been widely used and is known to yield a 50% to 80% success rate; however, most patients will again report pain after a year or so.
29 The operative mortality is 5% to 10%, and about 20% of patients complain of transient dysesthesias or oculomotor disturbances. This operation is aimed at sectioning the spinothalamic fibers and adjacent spinoreticular fibers. A limited number of neurosurgeons are comfortable performing stereotactic lesions for pain. The surgical stress and morbidity are low; this operation does have utility for cancer pain patients. The pain is relieved on the opposite side of the body from the tractotomy and bilateral lesions can be made for bilateral pain. Head and neck as well as body pains can be controlled by mesencephalic tractotomy, as the trigeminal and spinal noxious afferent thalamic fibers are adjacent to each other.
Thalamotomy
This operation destroys a target area in the thalamus. A panoply of thalamic sites have been the target for stereotactic relief of pain. The results have been highly variable, certainly in part because of the different targets and lesion sizes (
Table 21.3). The major issue with all of the sites has been the transient pain relief; good results do not often last more than 1 year. Producing a lesion in the thalamus by radiofrequency current, cryoprobe, or radiosurgery (Gamma Knife) may have significant side effects if the lesion is not precisely located in the desired area. Modern magnetic resonance imaging (MRI) scanning and neuronavigation equipment have reduced the risk of target errors.
Lesions in the ventrocaudal nuclei produce the loss of all sensory modalities as well as pain and for this reason they are not optimal for most patients. Lesions in the medial thalamus or pulvinar have been more useful as they only produce pain relief without sensory loss. Lesions in the anterior nuclei seem to resemble cingulumotomy in producing abatement of suffering rather than pain. Many other regions have been targeted, but the reported case series are small and results not reliable. Thalamotomy utilizing the Gamma Knife to avoid any surgical procedure is probably going to be used more in coming years.
30
Hypothalamotomy
This operation has rarely been performed and the true long-term results are unknown. It does not have a place in the current neurosurgical armamentarium.
Cingulumotomy
Bilateral lesions are made in the mesial frontal lobes to interrupt the cingulum bundles. This operation was first performed by Foltz and White in 1962.
29 Large series of patients have been carefully studied and the clinical results are well established. The principle of this operation is to disconnect the limbic structures that process affective states from the spinothalamic afferents that transmit pain sensations. The short-term success rate for patients with cancer is about 80%; good data on long-term outcomes is sparse but we know there is some drop off.
30 Cingulumotomy does not alter sensation in any way. Patients report that they still have pain but that it does not cause them to suffer. It clearly does not alter cognition or judgment. Originally performed through bilateral frontal burr holes with radiofrequency lesions, it is now possible to perform cingulumotomy using stereotactic radiosurgery (Gamma Knife) and avoid any surgical procedure.
Cortical Gyrectomy
Shortly after World War II, resections of the postcentral and even precentral gyri were reported to be useful in the management of pain on the opposite side of the body. Follow-up reports and larger case series did not reveal many long-term good results; this operation is not performed today in the pursuit of pain relief.
31
Hypophysectomy
The recognition that some cancers were endocrine dependent led to the idea that hypophysectomy might remove the trophic hormones and retard tumor growth and dissemination. The initial procedures were performed subfrontally
via an open craniotomy. Then, innovative techniques such as transecting the pituitary stalk while preserving the gland, the use of stereotaxis to make a lesion within the pituitary fossa, and the injection of alcohol via a transsphenoidal route broadened the use of this operation. It was also recognized that endocrine sensitivity was not required for the patient to obtain pain relief; nor was tumor regression. Pain relief may start very rapidly after pituitary destruction. Significant complications including partial diabetes insipidus in 75.5%, and CSF leaks in 11.3% after transsphenoidal microsurgical hypophysectomy were reported in one series.
32 Stereotactic radiosurgery (Gamma Knife) has greatly reduced the morbidity associated with pituitary operations. Approximately 70% of patients with disseminated cancer will gain significant pain relief for 3 months up to 1 year from this operation, no matter how the lesion in the gland is made.
32 Hormone replacement therapy is usually required. The mechanism of pain relief is not understood. Pituitary ablation may have some utility for the disseminated cancer pain patient who has failed opioid therapy by oral and intrathecal routes.
33