Age-Related Hepatobiliary Changes
Liver
Traditionally, hepatic biochemical parameters such as serum transaminases, hepatic alkaline phosphatase, γ-glutamyltranspeptidase and serum bilirubin are considered indices of liver function. These parameters, which are indeed more reflective of disrupted hepatocyte integrity and liver dysfunction, are not altered with ageing (James, 1997; MacMahon and James, 1994). However, there is an age-related compromise in more objective and sophisticated dynamic liver function indices. Available data show that with ageing hepatic volume and perfusion may decrease by approximately 30%. Other indices of hepatic metabolic function, such as nitrogen synthesis and aminopyrine clearance, also decrease with ageing. Likewise, age-related reduction in hepatic microsomal cytochrome content may compromise efficient drug metabolism in the elderly (Wynne et al., 1989; Fabbri et al., 1994; James, 1997).
Histological studies have identified decreased smooth endoplasmic reticulum and fewer mitochondria in hepatocytes from older adults (Schmucker, 1990) Age-related reduction in hepatic regeneration is particularly concerning. Several studies suggest that the older liver is more vulnerable to stress, perhaps due to an age-related reduction in mitogen activated protein kinase activity (Liu et al., 1996). These cellular changes contribute to the poorer outcomes observed in older adults following hepatic insult.
Few studies have specifically examined the effect of ageing on the gallbladder and biliary tract. With ageing, there is an increase in the diameter of the common bile duct, due to replacement of biliary ductal myocytes with connective tissue cells (Kialian and Aznaurian, 1995).
In addition, the lithogenicity of bile increases, resulting in an increased tendency to form cholesterol and calcium bilirubinate stones (Siegel and Kasmin, 1997). These preceding changes, set against a background of lifetime exposure to potentially hepatotoxic agents, set the stage for hepatobiliary disease as a major contender in geriatric medicine.
Hepatic Diseases of the Elderly
Viral Hepatitis
Classically, viral hepatitis is defined as hepatic inflammation induced by infection with specific hepatotrophic viruses. Histological features include diffuse or patchy necrosis of the liver acini. Severity of clinical presentation is variable. Some patients are asymptomatic, while others may complain of flu-like and fairly non-specific symptoms such as myalgia, athralgia, anorexia, nausea, vomiting and diarrhoea. Physical examination may reveal fever, jaundice, hepatomegaly and, in some cases, cutaneous manifestations such as purpura, urticaria and other skin lesions.
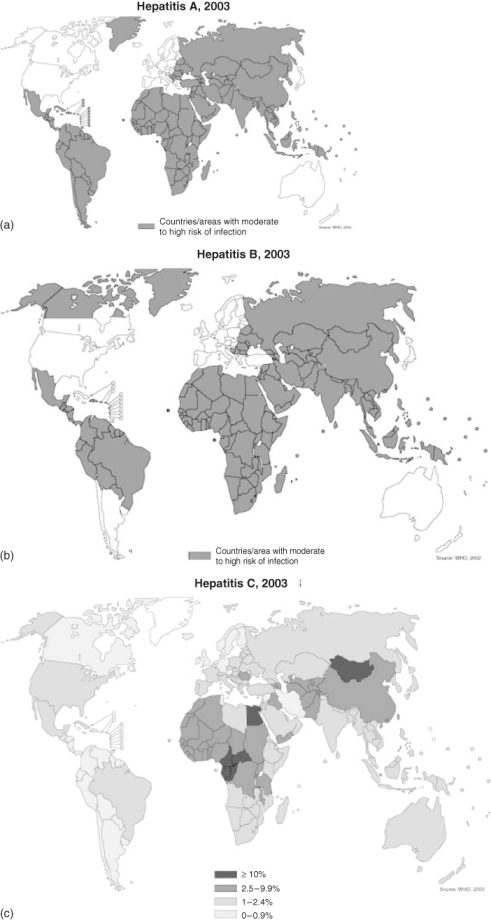
Geographical distribution and prevalence of viral hepatitis vary with the infecting agent (Figure 23.1).
Hepatitis A Virus
Hepatitis A virus (HAV) is a 27 nm single-stranded, non-enveloped RNA picornavirus. Although infection typically occurs by faecal-oral transmission, a few cases of HAV have occurred through haematogenous transmission (Centers for Disease Control and Prevention, 1999). Onset of symptoms is usually 2–6 weeks after exposure. In younger adults, hepatitis A infection is usually subclinical with mild symptoms.
Jaundice is present in less than 10% of cases. In contrast, although hepatitis A infections are less frequent in older adults, symptoms are likely to be more severe. In addition, the risk of developing and dying from complicating fulminant liver failure is far more common in infected elders. Reported case fatality rate among patients over the age of 65 years is 4% compared with 0.07% in patients aged 15–24 years (Forbes and Williams, 1988). Current recommendations state that older persons travelling to endemic areas should receive HAV vaccination. Additionally elderly food handlers and patients with chronic liver disease are also advised to receive HAV vaccination, although data regarding the efficacy and cost-effectiveness of the vaccine in older adults are lacking (James, 1997).
Hepatitis B Virus
Hepatitis B virus (HBV) is a 42 nm double-stranded, enveloped DNA hepadna virus. HBV is a highly infectious virus transmitted through sexual intercourse or contact with infected blood, blood products and saliva. Vertical maternofetal transmission also occurs during childbirth. The incubation period of HBV is approximately 120 days (Lok and McMahon, 2001). Although most infections occur in young adulthood, serological evidence of HBV infection is threefold higher among older adults aged between 64 and 74 years. Rates of HBV infection are also higher among nursing home residents compared to those in community dwelling elders. Sporadic outbreaks of HBV infection in nursing home residents have been linked to inappropriate sharing of razors and bathing appliances. Data indicate that in older adults who contact HBV, the risk of progressing to chronic hepatitis is over 50% compared with 5% following acute infection in younger adults. Nevertheless, acute hepatitis B is rare among older adults, and older adults with acute HBV infection are usually only mildly symptomatic (Marcus and Tur-Kaspa, 1997; Reeder and Halket, 1987). Nevertheless, age remains a risk factor for the development of life-threatening fulminant hepatitis. Perhaps as a result of more prolonged exposure, older adults with HBV infection are more likely to develop hepatocellular carcinoma and liver cirrhosis (Beasley, 1988; MacMahon and James, 1994).
Hepatitis C Virus
Hepatitis C virus (HCV) is a 55 nm enveloped RNA flavivirus, with an incubation period ranging from 15 to 90 days. Of the six known genotypes, type 1 is the most common in the United States. Although transmission is primarily haematogenous, a few cases have been transmitted through saliva and human bites (Bukh et al., 1995; Chu et al., 2002). Data indicate that the prevalence of acute HCV infection among older adults equals, and, in some cases, surpasses that in the general population. Within the United States, reported seroprevalence rate among adults aged over 70 years is 1%, compared with 1.8% among the general population (Alter et al., 1999). In an Italian cohort aged over 65 years, the HCV infection prevalence rate was over 4% compared with 3.2% among a comparable cohort of young subjects (Monica et al., 1998). Although the incidence of new cases has declined over the past decade, projections indicate that over the next 20–30 years the prevalence of HCV among older adults will increase significantly.
As in younger adults, infection with HCV in elders is only mildly symptomatic during the acute phase. However, the clinical course in older patients is much more aggressive and lethal. Similarly, advanced age at diagnosis of the disease portends more rapid progression to fibrosis and cirrhosis (Seeff, 1997; Watson et al., 1996). Other risk factors for the development of cirrhosis include alcohol use and obesity. Studies show that in patients who acquire HCV over the age of 60 years the risk of developing cirrhosis is reported to be as high as 46%, compared to approximately 7% among patients in the fourth decade of life. Reasons for the aggressive clinical course with ageing are not clearly known, although age-related immunocompromise has been proffered as a likely theory (Simmonds et al., 1996).
Hepatitis D Virus
Hepatitis D virus (HDV) is a single-stranded RNA viroid that is dependent on the HBV envelope protein for replication and pathogenicity. Transmission of HDV occurs haematogenously or through sexual contact and results in either coinfection or superinfection. Coinfection occurs when there is simultaneous transmission of both HDV and HBV, while superinfection refers to HDV infection of a previously HBV positive patient. Patients with coinfections have a better prognosis and progress to chronic disease in less than 5% of cases. In contrast, 70–90% of superinfected patients develop cirrhosis. Although HDV infection causes less than 5% of chronic hepatitis, it accounts for approximately 7500 new infections annually and has a mortality rate of 30% (Alter and Hadler, 1993). Data in older subjects are lacking.
Hepatitis E Virus
Hepatitis E virus (HEV) is a single-stranded RNA calicivirus that is transmitted feco-orally. This virus tends to infect younger adults and is rare in developed countries. Characteristically, pregnant women have a 20% mortality rate from this disease compared with 1% in the general population.
Older people travelling to endemic regions such as Asia, Mexico and Africa may be at risk. Prophylaxis is ineffective and the avoidance of consumption of foods and water that may be contaminated is strongly recommended (Gilchrist, 1999).
Hepatitis F Virus
Viral particles identified in the stool of post-transfusion, non-A, non-B, non-C, non-E hepatitis cases and injected into Indian rhesus monkeys caused acute hepatitis with elevated transaminases. Consequently, this viral enteric agent was named hepatitis F virus (HFV). However, to date there are no convincing corroborating scientific reports. Although sporadic cases in humans may have been identified in Europe, United States, and India, the validity of this virus remains questionable (Deka et al., 1994).
GB Virus Type C (GBV-C)
This virus belongs to the Flaviviridae and was previously referred to as hepatitis G virus (HGV). Currently, the lack of proven association of this virus with either acute or chronic hepatitis has discouraged the use of the name HGV (Dickens and Lemon, 1997). The name GBV-C was derived from a surgeon, whose initials were GB, after marmosets inoculated with his serum developed hepatitis. On the basis of this single observation, the surgeon was erroneously thought to have post-transfusion hepatitis. Later evidence did not support this diagnosis (Almeida et al., 1976). Indeed, GB virus type C (GBV-C) infection is common, but is yet to be associated with definite pathogenicity (Dickens and Lemon, 1997). Currently, the major clinical significance of this agent lies in the fact that HIV-positive patients infected with GBV-C may have prolonged survival (Xiang et al., 2001). Few data exist regarding the pattern of GBV-C infection in ageing adults.
Transfusion Transmitted Virus
Transfusion transmitted virus (TTV) is a single-stranded DNA virus. Despite the name, feco-oral transmission of the virus also occurs. Infection is usually acquired in childhood and may persist for years. Its role in causing hepatitis or other diseases has not been proven. Even though one of the genotypes of TTV is suspected to cause hepatitis, the pathogenicity of TTV in humans remains poorly defined (Takacs et al., 2003). The prevalence of TTV is also unclear. Available data indicate that the virus has been identified in 1% of blood donors, 18% in post-transfusion subject, 15% of patients with liver cirrhosis and 27% in patients with end-stage liver failure (Naoumov and Petrova, 1998). Notably, high TT virus load has been found to be independently associated with the occurrence of hepatocellular carcinoma among patients with HCV-related chronic liver disease (Nishizawa and Okomoto, 1997).
Autoimmune Hepatitis
Autoimmune hepatitis is characterized by severe chronic hepatitis in the presence of circulating autoantibodies. Characteristically, there is frequent progression to liver cirrhosis. Originally described as a disease of young women, autoimmune hepatitis is now known to affect all age groups and both genders. Approximately 20% of all patients diagnosed with autoimmune hepatitis are over the age of 65 years (Newton et al., 1997). Diagnostic criteria for autoimmune hepatitis are unchanged with age, and the prognosis for affected older adults is no worse than for younger adults (Table 23.1). Nonetheless, older adults present with less acute symptoms, but are more likely to have severe histological inflammation and necrosis. Unfortunately, data indicate that older adults are less likely to be prescribed immunosuppressive therapy, even though this has been shown to prolong survival in patients with severe disease. There are no data to support the benefits of therapy in older adults with mild disease (Czaja and Freese, 2002).
Table 23.1 Diagnostic criteria for autoimmune hepatitis (Alvarez et al., 1999; Czaja and Freese, 2002).
| Criterion | Definite | Probable |
| Genetic liver disease | Normal α1-antitrypsin, ceruloplasmin, iron and ferritin levels | Partial α1-antitrypsin deficiency, non-specific serum copper, ceruloplasmin, iron and ferritin abnormalities |
| Viral infection | No markers of current infection with HAV, HBV, HCV | No markers of current infection with HAV, HBV, HCV |
| Toxic or alcohol injury | Daily alcohol <25 g day−1 and no recent use of hepatotoxic drugs | Daily alcohol <50 g day−1 and no recent use of hepatotoxic drugs |
| Laboratory features | Predominant serum aminotransferase abnormality, globulin, gamma-globulin or immunoglobulin G level >1.5 times normal | Predominant serum aminotransferase abnormality; hypergammaglobulinaemia of any degree |
| Autoantibodies | ANA, SMA or anti-LKM1 >1:80; no AMA | ANA, SMA or anti-LKM1 >1:40, or other autoantibodiesa |
| Histological findings | Interface hepatitis No biliary lesions, granulomas or prominent changes suggestive of another disease | Interface hepatitis No biliary lesions, granulomas or prominent changes suggestive of another disease |
aPerinuclear antineutrophil cytoplasmic antibodies, antibodies to soluble liver antigen/liver pancreas, actin, liver cytosol type 1 and asialoglycoprotein receptor.
ANA, antinuclear antibody; SMA, smooth muscle antibody; LKM, liver kidney microsomal antibody; AMA, antimitochondrial antibody.
Drug-Induced Hepatitis
Several unique factors predispose the elderly to drug-induced hepatotoxicity. These include polypharmacy and, subsequently, an increased risk of drug-induced adverse effects and drug–drug interactions. Age-related physiological changes, such as reduced liver mass, hepatic hypoperfusion and reduced activity of phase 1 hepatic drug-metabolizing enzymes, further increase the likelihood of hepatic injury in response to toxic drugs. Age-related changes in body composition may compromise the volume of distribution, thereby increasing serum drug levels. Hypoalbuminaemia resulting from excess cytokine elaboration, related to ageing or disease, may reduce protein binding and further increase the likelihood of drugs attaining toxic levels. Finally, altered pharmacodynamics with ageing affect the response to drugs at the tissue level (Regev and Schiff, 2001; Varanasi et al., 1999).
Not surprisingly, drug-induced liver disease occurs more frequently, and is more severe, in older adults. In addition, older patients with coexisting renal or hepatic disease are more likely to be affected. Documented prevalence of drug-induced hepatitis ranges from 50 to 140 per 1 million person-years in adults aged between 70 and 79 years (Almdal and Sorensen, 1990; Sgro et al., 2003). Overall, the incidence of drug-induced liver disease may be higher in older adults simply because these drugs are used more frequently. Non-steroidal anti-inflammatory drugs (NSAIDs) are used extensively by older adults for a variety of arthritic and non-arthritic conditions. All NSAIDs are potentially hepatotoxic. Nevertheless, the reported rate of NSAID-induced hepatotoxicity is less than 1%. Affected patients are usually asymptomatic, with elevated hepatic transaminases. Hepatic alkaline phosphatase may also be mildly elevated. Notably, patients with piroxicam-induced hepatitis may present with severe cholestatic features. NSAID hepatitis usually responds well to withdrawal of the offending agent. All older adults started on NSAIDs should have their liver function evaluated within two to three months of starting therapy (Hepps et al., 1991; Solomon et al., 2003).
Following a decline in the use of methyldopa, hepatic disease associated with the use of cardiac medications exhibited a decline. However, with the increased use of amiodarone, hepatocellular disease related to cardiac medications has begun to increase. Affected patients are usually asymptomatic. Approximately half of all patients on amiodarone exhibit a rise in serum transaminase levels. Amiodarone-induced hepatitis may occur with both oral and intravenous administration. These changes resolve if amiodarone is withdrawn early in the course of treatment. Other histological findings of amiodarone-induced hepatitis include steatohepatosis, cholestatic hepatitis and micronodular cirrhosis (Tameda et al., 1996; Traverse et al., 1994; Gonzalez Galilea et al., 2002)
With most medications, the increased prevalence of drug-induced hepatotoxicity in older adults is a consequence of increased exposure. However, certain drugs such as benoxaprofen, halothane and several antituberculous agents—isoniazid (INH), rifampicin and pyrazinamide—are inherently more likely to cause hepatotoxicity in older adults (Varanasi et al., 1999; Nagayama et al., 2003). Benoxaprofen is a non-steroidal agent, which was withdrawn by the United States Food and Drug Administration (FDA) following several reports of fatal liver failure occurring specifically in adults over the age of 70 years. Similarly, animal studies indicate an age-related increase in sensitivity to the effects of halothane, resulting in an increased risk of hepatic failure and death among older adults exposed to this agent.
INH hepatitis is rare in young patients but occurs in more than 2% of patients aged over 50 years. Increased sensitivity to INH in older adults is related to changes in hepatic physiology and altered pharmacokinetics. INH metabolism produces toxic reactive metabolites presumably from acetylation. Traditionally, persons with the rapid INH acetylator phenotype were considered more prone to toxicity. Most recent studies have failed to confirm this relationship. Indeed, convincing data suggest that slow acetylators may divert larger amounts of INH to an alternative metabolic pathway (cytochrome P450 2E1) that results in production of a toxic reactive metabolite (Huang et al., 2003). The precise mechanism underlying INH toxicity is still unknown.
Presenting features of INH toxicity range from asymptomatic elevation of transaminases to fulminant hepatic failure requiring liver transplantation (Vasudeva and Woods, 1997). Thus, patients on INH should receive serial serum transaminase measurements to facilitate early detection of hepatotoxicity.
Diagnosis and Management of Hepatitis
Clinical presentation of hepatitis varies widely and affected patients may be entirely asymptomatic. Some patients present with flu-like symptoms, such as fever, chills, skin rash, nausea, vomiting, myalgia, arthralgia or malaise. System-specific symptoms such as jaundice, abdominal discomfort, dark urine, easy bruising, and hepatomegaly may also occur. Certain hepatitides, such as hepatitis C, are characteristically asymptomatic during the acute phase. Diagnosis in such cases is usually delayed until several years after infection. In autoimmune hepatitis, despite the chronic nature of the disease, 40% of patients present acutely with fever, jaundice, polyarthralgias, myalgias, thrombocytopenia and biochemical evidence of severe hepatic dysfunction (Krawitt, 1996).
Serum testing in most cases of hepatitis will reveal elevated transaminases. In mild cases, elevation usually does not exceed three times normal, while in severe cases there may be a 20-fold increase. Clinical detectable jaundice is usually not present until serum bilirubin exceeds 3 mg dl−1. With severe disease, prothrombin time increases, and this is usually indicative of impending liver failure. Additional blood testing should be done in all cases to determine the a etiology of the hepatitis. Thus, viral antigen and antibody studies are conducted to screen for hepatitis A–E. GBV-C RNA may be identified using a reverse transcriptase polymerase chain reaction test. This test is not available for commercial use. There are also no serological assays routinely available for the diagnosis of GBV-C (HGV) or TTV (Stapleton, 2003).
An autoantibody profile for circulating autoantibodies should be conducted to screen for autoimmune hepatitis. Most patients will have elevated levels of circulating autoantibodies. However, only two-thirds will have one of the more specific autoantibodies. Patients are frequently screened for antinuclear and/or antismooth muscle antibodies (Lohse et al., 1995; Czaja and Freese, 2002). Tests for other autoantibodies such as soluble liver antigen, liver cytosol antigen and the asialoglycoprotein receptor antibody are also helpful diagnostic tools with high specificity (Manns et al., 1987; Martini et al., 1988; Treichel et al., 1994). Laboratory tests for autoimmune hepatitis should include serum protein electrophoresis. This may reveal hypergammaglobulinaemia with a selective increase in IgG levels. Human leukocyte antigen (HLA) typing may be helpful as most patients are positive for HLA B8, DR3 or DR4 (Donaldson et al., 1994).
The diagnosis of drug-induced hepatitis is usually one of exclusion based on the patient’s medication history, which should include questions pertaining to the use of prescription, over-the-counter and herbal medications.
Imaging techniques, such as ultrasound, computed tomography (CT) scans, and MRI are helpful in further evaluation of patients with suspected hepatitis for a etiology and severity of disease. Definitive diagnosis, assessment of severity, acuity and activity of disease are based on histological findings and require a liver biopsy.
On the basis of liver biopsy findings, hepatitis may be characterized as acute or chronic. Autoimmune hepatitis and all the viral hepatitides except HAV, HEV and HFV exist in both the acute and chronic phases. Histologically, chronic hepatitis may be further characterized into four stages: (i) chronic persistent to mild chronic active hepatitis; (ii and iii) chronic active hepatitis with scarring; and (iv) cirrhosis (Bach et al., 2000). Rapidity of clinical progression through these stages cannot be predicted.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree