Surgical Technique
William Ignace Wei
Jimmy Yue Wai Chan
INTRODUCTION
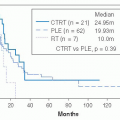
The primary treatment modality for cancer of the nasopharynx is radiotherapy for early-stage diseases and concomitant chemotherapy and radiation for advanced-stage diseases. Surgical resection of cancer of the nasopharynx is only applicable when the cancer persists or recurs after the initial treatment.1 For a group of 246 patients who underwent salvage nasopharyngectomy with a median follow-up of 38 months, the 5-year actuarial control of disease was 74% and the 5-year disease-free survival was 56%. Tumor size of <1.5 cm and negative resection margins were the two independent factors that affected the local tumor control and survival.1
The nasopharynx is located at the central skull base that anatomically is in the centre of the head and it is >10 cm from the skin surface from all directions. It is difficult to expose this region adequately for surgical resection of the tumor comfortably; this is particularly so when the lesion is malignant and has potential to infiltrate nearby structures.
Currently, there are two surgical techniques commonly employed for the resection of cancer of the nasopharynx.
Maxillary swing approach to expose the nasopharynx and the central skull base so that the malignant tumor in the region can be resected with adequate margin.2
The palate was split to expose the cancer in the nasopharynx and the tumor resection was carried out with the Da Vinci Robot.3
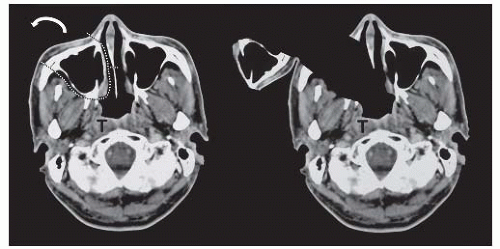
The maxillary swing approach originated from the observation that during maxillectomy for carcinoma of the maxillary antrum, the nasopharynx was widely exposed when the maxilla bone was removed. The anterolateral approach to the nasopharynx was thus developed; the maxillary antrum including the lateral walls and the floor attached to the anterior cheek flap could be swung laterally as an osteocutaneous flap to expose the pathology in the nasopharynx. After removal of the pathology, the maxillary antrum was returned to its original position and fixed to the rest of the facial skeleton (Fig. 22-26).
The surgical approach involves a Weber Ferguson facial incision as in maxillectomy, incision on the palate, osteotomies of the anterior wall, medial wall of the maxillary antrum, and lower portion of the zygomatic arch. The pterygoid plates are also separated from the maxillary tuberosity. This anterolateral approach exposed the nasopharynx and its vicinity from the side of the swing. With the removal of the posterior part of the nasal septum, the contralateral nasopharynx can be exposed. Persistent or recurrent cancer of the nasopharynx after chemoradiation can be removed adequately, and if there are paranasopharyngeal lymph nodes, these can be resected under direct vision. With the wide exposure of the nasopharynx and its vicinity following the maxillary swing approach, the internal carotid artery lying in the paranasopharyngeal space could be identified with palpation and vision, thus avoiding its injury during tumor extirpation; this is particularly important during the dissection of the paranasopharyngeal lymph node.4 A microvascular free flap could also be employed to cover the exposed vessel and the raw area following removal of tumor in the nasopharynx. With this additional new vascular supply, further adjuvant therapy could then be considered.5
The morbidity associated with the operation was acceptable. The facial scar usually heals well and becomes less obvious with time. The development of significant trismus in patients who had previous radiation could be managed with passive mechanical stretching and this frequently improves the trismus. With the resection of the Eustachian tube, the patient develops serous otitis media on the side of the swing and this results in deterioration of hearing acuity.
The Da Vinci Robot have been reported for the resection of recurrent nasopharyngeal carcinoma. With the splitting of the palate, the tumor in the nasopharynx is exposed. It is, however, difficult to employ the ordinary instruments to resect the tumor en bloc with a good resection margin. With the versatility of the endowrist of the Da Vinci Robot and the 3D camera, adequate resection is possible with splitting of the palate. The location and the size of the tumor are determinants for a successful resection. Those tumor of around 1 cm diameter, not deeply infiltrative and located in posterior wall, not extending laterally beyond the floor of pharyngeal recess, have a better chance of being resected completely with the robot. The morbidities associated with this split palate approach are limited, patient might develop palatal fistula as the patient had previous radiation with or without chemotherapy. Exposure of the raw area in the nasopharynx following resection might lead to the development of osteoradionecrosis of the skull base bone.
PREOPERATIVE PREPARATION AND ANAESTHESIA
For patients undergoing the resection of persistent or recurrent cancer in the nasopharynx, full cardiopulmonary assessment is essential to evaluate whether he or she can stand the procedure
as the blood loss might occasionally be significant, especially with the maxillary swing procedure. The interalveolar distance should be at least 3 cm wide as otherwise it is difficult to raise the palatal flap transorally and to insert the curved osteotome to separate the pterygoid plates from maxillary tuberosity. A significant degree of trismus will also prevent the insertion of the robotic arm transorally for tumor resection. The interalveolar distance also prompts the anaesthetist to consider the appropriate route to insert the endotracheal tube. An upper alveolar dental plate is fabricated for each patient before the maxillary swing procedure; this is used to clip onto the teeth on the upper jaw upon return of the swung maxilla, ensuring correct repositioning and precise dental alignment.
as the blood loss might occasionally be significant, especially with the maxillary swing procedure. The interalveolar distance should be at least 3 cm wide as otherwise it is difficult to raise the palatal flap transorally and to insert the curved osteotome to separate the pterygoid plates from maxillary tuberosity. A significant degree of trismus will also prevent the insertion of the robotic arm transorally for tumor resection. The interalveolar distance also prompts the anaesthetist to consider the appropriate route to insert the endotracheal tube. An upper alveolar dental plate is fabricated for each patient before the maxillary swing procedure; this is used to clip onto the teeth on the upper jaw upon return of the swung maxilla, ensuring correct repositioning and precise dental alignment.
Preoperative evaluation of the extent of persistent or recurrent cancer of the nasopharynx is mandatory before surgical resection. In addition to a full clinical examination, an endoscopic examination of the nasal cavities, the nasopharynx, and the oropharynx together with a cross-sectional imaging study such as computed tomography or magnetic resonance imaging is required to determine the extent of the cancer in the nasopharynx. Magnetic resonance imaging with contrast evaluates the proximity of the tumor to the internal carotid artery and possible involvement of soft tissue in the regions, such as the paranasopharyngeal lymph nodes. Computed tomography with bone window should be carried out to see whether the clivus or skull base bone is affected. For more extensive tumor in the nasopharynx or patients with both recurrent tumor in the nasopharynx and cervical lymph nodes, a positron emission tomography is indicated to rule out distant metastasis.
SURGICAL TECHNIQUE
Maxillary Swing Procedure
The operation is carried out under general anesthesia with the patient in supine position. The head is placed on a soft head ring to allow mobility and there is no need for any support behind the shoulders to extend the neck, unless a neck dissection or neck exploration is also planned. Endotracheal intubation is carried out through the mouth if possible as this avoids disturbance of pathologies in the nasopharynx. A temporary tracheostomy is then carried out and the endotracheal tube is withdrawn. The tracheostomy is optional as the procedure can be carried out with the transoral endotracheal tube in position. The presence of the tube, however, interferes to a certain extent the raising of the palatal flap and the osteotomy of the hard palate.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree