Surgical Technique
James Kenneth Byrd
Samuel L. Oyer
Eric J. Lentsch
Historically, little change has occurred in thyroid surgery since Theodore Kocher developed the classic techniques of thyroid surgery described below. However, in the last few decades there has been a period of innovation with the advent of “minimally invasive” surgical techniques. Over this time, multiple minimally invasive techniques (including CO2 insufflation, endoscopic without CO2, and video assisted) have been described, and for each technique multiple approaches (including cervical, axillary, postauricular, sublingual, and chest wall) have been followed. Of the many procedures, two techniques have become popular and well-studied—minimally invasive video-assisted thyroidectomy (MIVAT) and transaxillary endoscopic thyroidectomy, with or without robotic assistance.
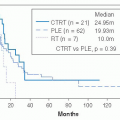
MIVAT was developed for thyroid nodules, but soon the technique was expanded for use in early thyroid cancer and even central compartment dissections.1 Multiple groups have reported on the safety and efficacy of the procedure for thyroid nodules,1,2,3 and the data continue to be compelling for its use in early differentiated thyroid cancer.4,5 However, the studies on the use of MIVAT for cancer have very short follow-up, and more time is necessary to fully evaluate its efficacy in the cancer setting.
Transaxillary endoscopic thyroidectomy, with or without robotic assistance, is the latest progression in the evolution of thyroid surgery and has taken the “minimally invasive” concept to its extreme by providing for “scarless” thyroid surgery. The best studied example of this is transaxillary endoscopic/robotic thyroidectomy. This technique can be done with standard endoscopic instruments or with the use of the daVinci robot; it has become popular in the past decade in Korea and Japan because it completely avoids a neck incision. When compared with open thyroidectomy, preliminary experiences have shown a comparable rate of complications and surgical completeness with superior cosmesis.6 However, few studies are available to document the efficacy of this technique for thyroid cancer,7 and as with MIVAT, they are limited in terms of follow-up.
Therefore, at this time “classical” open thyroid surgery, as described by Kocher, remains the “gold standard” for thyroid cancer. Thyroid lobectomy (or hemi-thyroidectomy) may be an option for early cancers, as has been well demonstrated in the literature. However, at this time most thyroid cancers are treated with total thyroidectomy. Recent evidence has shown that MIVAT appears to provide as complete a removal of diseased tissue as open techniques,4 however, the follow-up data on patients undergoing this procedure are not mature, and definitive recommendations for its use are difficult to make with certainty. In our opinion, it is a reasonable technique for early-stage differentiated cancers, but the surgeon should be willing to convert to an open technique if complete tumor removal is in any way compromised. Transaxillary endoscopic/robotic thyroidectomy has not been well studied in cancer patients and no recommendations for its use can be made. The following technique descriptions represent the distillation of these techniques and represent the current mainstays in our surgical armamentarium of thyroid surgery.
CLASSIC THYROIDECTOMY
The classic procedure for thyroidectomy has changed little since Kocher’s time. Paramount to the surgery is identification of critical structures in the neck, including the superior and recurrent laryngeal nerves, common carotid artery, superior and inferior thyroid arteries, middle thyroid vein, and parathyroid glands.
The classic thyroidectomy begins with the patient under general anesthesia, positioned supine, with a shoulder roll in place. A horizontal skin incision, preferably placed in a skin crease, is made between the cricoid cartilage and sternal notch. Dissection is taken to the strap muscles, which are separated in the midline to expose the gland (Fig. 28-28A).
The middle thyroid vein is usually encountered first and ligated to provide better exposure (see Fig. 28-28B and C). Next the gland is dissected superiorly, remaining on the thyroid capsule, and the superior thyroid vessels are identified. When taking
down the superior pedicle, individual branches of the artery should be divided on the gland with the superior laryngeal nerve visualized, as the nerve may cross the superior pole of the gland (see Fig. 28-28D). As the gland is dissected inferiorly, a careful observation should reveal the parathyroid glands and the recurrent laryngeal nerve. The inferior thyroid artery is a relatively reliable landmark for the recurrent laryngeal nerve, which crosses deep to the artery in most, but not all, cases. At this point, the inferior thyroid vessels are identified and ligated (see Fig. 28-28E). As the gland is further rotated medially, the gland is dissected free from the recurrent laryngeal nerve. By tracing the nerve to its point of entry into the larynx, the gland can be dissected off Berry ligament, and subsequently off the trachea (see Fig. 28-28F). The pyramidal lobe, if present, is removed at this time. If a lobectomy is to be performed, the isthmus is divided and the procedure ended. If a total thyroidectomy is to be performed, the identical procedure is performed on the opposite side. The wound is closed in multiple layers, with or without a drain.
down the superior pedicle, individual branches of the artery should be divided on the gland with the superior laryngeal nerve visualized, as the nerve may cross the superior pole of the gland (see Fig. 28-28D). As the gland is dissected inferiorly, a careful observation should reveal the parathyroid glands and the recurrent laryngeal nerve. The inferior thyroid artery is a relatively reliable landmark for the recurrent laryngeal nerve, which crosses deep to the artery in most, but not all, cases. At this point, the inferior thyroid vessels are identified and ligated (see Fig. 28-28E). As the gland is further rotated medially, the gland is dissected free from the recurrent laryngeal nerve. By tracing the nerve to its point of entry into the larynx, the gland can be dissected off Berry ligament, and subsequently off the trachea (see Fig. 28-28F). The pyramidal lobe, if present, is removed at this time. If a lobectomy is to be performed, the isthmus is divided and the procedure ended. If a total thyroidectomy is to be performed, the identical procedure is performed on the opposite side. The wound is closed in multiple layers, with or without a drain.
LARGE GOITER AND SUBSTERNAL GOITER
Large goiter can be a cause of concern for both the anesthesiologist and the surgeon. Goiter size and bilateral goiter appear to be predictors of difficult intubation8; therefore, careful preoperative planning with the anesthesiologist may be required in these cases.
In cases of substernal goiter, standard techniques and gentle upward traction on the gland is usually all that is needed to “deliver” the gland into the neck. Identification and tracing the RLN inferiorly is often necessary to free the gland from surrounding tissues and safely pull the substernal portion superiorly. The need for sternotomy or thoracotomy in substernal goiter is rare. A recent review of the literature, found that extracervical approach was required only 2% of the time.9 To date, there are no clear-cut indications for sternotomy, and much of the time it is dependent on the surgeon’s experience, skill, and comfort level.
MINIMALLY INVASIVE TECHNIQUES
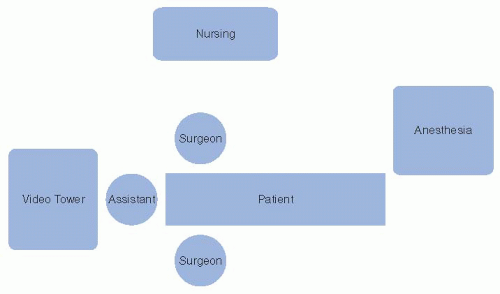
Video-assisted Thyroidectomy
In this technique, the room is set up as shown in Figure 28-29. The surgeon may stand on either side of the neck based on preference, with one to two assistants standing on the opposite side. The patient is positioned as for a classical thyroidectomy, except the neck is only slightly extended without the use of a shoulder roll. A 15-to-25-mm horizontal cervical incision is placed in the midline conforming to a preexisting skin crease if possible (Fig. 28-30A). The incision is made and carried down through the skin, dermis, and subcutaneous tissues. Notably, the platysma muscle is typically not encountered because the location and short length of the incision results in a dissection plane between the medial heads of this muscle. The midline raphe is exposed and opened and the thyroid gland is identified (see Fig. 28-30B). The thyroid gland is then mobilized away from the strap muscles, and the middle thyroid vein branches are ligated with the ultrasonic shears. At this point, retractors are placed laterally around the strap muscles, and medially around the thyroid gland itself, to retract the gland up and over the trachea.
At this point, the endoscope is brought into the field. Usually a 5-mm 30-degree laparoscopic telescope is placed just inside the wound, and both the surgeon and the assistant work off the appropriately positioned monitors. The dissection is then carried out, as described above, for a classical thyroidectomy (see Fig. 28-30C-D) until the gland is mobilized and freed from all surrounding structures. The main difference in this portion of the operation is the use of special endoscopic instruments, and the ultrasonic shears are used throughout.
Once the gland has been mobilized, the final removal of the gland is achieved using an open approach. The thyroid isthmus is divided at this point, or alternately it can be done as a last step before retrieving the specimen. The thyroid gland is delivered through the wound and remains attached primarily by the ligament of Berry. At this point, the recurrent laryngeal nerve is traced to its entry in the region of the cricothyroid joint (see Fig. 28-30E). The connective tissue attachments between the gland and the trachea are divided and the specimen is removed (see Fig. 28-30F). If a total thyroidectomy is to be performed, the contralateral gland is removed in similar fashion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree