Introduction
Stroke is the leading cause of severe disability in most of the developed world. The World Health Organization (WHO) estimated that in 2002, 15.3 million people had a stroke worldwide, with more than one-third, 5.5 million, resulting in death.1 Population projections for Europe suggest that the proportion of the population aged 65 years and over will increase from 20% to 35% by 2050, and this demographic shift will increase the number of acute stroke episodes from 1.1 million to more than 1.5 million per year by 2025.2 In addition to a high mortality, stroke is also associated with significant disability amongst survivors. Nearly 40% of stroke survivors had severe and 20% had moderate disability, which consumed nearly one-third of all healthcare resources in a large community study in patients over 80 years of age.3 Stroke is also an expensive disease. The estimated average cost of a stroke varies between countries and the average ranged from US$468 to $146 149 in a review of 120 studies across the world.4 The average cost of stroke varied between $2822 in Eastern Europe and $12 883 in Japan to $22 377 in the UK, $24 548 in Sweden and $28 253 in the USA.5 These costs do not take informal costs of care into account; when such costs are included, the total cost of stroke nearly doubles.6 An estimation of total costs of stroke using a long-running community-based South London Stroke Register estimated that stroke costs in the UK totalled  9 billion per year with productivity losses due to morbidity and mortality accounting for
9 billion per year with productivity losses due to morbidity and mortality accounting for  1.3 billion.7
1.3 billion.7
Recent years have seen several developments to improve the management of stroke patients and reduce mortality, disability and costs associated with this disease. These range from advances in imaging techniques which improve diagnostic capabilities8 and acute interventions aimed at reducing the size of brain injury9 to improved acute care10 and organized rehabilitation aimed at reducing residual dependence.11 Despite the proven efficacy of thrombolysis and optimism about physiological manipulations in the acute phase of stroke, these interventions will have only a modest impact on eventual outcome in most stroke patients because of the limitations on their use.12 On the other hand, over 300 randomized controlled trials provide a sound foundation for evidence-based practice in stroke rehabilitation, supplementing and often confirming decades of clinical experience.13 Hence early and planned multidisciplinary rehabilitation remains the cornerstone of stroke management in the foreseeable future because it is applicable to most stroke survivors and has a strong evidence base for effectiveness in all patients, regardless of stroke severity.
The Neurological Basis of Recovery
The principle that underlies all rehabilitation is that the brain has an inherent capacity to recover lost function after stroke.14 This is based on observations that most survivors regain some or many of the functions initially lost as a result of the stroke. Recovery is of two types: intrinsic, which involves neuronal regeneration and setting up of new axonal connections, and adaptive, in which alternative strategies, usually behavioural changes, are used to overcome disability.15 The majority of patients show both intrinsic and adaptive recovery, the proportion of each being dependent upon factors such as age, severity of stroke, cognitive abilities and rehabilitation input after stroke. Intrinsic mechanisms consist of restitution, which includes repair of partially damaged pathways, and strengthening of existing pathways, mediated by local changes in blood flow, neurogenesis and cell migration, growth factor release, metabolism or neurotransmitter concentrations. Diaschisis or substitution is the development of new, but functionally related, pathways in the unaffected areas of the brain to take over the lost function. Studies in experimental models have shown a number of cellular and histological changes, such as axonal sprouting and formation of new dendritic connections, in the unaffected hemisphere of chronic stroke models, which probably are responsible for long-term recovery in these animals.16 The degree of recovery due to intrinsic mechanisms is variable and may be incomplete in a significant number of patients. In these circumstances, re-education in compensatory techniques, either by changed use of the affected side or retraining of the unaffected side, becomes an important behavioural adaptation to improve function and reduce the level of disability posed by the impairment.17
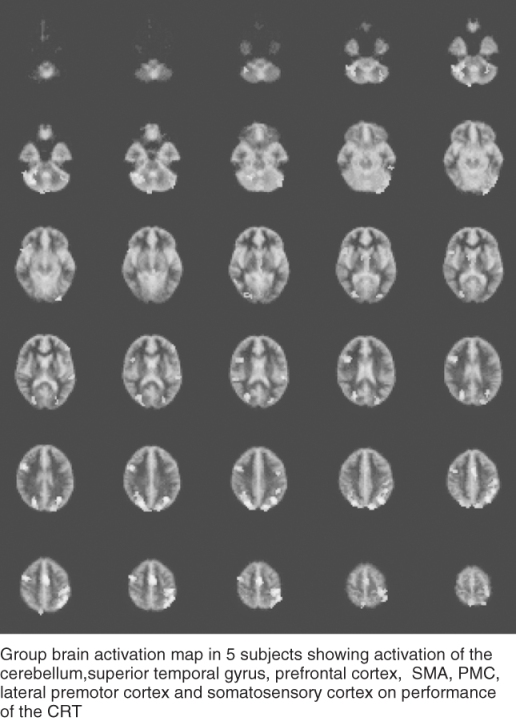
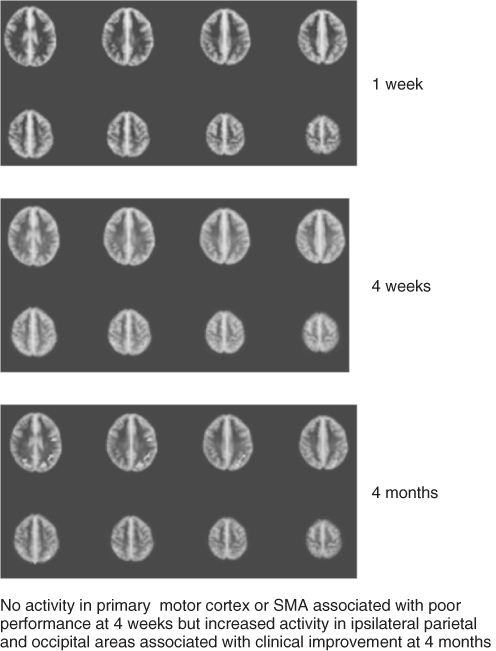
The development of advanced neuroimaging techniques, such as positron emission tomography (PET) and functional magnetic resonance imaging (MRI), has helped to demonstrate the processes of reorganization of neural activity after stroke in human subjects.18 These studies have shown that unilateral motor tasks are associated with activation (increased metabolic activity) primarily in the contralateral sensorimotor cortex and the ipsilateral cerebellum in healthy subjects (Figure 58.1). The contralateral premotor cortex, ipsilateral somatosensory cortex and bilateral supplementary motor areas also participate in hand and finger motor tasks, particularly when the task increases in complexity. In recovered stroke patients, activation on these tasks is seen in the peri-infarct cortex and supplementary areas of the affected side (Figure 58.2) and also in additional regions including the ipsilateral sensorimotor and premotor cortex (Figure 58.3). The cerebellum, thalamus and prefrontal areas play an important part in restoration of function. The process of reorganization is dynamic, there is an evolution of changes with time and several different patterns have been described. These include activation, and later extinction, of bilateral cerebellar and prefrontal areas, an initial increase followed by a decrease in activation of motor areas and progression from early contralesion activity to late ipsilateral activity.19–22 All these changes appear to be associated with recovery, although their exact significance and relevance to recovery remain a subject of debate. It is now clear that there are multiple motor circuits in the brain which serve similar functions. Conventional pathways dominate in healthy subjects and inhibit the activity of alternative pathways in other areas of the brain. Disruption of traditional pathways in cerebral ischaemia reduces or eliminates the inhibition normally exerted by these pathways and allows activation of alternative pathways in the premotor areas of the affected side and primary motor areas on the unaffected side. Hence the paradigm for function has shifted from strict cerebral localization to that of interactive functioning of diverse cortical areas activated by the constantly changing balance of inhibitory and excitatory impulses.
Figure 58.2 FMRI on CRT using affected hand in a patient with small lacunar infarct in the left internal capsule.
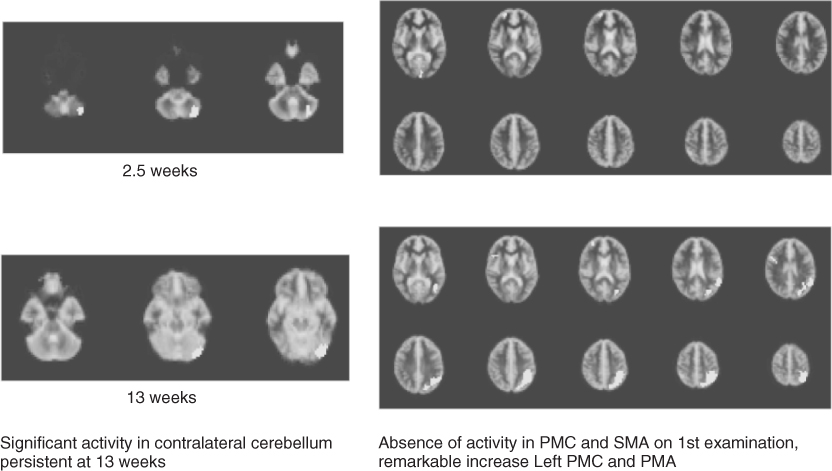
Figure 58.3 FMRI on CRT using affected hand in a patient with cortical infarct in the right hemisphere.
New evidence suggests that neurogenesis represents a key factor in plasticity of the normal brain in response to environmental stimuli and that newly generated nerve cells form synaptic contacts which become fully integrated into existing neuronal circuitry.15, 23 Stroke-induced neurogenesis takes place in the subventricular zone and ischaemic boundary of adult human brains and has been demonstrated even in elderly patients up to 90 years of age.24 Ischaemic injury to the brain sets up orchestrated waves of cellular and molecular events characterized by a reduction in growth-inhibitory molecules and activation of growth-promoting genes by neurons. Angiogenesis appears to be the first step in regeneration, closely followed by the production and migration of neural progenitors.25 Neural progenitors interact with other cells such as the astrocytes and oligodendrocytes and other growth factors, creating a microenvironment which promotes neurite outgrowth that repair damaged connections or establish new signalling pathways.25
An important concept in rehabilitation is that of ‘brain plasticity’, which implies that it is possible to modulate or facilitate reorganization of cerebral processes by external inputs.23, 26 This concept is supported by studies which show that activation can be facilitated by sensory stimulation, repetitive movement of the affected limbs or the use of drugs which modify neurotransmitter release.27–29 Absence of adequate external inputs may have a negative effect—primate studies have shown that lack of afferent stimulation because of loss of voluntary activity impedes recovery in function after induced ischaemic injury to the brain.30, 31 The timing and intensity of intervention may also be important. Although some studies have suggested that very early attempts at intensive movement training in experimental models result in an increase in the size of the cortical lesion,32 the bulk of evidence supports the benefits of early initiation of rehabilitation in animal models.33 This emerging picture fits in well with theoretical concepts about motor learning, which emphasizes the importance of repetition, attention and goal-directed activity.
The observations made in animal experiments provide increasing support for some of the basic underpinnings of stroke rehabilitation, that is, that the earlier rehabilitation is started the better the recovery is, that greater intensity of treatment translates into greater recovery and that improvement can continue for some time after discharge from hospital or rehabilitation centre.34 Feys et al., using a randomized controlled design, showed that adding an early, repetitive and targeted stimulation to the arm during the acute phase after a stroke resulted in a clinically meaningful and long-lasting effect on motor function in patients, even after 5 years of observation.35 A meta-analysis of the effects of augmented exercise therapy after stroke has shown that such treatment has a small but favourable effect on activities of daily living (ADLs) within the first 6 months after stroke.36 Intensive language training has been shown to improve language functioning significantly and this correlated with cortical perilesional reorganization or plasticity.37 In an observational study, Bode et al.38 investigated the importance of therapy content and intensity after controlling for stroke severity and found that content and amount of therapy are important predictors of greater than expected gains in self-care and cognition. A small functional MRI study demonstrated that drugs can modify reactivation and recovery; a single dose of fluoxetine resulted in significantly greater activation in the ipsilesional primary motor cortex and significantly improved motor skills on the affected side in patients with pure motor hemiparesis.39
To summarize, advances in basic sciences and clinical research are beginning to merge and show that the human brain is capable of significant recovery after stroke, provided that the appropriate treatments and stimuli are applied in adequate amounts and at the right time. There is also evidence to suggest that advances in pharmacotherapeutics and robotic assistive technology can further enhance and hasten the process of recovery, and will change the focus of rehabilitation from intuitive methods employed at present to new strategies firmly rooted in the neuroscience of recovery.
Patterns of Recovery
Recovery is fastest in the first few weeks after stroke, with a further 5–10% occurring between 6 months and 1 year. About 30% of survivors are independent within 3 weeks and by 6 months this proportion rises to 50%.40 Late neurophysiological recovery can continue for several years but is at a much slower rate and seldom results in dramatic changes in overall functional ability.41 Completeness of recovery depends largely on the severity of the initial deficit. The more severe the initial deficit, the less likely is it that complete recovery will occur. The pattern of recovery is not uniform and shows considerable variation between individuals and also between different deficits in the same individual. There is currently no validated method for predicting the precise mode or degree of recovery for a given individual. In addition, there can be considerable variation in day-to-day progress of individual patients, which may mask overall recovery or at times give rise to false optimism. This problem can be overcome by monitoring patients over time, as overall trends are more important than ‘one-off’ assessments. Recovery may be affected adversely by the development of stroke-related complications. Comorbidity in elderly patients is another variable that affects overall recovery and rehabilitation.
The rate of recovery varies for different impairments and disabilities. Some problems, such as homonymous hemianopia, dysphagia and sitting balance, resolve very quickly in stroke survivors, whereas arm paralysis and language impairment recover more slowly and less completely. Perceptual problems may persist or take a very long time to recover. If all stroke survivors are considered, 62% are independent in self-care at 3 months and 66% at the end of 1 year, despite the persistence of neurological deficit in some patients.42
Objectives of Rehabilitation
Rehabilitation in stroke is not simply a matter of being treated by a therapist or a group of therapists but involves a whole range of approaches to managing disability, provided by a coordinated multidisciplinary team and tailored to restore patients to their fullest possible physical, mental and social capability.43 The goals of rehabilitation are to:
- maximize patients’ role fulfillment and independence in their environment within the limitations imposed by underlying impairment and availability of resources;
- make the best possible physical, psychological and social adaptation to any difference between the roles desired and the roles achieved following stroke;
- ensure the long term wellbeing and quality of life of stroke survivors and their families by providing the necessary knowledge, skills and support using a range of health, social and voluntary services resources.
An important objective of the rehabilitation process is to monitor the relevance, quality and effectiveness of the services provided in order to ensure that they meet the expectations of patients and their families and obtain the best possible value for the money and effort being expended.
The revised WHO International Classification of Impairments, Disabilities and Handicaps (ICIDH) provides a conceptual model for stroke rehabilitation.44 In this model, the terms disability and handicap have been replaced by limitations in activities and restriction in participation. The focus of attention shifts from pathology to handicap and from patient to environment during the course of rehabilitation.45 The key areas that rehabilitation impacts upon are limitation of activity (disability) and restriction of participation (handicap). Disability is the lack of ability to perform an activity in the manner, or within the range, that the person was able to accomplish prior to the stroke and relates to function. In this context, the ability to undertake basic activities of self-care is fundamental to any physical rehabilitation programme. Handicap is the social consequence of disability and constitutes the limitations faced by stroke patients in fulfilling their normal role in society. It is not always possible to differentiate handicap from disability and most pragmatic approaches tend to combine these two dimensions, referring to them as social disability.
Rehabilitation in stroke is essentially a multidisciplinary activity, which has been described as a problem-solving educational process focusing on disability and intended to reduce handicap.46 The basic principles that should be applied throughout rehabilitation of stroke patients are:
- documentation of impairments, disabilities and handicaps and, where possible, measuring them using simple, valid scales;
- maximization of independence and minimization of learned dependency;
- adopting a holistic approach to patients that takes into account their physical and psychosocial background, support mechanisms and environment;
- supporting caregivers and helping them to develop physical and psychological skills to provide long-term, sustainable support to stroke patients.
Process of Rehabilitation
Rehabilitation has four important components: assessment, planning, intervention and evaluation.
Asessment
Assessment is fundamental to ascertain the precise nature and severity of deficits and define treatment goals prior to commencement of a rehabilitation programme because it provides a logical basis for treatment and management of stroke patients. The major reasons for undertaking assessments in stroke patients are to:
- define the type of patient, the extent of disability and the potential for recovery and/or responding to intervention (prognostication);
- identify main areas of difficulty and their underlying causes and also the expectations of the patient and the family;
- monitor the process of rehabilitation (evaluation) and assess the degree of recovery or residual disability at the end of the rehabilitation process (outcome).
A large number of neurological, physical and functional assessments are currently available and can be divided into global assessments (which determine the overall impact of stroke) and specific assessments (which deal with a single level or domain of impairment or disability). Composite scores for global disease severity are unreliable because of the dominance of speech and language function over other indexes and because, when very different disabilities are combined into one score, much specific information is lost.47 Most scores also mix a variety of impairments and disabilities without considering their interactions.
The importance of knowing what information is wanted and why, that is, the purpose of a measure, is central to choosing any measure in rehabilitation. It is also important to decide on the least amount of information needed to achieve this purpose. The necessary characteristics of suitable measures are validity, reliability, sensitivity, simplicity and communicability. It is best to use existing measures wherever possible provided that they are valid for the purpose in mind, reliable in the circumstances proposed and relevant to the objectives of intervention. Moreover, the use of established measures makes communication and interpretation of data easier.
Predicting when a stroke patient has reached their full potential for recovery and may not benefit from further therapy inputs is an imprecise science. Estimation of the functional capacity for recovery is particularly important for chronic stroke patients (more than 1 year after stroke), especially as these are the patients most likely to be denied further rehabilitation inputs. Unfortunately imaging and electrophysiological techniques to aid such predictions have generally proven to be expensive and unhelpful in clinical practice. However, it may be possible to combine these modalities to develop algorithms for patient selection for both research and clinical programmes. A recent example of this is the combined use of transcranial magnetic stimulation (TMS) and MRI to determine the integrity of corticospinal tracts and predict functional recovery potential.48 The study showed that motor evoked potentials to TMS in the affected limb in the presence of little or no asymmetry in the fractional anisotropy map of the internal capsule on MRI (indicative of minimal long tract damage) was associated with a potential for improvement up to 3 years after stroke.
Planning
Planning is the process of goal setting based on identification of aims, objectives and targets.49 Goals can be set at different levels; most patients will have immediate goals which relate to basic personal ADLs such as achievement of sitting balance, independent transfers and independence in toiletting activities. As patients continue to improve, goals need to be set for higher levels of function which incorporate not only independence in household activities but also the ability to undertake social, leisure and occupational pursuits. The ultimate goal of the rehabilitation programme is to improve overall wellbeing and participation, but many rehabilitation programmes often stop once patients have achieved independence in personal ADLs. It is important that planning takes into account not only the immediate needs of the patients but also their potential needs when they return to their own environment. This often involves adapting rehabilitation to the home setting and addressing the needs of caregivers, many of whom will play an important role in providing ongoing support and management of disability at home.50 The areas of practical importance in goal setting are:
- Accommodation: Where will the patient live and what physical adaptations will be needed?
- Personal support: What is the level of support available for existing caregivers and what extra help will be essential for the patient?
- Life satisfaction: What roles will the patient be fulfilling within their social setting and how will they be occupying their time?
Many difficulties arise in stroke rehabilitation because the goals of intervention are not set in advance or because these goals have not been discussed and agreed on by all relevant parties. Goals of rehabilitation vary according to the expectations of those involved. The goal of hospitals may be to discharge patients as soon as possible, whereas the goal of patients may be to return to their previous functional status even if this is unattainable. The goal of caregivers may be to minimize the level of input that they need to provide even at the cost of institutionalization. Many of the difficulties ultimately faced in managing patients and in evaluating the effectiveness of interventions can be traced back to conflicts between the goals and objectives of different parties. An essential function of the whole rehabilitation team is to identify and modify unrealistically high (and sometimes unjustifiably low) expectations of patients and their families by making them more aware of the nature of residual deficit and expected prognosis as soon as these are reasonably clear. The two major problems that arise in goal setting include failure to use a common language in communication between various professionals or between professionals and patients and, second, failure to agree on a time frame within which the rehabilitation process must be accomplished.
Intervention
The minimum requirement of any stroke intervention is to provide care necessary to maintain the status quo and prevent deterioration of the patient’s condition or functional ability due to poor management or complications. Further intervention should be aimed at facilitating recovery and improving outcome by minimizing disability and preventing handicap. Although large amounts of time and resources are devoted to various therapy interventions after stroke, evidence suggests that these resources are not used optimally in many settings and many of the potential gains of therapy input are not realized because of organization and systems limitations.51, 52 There is also limited evidence on individual interventions because despite the large number of studies available, most of them have small and heterogeneous samples, small amounts of formal therapy have been given in any trial and the interventions most often become a comparison between different intensities of treatment. In addition, there is considerable diversity of outcome measures used in these studies and limited comparability of study designs.53
At present, there are many rehabilitation techniques available, some with more robust evidence than others in trial conditions, but none that have been shown to be superior to any other in the major areas of physical therapy or in speech and language function in clinical practice. A summary list of current approaches is given in Table 58.1 and some of the more commonly used approaches are summarized.
Table 58.1 A summary of rehabilitation techniques in stroke.54.
|
Early Mobilization
Early mobilization is a key rehabilitation strategy associated with good functional outcomes in several observational and controlled studies.55 Despite this, mobilization protocols remain poorly defined and vary across units and across patients. A review which combined data from observational studies and meta-analyses was not able to find any positive, unequivocal benefit associated with early mobilization, independent of other aspects of stroke care,56 but concluded that early mobilization after stroke was not harmful for most stroke patients and may contribute as part of the routine stroke unit in achieving good long-term outcome in stroke patients.
Restoration of Motor Function
Restoration of motor function is a primary objective of stroke rehabilitation and there are several pooled data analyses of studies on various strategies for improving motor performance in stroke patients.57 A prospective meta-analysis of the effectiveness of bilateral movement training in post-stroke motor rehabilitation showed that bilateral movements alone or in combination with auxiliary sensory feedback were effective in improving functional and mobility outcomes in stroke patients.58
Treadmill training has been shown to improve gait and walking speeds significantly in hemiparetic patients when used as an adjunct to conventional treatment. There are many approaches to gait training, but the most effective combination of training parameters, such as amount and timing of body support during the gait cycle, belt speed and acceleration, remains unknown.59
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree