Epidemiology and Pathogenesis
Thromboembolism (venous, cardiac, or arterial) is the commonest cause of death, and a major cause of morbidity, in later life. Like cardiac and arterial thromboembolism, the incidence of venous thromboembolism increases exponentially with age approaching 1% per year by 90 years (Figure 44.1).1 Almost half of cases occur between 60 and 79 years; and almost a quarter after 80 years (Figure 44.2).1 This may reflect age-related increases in risk factors and comorbidities (Table 44.1), and in activation of inflammation, endothelium, platelets and coagulation2, 3 combined with age-related decreases in coagulation inhibition,2, 4 fibrinolytic activity and in general mobility.
Figure 44.1 Incidence of first venous thromboembolism by age and sex. Rates are shown per 1000 per year, for men (striped bars), for women (solid bars). Reproduced from Rosendaal et al.1 with permission from Wiley-Blackwell.
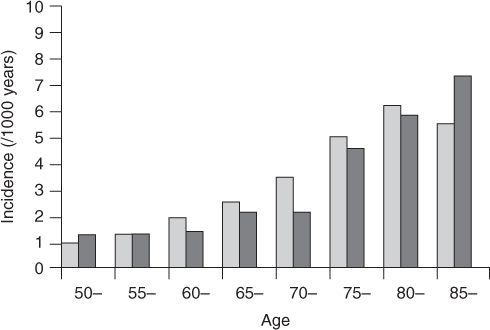
Figure 44.2 Age distribution of patients with venous thromboembolism. Percentage of patients by age group: 20–39 years, 7.5%; 40–59 years, 21.5%; 60–79 years, 45.9%; 80+ years, 23.6%. Reproduced from Rosendaal et al.1 with permission from Wiley-Blackwell.
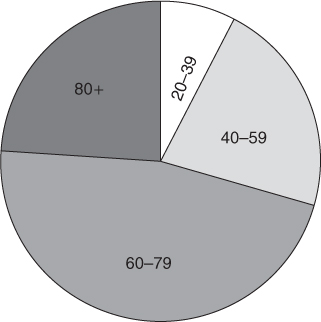
Table 44.1 Risk factors for venous thromboembolism.
| Patient factors | Disease or surgical procedure |
| Age | Trauma or surgery, especially of pelvis, hip, lower limb |
| Smoking | Malignancy, especially pelvic, abdominal, metastatic |
| Obesity | Heart failure |
| Blood lipids | Recent myocardial infarction |
| Immobility (bed rest over 4 days) | Paralysis of lower limb (e.g. stroke) |
| (Pregnancy) | Infection |
| (Puerperium) | Inflammatory bowel disease |
| Estrogen therapy | Nephrotic syndrome |
| Previous deep vein thrombosis or pulmonary embolism | Polycythemia |
| Genetic thrombophilias | Paraproteinemia Paroxysmal nocturnal haemoglobinuria Bechet’s disease |
Venous thromboembolism (VTE) may present as deep vein thrombosis of the leg (DVT) or pulmonary embolism (PE). Case-fatality is largely due to PE; and increases to over 10% in the elderly.1 Treatment of VTE is also more hazardous in the elderly: the risk of major haemorrhage during anticoagulation increases by nearly 50% for each decade of age.5, 6 Hence prophylaxis of VTE is especially important in the elderly. Because about half of cases occur within three months of hospitalization, routine prophylaxis against hospital-acquired thrombosis is important.
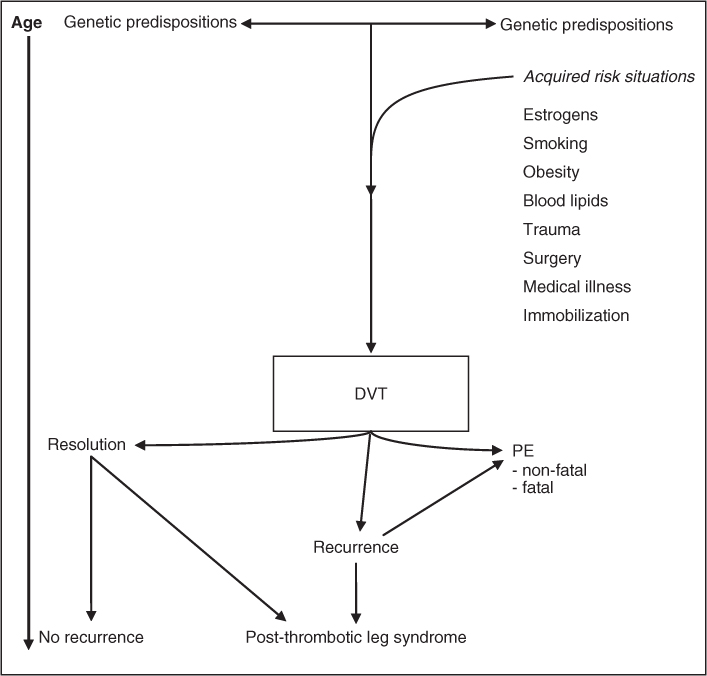
Risk factors for venous thromboembolism in older patients are similar to those in younger patients, with the obvious exception of pregnancy and the puerperium (Table 44.1). There is increasing evidence that the pathogenesis of DVT involves a ‘multiple hit model’, which starts at conception with multiple, interacting, genetic predispositions (thrombophilias) which thereafter interact throughout life with acquired risk factors which may precipitate thrombosis (Figure 44.3). Once venous thrombosis has occurred, it acts as a strong predictor of the risk of recurrence, especially if idiopathic.
Genetic Thrombophilias
Genetic thrombophilias should be suspected clinically if there is a past history, or a family history in blood relatives, of ‘premature’ (e.g. onset before 40–45 years) DVT, PE or recurrent fetal loss (spontaneous abortion or stillbirth); if there is recurrent venous thromboembolism or thrombophlebitis; or if thromboembolism occurs at an unusual site (upper limb veins, retina, cerebral venous sinuses, mesenteric, portal, or hepatic veins).8 Protein C or protein S deficiency may also present with coumarin-induced skin necrosis.8 Congenital deficiencies of the three coagulation inhibitors (antithrombin, protein C, or protein S) are usually due to heterozygosity for autosomal dominant gene defects; they increase the risk of VTE about two- to threefold.9 The low prevalence of these mutations in non-Western countries may explain their low incidence of DVT and PE.
DVT in the population is also associated with increased plasma levels of the von Willebrand factor—coagulation factor VIII complex;9 and probably explains why non-O blood group increases the risk of VTE by about 80% (non-O blood group elevates plasma levels of this complex by about 30%).10 Homozygous homocystinuria has long been recognized as a risk factor for premature arterial and venous thrombosis. More recently, hyperhomocysteinaemia has also been associated with increased risk of both venous and arterial thrombosis: this is partly due to heterozygosity for cystein synthase or methylene-tetrahydrofolate reductase (MTHRF) deficiency (whose cumulative prevalence in the general population is 0.4–1.5%) and partly due to deficiencies of vitamins (folate, cobalamine and pyridoxine) especially in the elderly.11There is much current interest in the possibility that dietary supplementation of these vitamins could have a major impact on venous as well as arterial thrombosis, particularly in the elderly; however, randomized trials have to date been inconclusive.12
Acquired Risk Factors
In recent years it has been increasingly appreciated that risk factors for arterial thrombosis (tobacco-smoking, obesity, diabetes and increased levels of blood lipids) are also risk factors for venous thromboembolism.9 As with genetic thrombophilias, increased activation of blood coagulation is the most likely explanation.9 Reduction in blood lipids by statin therapy appears to reduce the risk of VTE, as well as of arterial thrombosis.13 Aspirin prophylaxis in high-risk persons reduces the risk of VTE, as well as of arterial thrombosis, by about 24%.14
Varicose veins increase the risk of postoperative DVT,15 possibly because they may be a marker of previous (often asymptomatic) DVT in older persons. The increased risks of DVT and PE with increased estrogens, for example hormone replacement therapy,16, 17 suggest common mechanisms, including activated protein-C resistance, low levels of antithrombin and protein S, and high levels of factor IX.17 These risks are increased in women with thrombophilias.16, 17
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree