Surgical Technique
Vikas Mehta
Robert L. Ferris
INTRODUCTION
Over the last decade, technological advances in minimally invasive, transoral surgical techniques have revolutionized the treatment paradigm for oropharyngeal neoplasms. Since the early 1990s, due to evidence extrapolated from the VA larynx and RTOG 91-11 trial1,2 for nonsurgical larynx preservation, primary surgical therapy was reserved for small tumors (<1.5 cm) of the posterior pharyngeal wall and the tonsils, carcinomas requiring bony resection or tumors not sensitive to radiotherapy. Organ-preservation protocols demonstrated not only that patients treated with primary radiation therapy had similar survival rates to upfront surgical therapy, but also that primary surgical patients were 10 times more likely to have severe morbidity or mortality.3 The complications from traditional surgical methods were largely due to external surgical approaches, which required opening the pharyngeal and oral contents to the neck, with the patient often needing a tracheostomy and feeding tube. The addition of a mandibulotomy and/or glossotomy further increased postoperative speech and swallowing dysfunction, as well as cosmetic deformity.
With the sharp increase in the prevalence of human papillomavirus (HPV)-associated oropharyngeal squamous cell carcinoma (OPSCC), there has been a corresponding shift in the affected population to younger, nonsmoking patients.4 Per the current practice guidelines, these HPV-positive patients undergo intensive chemoradiotherapy (CRT) protocols, just as their HPV-negative counterparts, but with drastically improved survival. The increased risk for these younger patients of long-term sequelae such as osteoradionecrosis, progressive dysphagia, fibrosis, aspiration, and radiation-induced malignancy has led head and neck surgeons to explore minimally invasive surgical techniques to minimize the morbidity of surgical resection and reduce the need for high-dose chemoradiotherapy. Additionally, the very good survival of patients with advanced OPSCC treated with CRT can be primarily attributed to increasing rates of HPV-positive disease. A multicenter phase III trial reported 3-year overall survival (OS), disease-free survival (DFS), and loco-regional control rates of 51%, 42%, and 66%, respectively, when treated with chemoradiation.5 When the TAX 324 study, a phase III CRT trial of 264 patients with OPSCC, was stratified by HPV status, 5-year survival was 82% for HPV+ and 35% for HPV- patients.6
Both transoral laser microsurgery (TLM) and transoral robotic surgery (TORS) have demonstrated excellent oncologic results with good functional outcomes for oropharyngeal tumors,7,8,9,10 leading to a change in the National Comprehensive Cancer Network 2011 guidelines to remove primary radiation therapy as the Category 2B preferred treatment for early oropharyngeal cancer.
For advanced, high-volume, or post-CRT recurrent oropharyngeal carcinoma, surgical resection via an external approach is often required. The choice of open surgical approaches depends on the location of the tumor and degree of bony involvement. The oropharynx contains structures crucial for deglutition, respiration, and phonation. There is no one approach that allows wide exposure with minimal morbidity. The three main routes are combined transoral/transcervical, transpharyngeal, and transmandibular approaches. Each has its own risks and sequelae to these vital structures. If necessary, a maxillectomy and/or mandibulectomy can be combined with any of the three techniques. Often, oropharyngeal resections will require flap reconstruction. This chapter will address the indications, advantages and disadvantages of the transoral and external approaches.
Minimally Invasive Transoral Approaches
Minimally invasive surgical techniques have greatly expanded the scope of the transoral approach for oropharyngeal resections. Traditionally, transoral surgery was reserved for tumors <2 cm of the tonsil, the soft palate, and the posterior pharyngeal wall. Larger neoplasms or tumors of the base of tongue were difficult to access, especially at the deep margins. The use of endoscopes greatly improved transoral visualization of the oropharynx by magnification, tissue distention, and angled optics. Additionally, advancements in laser delivery systems and the wristed technology of the DaVinci robot have allowed increased freedom of motion in previously inaccessible subsites. These innovations have enabled surgeons to remove large neoplasms from the oropharynx with excellent oncologic control and functional outcomes.
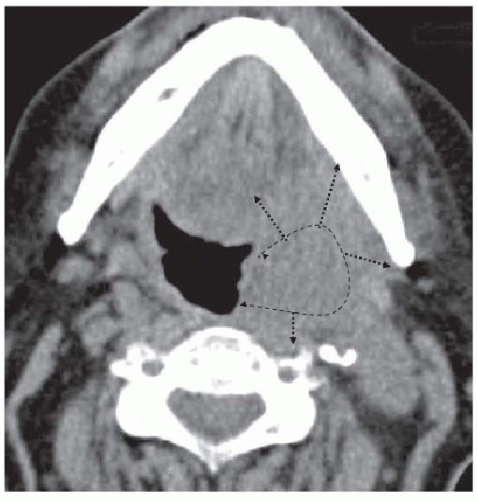
Transoral Laser Microsurgery
Transoral laser microsurgery was first introduced by Strong and Jako in 1972.11 Despite promising initial results, it soon fell out of favor as an oncologic treatment option due to early difficulties with exposure and en bloc removal. In 1993, Steiner revolutionized the field of minimally invasive transoral surgery by presenting an article describing results with a piecemeal resection utilizing a tumor-splitting approach.12 The splitting of the tumor in this dimension allowed much better assessment of the deep margins (Fig. 17-33). Steiner’s report was followed by a rapid influx of evidence supporting the roles of TLM in treating cancer of the upper aerodigestive tract. Recent large cohort studies and multicenter case series have reported oncologic results for laryngeal and oropharyngeal neoplasms that are comparable to nonsurgical management, with improved functional outcomes and decreased health care costs (mean cost of US$3,281 for TLM compared to US$13,825 for XRT).10,13,14,15,16,17
While most of the supporting evidence for TLM is in early glottic cancer, there has been promising results with OPSCC over the last decade. In 2003, Steiner et al. reported on a cohort of 48 patients with OPSCC treated with TLM, of which 94% were stage III/IV.18 Twenty-three of the 48 patients required therapy for either deep extension into the tongue base or positive resection margins. The 5-year local control for all T stages was 85% with no local recurrences in the T1 or T2 group and a 20% local recurrence rate for T3/T4 tumors. OS and DFS were 52% and 73%, respectively.
In a recent, multicenter, prospective study of primary, TLMresected, stage III/IV OPSCC, 204 patients were reported.10 Twoand 5-year estimates demonstrated an OS of 89% and 78%, DSS of 91% and 84%, and DFS of 85% and 74%, respectively. The survival results are comparable with studies using chemoradiation as the primary treatment modality, with improved functional outcomes. A recent CRT study (n = 71) by Huang et al. with 32% of the tumors staged T3 and T4, showed a 3-year OS of 83% and a loco-regional control rate of 90%.19 In the TLM study, with
34% T3 and T4 tumors, the OS was 86% at 3 years and loco-regional control of 93%. The matched, chemoradiation group in this report had a long-term G-tube rate of 35% compared with 3.4% in the TLM study.
34% T3 and T4 tumors, the OS was 86% at 3 years and loco-regional control of 93%. The matched, chemoradiation group in this report had a long-term G-tube rate of 35% compared with 3.4% in the TLM study.
Studies have also indicated that TLM-based surgical treatment without adjuvant therapy can be used with excellent oncologic control for early T-stage OPSCC. In 2009, Grant et al. reported 69 cases of oropharyngeal carcinoma staged T1 to T4 (T1 = 25, T2 = 30, T3 = 12, T4 = 2) treated with TLM and a neck dissection, if indicated.13 None of the patients received adjuvant radiation therapy, either because it was not indicated or the patient declined. Five-year OS was 86% with loco-regional control of 90% for T1 and 94% for T2. None of the T3 or T4 patients had a local recurrence. In terms of functional outcomes, none of the patients required a long-term feeding tube and 98% reported normal or near-normal swallowing, using the Salassa scale.
Technique TLM is usually done with either a microscopemounted carbon dioxide laser or a hollow-fiber carbon dioxide laser system. Exposure of the tumor is achieved with a variety of specialized endoscopes, and excision is performed either circumferentially (en bloc) or in a tumor-splitting fashion (Fig. 17-33), to ensure adequate surgical margins. Tumor mapping and margin status is typically performed using both frozen-section and permanent pathologic analysis. The reported complication rate of TLM is extremely low with the most common problem encountered being postoperative bleeding at a rate of 1.5% to 3%.13,20 Contraindications to TLM include inadequate endoscopic access, which is unusual for oropharyngeal carcinomas, or projected unresectability because of a probable positive margin. Examples of an unresectable tumor are lateral extension of a tonsillar primary into the infratemporal fossa invading the great vessels or ventral extension of tongue base tumors into the anterior floor of mouth.
Transoral Robotic Surgery
The first described use of robotics in head and neck surgery consisted of a robotic-assisted salivary gland resection and neck dissection in an animal model.21 The elimination of hand tremor and superior, three-dimensional visualization were both described as significant advantages.21 The feasibility of transoral robotic surgery was investigated at the University of Pennsylvania, first using a human cadaver,22 followed by a supraglottic laryngectomy in a canine model.23 Protocols were then established for positioning, use of 5-mm instruments, and hemostasis.23,24 The first documented OPSCC TORS resection was in three patients with early T-stage, base of tongue SCCs. En bloc resection with negative margins was achieved in all three cases with no complications or change in swallowing function.25
In 2007, a case series of 27 patients with tonsillar SCC underwent primary resection with TORS.26 The patients were mostly stage III/IVa.24 Neck dissections were performed on 26 of the 27 patients with 24 of the patients having at least one positive node. The cervical lymphadenectomy was performed 1 to 3 weeks after the TORS procedure to minimize lymphedema in the oropharynx after TORS. Negative margins were achieved in all of the cases and there were no loco-regional recurrences during the 2-year study period with a minimal of 6-month follow-up. All of the patients who returned for evaluation (26 of 27) tolerated a regular diet without the need for a gastrostomy tube. Only one patient required a tracheostomy for preexisting sleep apnea, which was exacerbated by the surgical procedure.
Since 2007, several institutions have reported case series highlighting the efficacy of TORS for OPSCC.9,27,28,29,30,31 These reports document excellent oncologic outcomes in patient series ranging from 20 to 47 patients. In the patient population presented by Moore et al.,9 12 of 45 patients (27%) were able to avoid adjuvant radiation, and at 1-year follow-up in this series, no local recurrences were detected. Weinstein et al.31 reported a series of 47 patients with advanced OPSCC (stage III/IV). One patient had a positive margin (2%). DSS was 98% at 1 year and 90% at 2 years. Due to the TORS procedure, 18 of 47 patients (38%) avoided chemotherapy, and 5 patients (11%) did not require any adjuvant therapy. In a prospective, phase I single arm study,32 31 patients underwent TORS with selective neck dissection(s) (SND) with a 100% disease control rate and a 2-year PEG dependency rate of 0%. Seven patients avoided adjuvant therapy and 15 of the remaining 24 (62.5%) received radiation alone (60 Gy to the primary site and dissected neck, 54 Gy to the contralateral neck and retropharyngeal nodes) based on the lack of nodal extracapsular extension (ECE).
Functional outcome studies in OPSCC patients undergoing TORS resections have reported superior swallowing results when compared to published, organ-preservation protocols.8,9,29,30,33,34. In a direct comparison of TORS versus CRT with matched group of OPSCC patients at a single institution, TORS was associated with better short-term eating ability (swallowing score 72 vs. 43, p = 0.008), diet-tolerance (43 vs. 25, p = 0.01), and Functional Oral Intake Score (FOIS) (5.5 vs. 3.3, p < 0.001) at 2 weeks after completion of treatment.33 At 12 months, the TORS group had returned to baseline swallowing status while diet and FOIS remained impaired in the CRT group. In a series of 45 patients, Moore et al. found that only 5 of 22 patients who had gastrostomy tubes required their use beyond 20 days and all patients had their feeding tubes removed by 4 months.9 Dean et al. compared feeding tube dependence in patients undergoing TORS to those who had open surgery for post-CRT OPSCC failures and found that while 43% of the open salvage group were G-tube dependent at 6 months, none of the TORS patients required feeding tube supplementation. These early evaluations of the oncological and functional outcomes of TORS led to FDA approval of TORS
for use in selected benign and malignant (T1/T2) tumors of the head and neck in December 2009.
for use in selected benign and malignant (T1/T2) tumors of the head and neck in December 2009.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree