Sporadic Painless, Painful Subacute and Acute Infectious Thyroiditis
Alan P. Farwell
Introduction
Thyroiditis comprises a diverse group of disorders that are among the most common endocrine abnormalities encountered in clinical practice. Clinical presentations are diverse and include all manifestations of thyroid disorders, ranging from an incidental finding of a goiter to potentially life-threatening illness, from thyrotoxicosis to hypothyroidism, from an exquisitely painful thyroid to a painless goiter. A rational approach to such patients, including history, physical examination, laboratory evaluation, radionuclide or ultrasonographic imaging, and fine needle aspiration biopsy, will allow the appropriate diagnosis to be made in the vast majority of cases.
In general, the thyroiditis can be divided into categories based on etiology: 1) autoimmune, 2) infectious and 3) unknown (Table 22.1). The three types of thyroiditis discussed in this chapter represent each of these different etiologies (Table 22.2). Their clinical presentations can also be divided into two broad categories: 1) destruction-induced thyroiditis and 2) the painful thyroid. Sporadic painless thyroiditis follows the classical clinical course of the destruction-induced thyroiditis. Acute suppurative thyroiditis, especially the most common bacterial type, falls into the painful thyroid. Subacute painful thyroiditis includes features from both categories. A fourth category (infiltrative) can also be included, although the thyroid manifestations are a consequence of a systemic disorder affecting many other organs while the other etiologies are primary thyroid disorders. Because of this, difference, infiltrative thyroiditis will not be discussed further in this chapter.
Destruction-Induced Thyroiditis
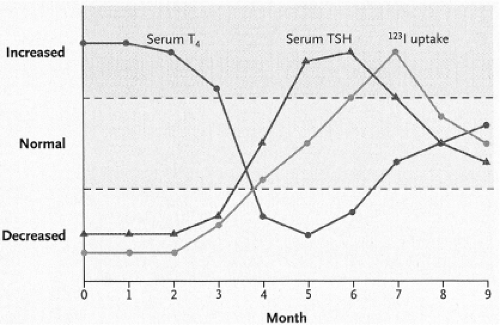
Sporadic painless and subacute painful thyroiditis, along with postpartum thyroiditis, are a group of disorders also known as the destruction-induced thyroiditis (1,2,3,4). These are transient disorders, usually consisting of four phases (Fig. 22.1). The clinical hallmarks of the destruction-induced thyroiditis begin with the abrupt onset of thyrotoxic symptoms, which is associated with a low thyroid radioactive iodine uptake (Table 22.3, see Chapters 12 and 17) and elevated serum thyroid hormone and thyroglobulin concentrations, consistent with the leakage of pre-formed hormone from a damaged gland. This represents the major cause of non-hyperthyroid thyrotoxicosis. Following a brief euthyroid phase as the thyroid hormones fall back into the normal range, hypothyroidism ensues, which is a consequence of depleted thyroid hormone stores and, possibly, recent TSH suppression during the thyrotoxic phase. Because the destructive process is self-limited, however, recovery generally occurs.
Table 22.1 Types of Thyroiditis | |
|---|---|
|
Table 22.2 Comparison Between the Syndromes of Thyroiditis | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Differential Diagnosis of the Painful Thyroid
Subacute thyroiditis is the most common cause of the painful thyroid and acute infectious thyroiditis is a potential life-threatening disease. Both of these disorders must be differentiated from the other causes of anterior neck pain in the acutely symptomatic patient (Table 22.4). Essentially all of the non-thyroidal causes of neck pain are infectious in origin and present as discrete painful masses (5). Acute hemorrhage into either a thyroid cyst or a nodule usually presents with the sudden onset of unilateral neck pain associated with a marked increase in the size of a preexisting nodule. The pain associated with a rapidly enlarging carcinoma, usually anaplastic, is often more chronic in nature (6), as is painful Hashimoto’s thyroiditis, which usually involves the entire gland and antibodies directed against thyroglobulin and thyroid peroxidase are usually present in high titer (7). Radiation thyroiditis occurs in the setting of radioactive iodine treatment for hyperthyroidism or following supravoltage external radiation of the anterior neck for thyroid cancer or lymphoma. Amiodarone, an iodine-rich antiarrhythmic drug, may cause iodine-induced thyrotoxicosis (Jod-Basedow disease) and, less commonly, thyroiditis, which may occasionally be painful (8,9). Globus hystericus, an anxiety reaction that is characterized by a constrictive feeling in the throat, is a diagnosis of exclusion.
Table 22.3 Causes of Low Radioactive Iodine Uptake Thyrotoxicosis | |
|---|---|
|
Sporadic Painless Thyroiditis
Sporadic painless thyroiditis has multiple other eponyms, including silent thyroiditis, painless thyroiditis, sporadic thyroiditis, destructive thyroiditis, spontaneously resolving lymphocytic thyroiditis, transient painless thyroiditis, painless thyroiditis with transient hyperthyroidism, painless subacute
thyroiditis, occult subacute thyroiditis, atypical thyroiditis, and transient thyrotoxicosis with lymphocytic thyroiditis (10). Sporadic painless thyroiditis and postpartum thyroiditis are probably variants of the same disorder, distinguished only by their relationship to a clearly defined inciting event, namely pregnancy. Their histopathologies are similar, as are their clinical courses and laboratory features. Postpartum thyroiditis is more clearly defined than sporadic painless thyroiditis, since it is easier to study the disorder in a prospective fashion and it is far more common than sporadic painless thyroiditis. Both of these disorders are autoimmune in nature and elevated circulating levels of antithyroid antibodies are frequently seen in sporadic painless thyroiditis. Postpartum thyroiditis is discussed in detail in Chapter 56.
thyroiditis, occult subacute thyroiditis, atypical thyroiditis, and transient thyrotoxicosis with lymphocytic thyroiditis (10). Sporadic painless thyroiditis and postpartum thyroiditis are probably variants of the same disorder, distinguished only by their relationship to a clearly defined inciting event, namely pregnancy. Their histopathologies are similar, as are their clinical courses and laboratory features. Postpartum thyroiditis is more clearly defined than sporadic painless thyroiditis, since it is easier to study the disorder in a prospective fashion and it is far more common than sporadic painless thyroiditis. Both of these disorders are autoimmune in nature and elevated circulating levels of antithyroid antibodies are frequently seen in sporadic painless thyroiditis. Postpartum thyroiditis is discussed in detail in Chapter 56.
Table 22.4 Differential Diagnosis of the Painful Neck Mass | |
|---|---|
|
Sporadic painless thyroiditis was not reported in the United States until 1969 and was uncommon up to 1973 (11). The frequency then increased and thyroiditis was thought to be responsible for about 20% of all cases of thyrotoxicosis in the United States (12). However, these likely represented cases subsequently reported in two epidemics of thyrotoxicosis thought to reflect sporadic painless thyroiditis but were found to be explained by meat contamination by the thyroid with the use of bovine strap muscles for the manufacture of hamburg (13,14). In a study from Japan, an incidence of 10% was found in the 1980s, but in New York it was only 2.4% (15). More recently, sporadic painless thyroiditis was not listed as a diagnosis in a study of hyperthyroidism in Demark, relegating the incidence to <1% (16). Affected patients are mostly between 30 and 60 years of age and the female to male ratio is about 1.5:1 (16,17).
Etiology
Thyroid autoimmunity in sporadic painless thyroiditis is probably inherited (18), which would be consistent with the observations that postpartum thyroiditis is weakly associated with genes that regulate immune function (19). These include, in certain populations, HLA-DR4, DR5, and DR3 in combination with -A1 and -B8 (19,20).
Clinical Manifestations
As a form of destruction-induced thyroiditis, sporadic painless thyroiditis is usually a transient disorder consisting of four phases, similar to postpartum thyroiditis (Fig. 22.1), although not all phases are seen in all patients (4,20,21). Clinical presentation varies from overt thyrotoxicosis, to thyroid enlargement with minimal thyroid dysfunction or hypothyroidism, depending on the stage in which the diagnosis is made. A non-tender goiter is usually present.
Phase 1/toxic phase: The initial phase is one of thyrotoxicosis, due to the “leak” of thyroid hormone from the regions of lymphocytic infiltration within the thyroid gland. Tachycardia, palpitations, heat intolerance, and emotional disturbances are characteristic of the thyrotoxic phase of sporadic painless thyroiditis. The ratio of serum T3 to serum T4 is lower in sporadic painless thyroiditis and postpartum thyroiditis than it is in Graves’ disease (22); therefore patients are less symptomatic and features that develop with longstanding thyrotoxicosis, such as substantial weight loss or severe muscle weakness, are unusual. The toxic phase usually last from 1 to 3 months.
Phase 2/euthyroid phase: A brief period of euthyroidism follows the thyrotoxic phase and may last for a few months (23).
Phase III/hypothyroid phase: As the gland becomes depleted of hormone, hypothyroidism ensues and may last for up to 1 year. Fatigue, malaise, impaired concentration, carelessness, and symptoms related to depression are common in patients in the hypothyroid phase. In general, the duration of hypothyroidism in those patients who initially present with thyrotoxicosis is more likely to be brief. Hypothyroidism tends to be more severe and prolonged if it is the presenting disorder. While most patients return to a euthyroid state, some remain permanently hypothyroid (4,20,21). However, recent studies suggest a far higher incidence of permanent hypothyroidism, with up to 54% of women with postpartum thyroiditis remaining hypothyroid (24,25). The features associated with the development of permanent hypothyroidism in sporadic painless thyroiditis are high titers of antithyroid antibodies, the lack of a detected thyrotoxic phase, more severe degrees of hypothyroidism and persistent hypoechogenicity on ultrasound. While recurrences of sporadic painless thyroiditis are not unusual, they are nowhere near the recurrence rate of women with postpartum thyroiditis after a subsequent pregnancy, probably due to a lack of a clearly recognized inciting event (4,20,21). The risk of permanent hypothyroidism in patients with a recurrent episode is increased. Further, these patients are susceptible to iodine-induced hypothyroidism years later as may be seen in other disorders of the thyroid (see Chapter 11E).
While the major clinical feature that distinguishes sporadic painless thyroiditis from subacute thyroiditis (see later) is the presence of thyroid pain and tenderness, thyroidal pain has occasionally been reported in sporadic painless thyroiditis. Fine needle aspiration biopsies consistent with chronic lymphocytic thyroiditis were described in five of eight patients presenting with destruction-induced thyrotoxicosis and thyroidal pain (26). These patients also had high titers of antithyroid antibodies and many of them developed permanent hypothyroidism. Conversely, painless destruction-induced thyrotoxicosis with
pathologic changes characteristic of subacute thyroiditis has been reported in 10 of 12 patients in the Netherlands (27).
pathologic changes characteristic of subacute thyroiditis has been reported in 10 of 12 patients in the Netherlands (27).
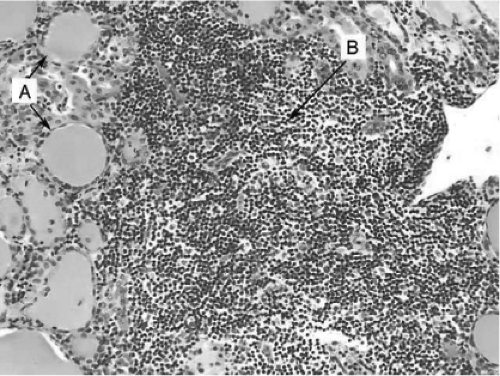 Figure 22.2 Histopathologic findings in painless thyroiditis. The specimen shows normal follicles with minimal hurtle cell metaplasia (A) and dense lymphocytic infiltration without germinal centers (B) (Hematoxylin and eosin, X 40). (Reproduced with permission from: Pearce EV, Farwell AP, Braverman LE. Thyroiditis. N Engl J Med 2003; 348:2646–2655.) See color plate. |
Laboratory Findings
During the toxic phase of sporadic painless thyroiditis, release of hormone from the inflamed thyroid results in increases in serum T4, T3, and a decrease in serum TSH. The thyrotoxicosis is associated with a low radioactive iodine uptake, which is a hallmark of the disease. Thyroglobulin levels will be increased and anti-thyroglobulin and anti-thyroid peroxidase antibodies may be present but usually in a low titer (23). TSH receptor antibodies are usually negative (28,29,30). The white blood cell count is generally normal. An increased erythrocyte sedimentation rate may be seen but is rarely greater than 40 mm/hour (23).
Ultrasonography generally shows decreased or heterogeneous echogenicity (31,32). The decrease in echogenicity has been correlated with the decrease in T3 levels following the toxic phase (32). During the toxic phase, color Doppler flow is markedly decreased, as opposed to the marked increase seen in Graves’ disease (31). However, care must be used to ensure that thyroid hormone levels are still increased, as increased color Doppler flow can be seen in the recovery euthyroid phase as well as the hypothyroid phase.
Pathology
Histopathology shows extensive lymphocytic infiltration, collapsed follicles, and degeneration of follicular cells (33) (Fig. 22.2). The changes can be either focal or diffuse with lymphoid follicles being present in about half of the patients (33). However, unlike Hashimoto’s thyroiditis, there is usually no stromal fibrosis, oxyphilic changes, or germinal centers. Most intra-thyroidal lymphocytes have the T-cell phenotype and distribution of T and B cells is similar in Hashimoto’s thyroiditis and sporadic painless thyroiditis (33). There is focal or diffuse chronic thyroiditis in the early stages of this disorder; during the recovery phase follicular disruption and hyperplastic changes of the follicles are common. The inflammatory changes noted above are seen as hypoechogenicity on ultrasound (31,32). The hypoechogenicity resolves with the resolution of the thyroiditis; persistence of hypoechogenicity is frequently observed in those individuals with permanent hypothyroidism.
Differential Diagnosis
Sporadic painless thyroiditis is one of several forms of thyrotoxicosis in which the radioactive iodine uptake is low (Table 22.3, see Chapters 12 and 17). This is also the case for thyrotoxicosis of extrathyroidal origin, such as struma ovarii and ingestion of supraphysiologic amounts of thyroid hormone. The most useful laboratory test in the diagnosis of thyrotoxicosis factitia is the serum thyroglobulin concentration. Serum thyroglobulin is low in patients who are ingesting extra thyroid hormone and is elevated in all other causes of thyrotoxicosis, including struma ovarii (34). Additionally, thyroid enlargement is common in destruction-induced thyrotoxicosis but unusual in thyrotoxicosis of extrathyroidal origin.
Sporadic painless thyroiditis in the toxic phase can be mistaken for Graves’ disease leading to the inappropriate use of antithyroid drugs, which are contraindicated in patients with sporadic painless thyroiditis. Radioisotope studies are recommended in thyrotoxic patients who do not have a goiter, if they have recently been pregnant, or if they have had an abrupt onset of thyrotoxicosis. Ultrasonography certainly is safe in nursing mothers and color Doppler ultrasonography reveals a markedly decreased blood flow as opposed to the increased blood flow in patients with Graves’ disease (31). As noted above, it is important to ensure that the thyroid hormone levels are still increased and serum TSH is decreased at the time either ultrasonography or radioactive iodine uptake is performed, since the radioactive iodine uptake may be normal or elevated and color Doppler flow increased as the patient recovers from the acute toxic phase. Measurement of the TSH receptor antibodies can be helpful in differentiating between these two conditions, as it is usually elevated in Graves’ disease and negative in sporadic painless thyroiditis (28,29,30).
In patients in whom the toxic phase either was missed or never occurred, the presentation of hypothyroidism is indistinguishable from other forms of hypothyroidism. Recently, determination of the erythrocyte zinc concentration has been proposed as an indicator of hypothyroidism due to sporadic painless thyroiditis as opposed to permanent hypothyroidism, with lower zinc levels seen in sporadic painless thyroiditis (35).
Clinical Management
Like the other causes of destruction-induced thyroiditis, the clinical course of sporadic painless thyroiditis is self-limited. The thyrotoxic phase of sporadic painless thyroiditis should be treated symptomatically with beta-adrenergic blocking drugs if signs and symptoms of thyrotoxicosis are moderate or severe. Antithyroid drugs have no role, as thyroid hormone biosynthesis is not increased. While sodium ipodate and iopanoic acid have been utilized to achieve rapid control of severe thyrotoxicosis in patients with thyroiditis in the past, neither of these two valuable medications are currently available in the United States.
Treatment of hypothyroidism may be necessary in either sporadic painless or postpartum thyroiditis if symptoms are pronounced or prolonged. However, if L-thyroxine therapy is instituted, it can be withdrawn after 6 to 9 months to determine whether recovery of thyroid function has occurred. In some patients it is reasonable to continue thyroid hormone indefinitely if a goiter persists or they have prognostic features that are associated with the development of permanent hypothyroidism, such as persistent goiter and extensive hypoechogenicity on ultrasound (36).
Subacute thyroiditis
Subacute thyroiditis is a spontaneous remitting inflammatory disorder of the thyroid that may last for weeks to months (1,3). This disorder has a number of eponyms, including de Quervain’s thyroiditis, giant cell thyroiditis, pseudogranulomatous thyroiditis, subacute painful thyroiditis, subacute granulomatous thyroiditis, acute simple thyroiditis, noninfectious thyroiditis, acute diffuse thyroiditis, migratory “creeping” thyroiditis, pseudotuberculous thyroiditis, and viral thyroiditis. The first description of subacute thyroiditis was in 1895 by Mygind, who reported 18 cases of “thyroiditis akuta simplex” (2). However, the pathology of subacute thyroiditis was first described in 1904 by Fritz de Quervain, whose name is associated with the disorder, when he reported giant cells and granulomatous-type changes in the thyroids of affected patients.
Subacute thyroiditis is the most common cause of the painful thyroid (Table 22.4) and may account for up to 5% of clinical thyroid abnormalities (1,2). An evaluation of the epidemiology of thyroid disorders in Denmark found an incidence of 2.5% for subacute thyroiditis (16), while the Mayo clinic reported an annual incidence of 4.9 cases per 100,000 population from 1970 to 1997 (37). As with other thyroid disorders, women are more frequently affected than men, with a peak incidence in the fourth and fifth decades. It is rarely seen during pregnancy (38) or in children (39,40). While the term “subacute thyroiditis” connotes a temporal quality that could apply to any thyroidal inflammatory process of intermediate duration and severity, it is actually referring specifically to the granulomatous appearance of the thyroid found on pathologic examination. This pathologic appearance of the thyroid is specific for the disease.
Etiology
There is no clear evidence for a specific etiology for subacute thyroiditis. Because it frequently follows an upper respiratory infection, a viral etiology is often proposed. Autoimmune and genetic etiologies have also been suggested over the years. The following discussion will address each of these potential causes.
Infectious Association
Indirect evidence suggests that subacute thyroiditis may be caused by a viral infection of the thyroid (41,42). The condition is often preceded by a prodromal phase of myalgias, malaise, low-grade fevers, fatigue, and frequently by an upper respiratory tract infection. It has been reported most frequently in the temperate zone, and only rarely from other parts of the world. It has been found to occur seasonally; the highest incidence is in the summer months (July through September), which coincide with the peak of enterovirus (Echovirus, Coxsackie virus A and B) infections (43). The incidence rate has been shown to vary directly with viral epidemics; during certain viral epidemics, specifically mumps, the incidence of subacute thyroiditis has been found to be higher. Interestingly, antibodies to the mumps virus have even been detected in individuals with subacute thyroiditis who do not have clinical evidence of mumps. Subacute thyroiditis has also been associated with other viral infections (2,44,45,46) including measles (47,48), influenza [both usual and H1N1 types (49)], the common cold, adenovirus, infectious mononucleosis, hand-foot-mouth disease (50), myocarditis (51), cat scratch fever, St Louis encephalitis (52), hepatitis (53), and the parvovirus B19 infection (54).
However, only mumps virus (55) and an unidentified cytopathic virus (45) have been directly isolated from affected thyroids while an electromagnetic imaging study demonstrated viral particles in thyroid tissue from a single patient with subacute thyroiditis (56).
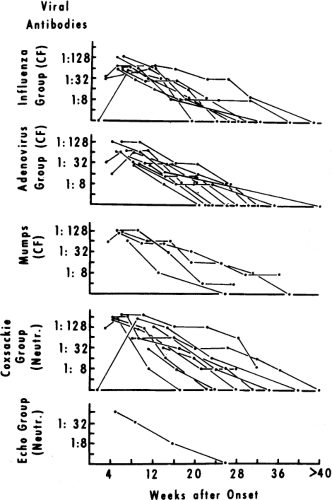
In the most commonly quoted study regarding a viral etiology of subacute thyroiditis, Volpe et al. (57) reported rising antibody titers to mumps virus, echovirus, adenovirus, and enterovirus in convalescent sera of 32 patients with subacute thyroiditis (Fig. 22.3). However, an additional 26 patients had demonstrable serologic viral antibody titers that did not change (57). Coxsackie virus is most commonly associated with subacute thyroiditis. A single report has described a fourfold rise in serum Coxsackie antibody titers after a documented case of subacute thyroiditis (58) and Coxsackie virus antibody titers have been shown to directly follow the course of the thyroid disease (43). However, in another study, sera, stool, and fine needle thyroid aspirations in 27 consecutive patients with subacute thyroiditis failed to document evidence of either Coxsackie or enteroviral infection (59). A similar report failed to find evidence of Epstein–Barr or cytomegalovirus infections in fine needle aspiration biopsy specimens of patients with subacute thyroiditis (60). Finally, 10 patients presented with post-viral thyroiditis that followed a similar course to subacute thyroiditis but was painless (61).
Certain non-viral infections including Q fever and malaria have been associated with a clinical syndrome similar to subacute thyroiditis. In addition, a case of subacute thyroiditis occurring simultaneously with giant cell arteritis has been reported (62).
Autoimmune Association
There is no clear association between subacute thyroiditis and autoimmune thyroid disease. Serum thyroid peroxidase and thyroglobulin antibody levels are usually normal. When described, the levels of thyroid peroxidase and thyroglobulin antibodies correlated with the phase of transient hypothyroidism. Antibodies to an unpurified thyroid preparation can be detected for up to 4 years after a bout of subacute thyroiditis.
Several reports have suggested that subacute thyroiditis may trigger the development of TSH receptor antibodies (63), contributing to a prolonged hypothyroid phase (64) and occasionally leading to the development of Graves’ disease
(65), although this was not observed in the most recent epidemiologic survey (37). In most studies, there was no correlation between the presence of thyrotropin-receptor–binding inhibitory immunoglobulin or of thyrotropin-receptor–stimulating immunoglobulin and the thyrotoxic phase of the thyroiditis (66). On the other hand, there has been some correlation between thyroid-blocking antibodies and the development of hypothyroidism. An explanation for this observation is that the appearance of the TSH-receptor antibodies results from an immune response that occurs after there is damage to the thyrocytes, specifically membrane desquamation (41,42). Following recovery from the inflammatory process of subacute thyroiditis, all immunologic phenomena disappear (66). Thus, the transitory immunologic markers that are observed during the course of subacute thyroiditis appear to occur in response to the release of antigenic material from the thyroid.
(65), although this was not observed in the most recent epidemiologic survey (37). In most studies, there was no correlation between the presence of thyrotropin-receptor–binding inhibitory immunoglobulin or of thyrotropin-receptor–stimulating immunoglobulin and the thyrotoxic phase of the thyroiditis (66). On the other hand, there has been some correlation between thyroid-blocking antibodies and the development of hypothyroidism. An explanation for this observation is that the appearance of the TSH-receptor antibodies results from an immune response that occurs after there is damage to the thyrocytes, specifically membrane desquamation (41,42). Following recovery from the inflammatory process of subacute thyroiditis, all immunologic phenomena disappear (66). Thus, the transitory immunologic markers that are observed during the course of subacute thyroiditis appear to occur in response to the release of antigenic material from the thyroid.
Manipulation of the immune system by vaccines and drugs has also led to the development of subacute thyroiditis. Reports have linked subacute thyroiditis with the hepatitis vaccine (67), influenza vaccine (68), the H1N1 vaccine (69), during interferon and interleukin-2 therapy (70,71,72,73) and combination interferon and ribavirin therapy (74,75). Other immune mechanisms have been suggested by an association between subacute thyroiditis and Sweets syndrome (76,77) and Takayasu’s arteritis (78). Subacute thyroiditis has also been reported in patients on long-term immunosuppression (79), suggesting a minimal effect of the immune system on development of the disease.
Table 22.5 Common Clinical Features of Subacute Thyroiditis. the following Clinical Features have been Reported in >50% of Patients with Subacute Thyroiditis (37,81,86,87)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|
|---|