Spine and Bone Pain
METASTATIC SPINAL DISEASE
Metastases of the spine may occur in the spinal cord (intramedullary), in the subarachnoid space (extramedullary), epidural space, and vertebral bodies. Intramedullary metastases are relatively rare (1% to 3% of cancer patients), and originate from the tumors outside the central nervous system (CNS; most commonly breast and lung cancers) as well as from CNS tumors such as glioblastoma, medulloblastoma, and ependymoma. Tumor spread occurs via blood or due to the cord penetration from leptomeningeal tumors. Intramedullary metastases may be single or multiple. Intramedullary metastases show low signal intensity on T1-weighted (T1W) magnetic resonance imaging (MRI) and high signal intensity on T2-weighted (T2W) images, with heterogeneous contrast enhancement. Leptomeningeal metastases have the same origin as the intramedullary ones, with the exception of acute leukemia, which occurs frequently in the dura. The intradural involvement (carcinomatous meningitis) results in thickened leptomeninges. As the tumor increases, nodules and/or plaques appear in the subarachnoid spaces. Myelography and intrathecal contrast-enhanced computed tomography (CT) reveal nodular filling defects suggesting leptomeningeal disease, which should be confirmed by positive findings on cerebrospinal fluid (CSF) study. Contrast-enhanced MRI will also identify the nodules and the dura involvement as area of contrast enhancement.
Leptomeningeal involvement is most commonly seen in melanoma, breast, and lung cancer. Tumor reaches the leptomeninges by hematogenous spread or by direct extension from preexisting parenchymal tumor deposits. Tumor cells are then disseminated throughout the neuraxis by CSF flow. Patients may present with signs and symptoms suggestive of local injury to nerves (cranial nerve palsies, radicular weakness, paresthesias, or pain); direct invasion into the brain or spinal tissues or interruption of blood supply to those tissues (focal findings or seizures); obstruction of normal CSF flow pathways (headache and increased intracranial pressure); interference of normal brain function (encephalopathy); or perivascular infiltration by tumor cells, leading to local ischemia and hence stroke-like symptoms. Without treatment, the median survival is 4 to 6 weeks, and death usually occurs as a result of progressive neurologic dysfunction. Often, leptomeningeal metastases are a manifestation of end-stage disease, and symptom management may be the most appropriate care.
Epidural and paraspinal lesions are closely related to those of vertebral bodies. On MRI, the tumor cells infiltrate and replace the fatty epidural spaces, with isohypointensity on T1W imaging, and high signal on T2W imaging, with homogeneous enhancement on postcontrast studies. Metastases of the vertebral bodies are the most frequent pathology of the spine. MRI is the method of choice in symptomatic patients for detecting and defining vertebral body metastases. Daldrup-Link et al.1 noted that positron-emission tomography (PET) scanning had a higher sensitivity (90%) for detection of bone metastases in young adults than whole-body MRI (82%) and skeletal scintigraphy (71%). Foraminal and intracanalar epidural extension of lesions is well defined on postcontrast MRI images. On T1W images the osteolytic metastasis by tumoral infiltration of the bone marrow shows hypointense signal related to isointense signal of the bone, whereas on T2W imaging, metastases show a high signal, easily depicted on Short T1 Inversion Recovery (STIR) and Spectral Presaturation by Inversion Recovery (SPIR) sequences.
The most frequent presentation of spinal tumors is axial pain. A thorough spinal examination includes assessment of local tenderness, deformity, limitation of motion, and signs of nerve root or cord compression. Management is guided by three key issues: neurologic compromise, spinal instability, and individual patient factors. Standard treatment options for spinal tumors include radiation therapy alone, radionuclide therapy, radiation plus systemic chemotherapy, hormonal therapy, or surgical decompression and/or stabilization followed by radiation.
The role of radiation therapy in the treatment of meta – static tumors of the spine is well established and is often the initial treatment modality.2 The goals of local radiation therapy in the treatment of spinal tumors are palliation of pain, prevention of pathologic fractures, and halting progression of or reversing neurologic compromise. A primary factor that limits radiation dose for local vertebral tumor control with conventional radiation therapy is the relatively low tolerance of the spinal cord to radiation. 3 Conventional external beam radiation lacks the accuracy to deliver large single-fraction doses of radiation to the spine near radiosensitive structures such as the spinal cord. Consequently, the low tolerance of the spinal cord to radiation often limits the treatment dose to a level that is far below the optimal therapeutic dose thus limiting the optimal clinical response.
Radiosurgery is defined as the delivery of a highly conformal, large single-fraction radiation dose by a stereotactic approach to a localized intracranial or extracranial tumor. The goal of radiosurgery is cessation of tumor growth and preservation of neurologic function. Precise confinement of the radiation dose should increase the likelihood of successful tumor control while minimizing the risk of spinal cord injury. Radiosurgery has been shown to be very effective for controlling intracranial malignancies.4 Stereotactic radiosurgery for tumors of
the spine has also been demonstrated to be accurate, safe, and efficacious.5
the spine has also been demonstrated to be accurate, safe, and efficacious.5
The emerging technique of spinal radiosurgery represents a logical extension of the current state-of-the-art radiation therapy. Technological developments include imaging technology for three-dimensional localization and pretreatment planning, the advent of intensity-modulated radiated therapy, and a higher degree of accuracy in achieving target dose conformation while sparing normal surrounding tissue. Unlike conventional radiation therapy that delivers a full dose to both the vertebral body and the spinal cord, the CyberKnife Image-Guided Radiosurgery System (Accuray, Sunnyvale, CA) can deliver a single high-dose fraction of radiation that conforms to the target tissue while sparing most of the adjacent spinal cord. Fiducials are placed using fluoroscopic guidance using a percutaneous technique. Fiducial placement procedure is performed in the operating room in an outpatient setting. A limit of 8 Gy is set as the maximum spinal cord dose for treatment planning calculations. A limit of 2 Gy is set as the maximum dose to each of the kidneys. A limit of 4 Gy is set as the maximum dose to the bowel. This especially becomes important in the treatment of lower thoracic and lumbar vertebrae, even more so if the patient has undergone a nephrectomy or received nephrotoxic chemo therapy. Potential lesions for spinal radiosurgery are listed in Table 23.1.
Gerszten et al.6 reported that spinal radiosurgery was highly effective in decreasing pain in patients with spinal tumors. Long-term pain improvement occurred in 96% of women with breast cancer, 96% of patients with melanoma, 94% of patients with renal cell carcinoma, and 92% of patients with neurofibromatosis Type 1. Pain usually decreased within weeks after treatment, and occasionally within days. Spinal radiosurgery was also effective at alleviating radicular pain caused by tumor compression of adjacent nerve roots.
MANAGEMENT OF EPIDURAL SPINAL CORD COMPRESSION
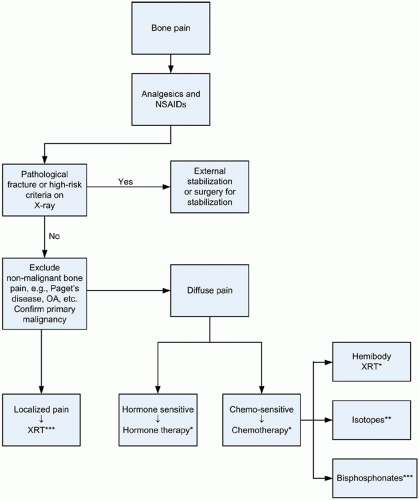
Epidural spinal cord compression (ESCC) is a neurologic emergency requiring immediate attention. ESCC usually occurs in patients with disseminated disease. The patterns of compression, as identified by magnetic resonance imaging (MRI) scan, appear to be predominantly soft tissue epidural disease.7 Figure 23.1 outlines a treatment algorithm of patients with symptomatic epidural spinal metastasis. Treatment of patients with coexisting pain and neurologic deficits should be prioritized according to neurologic deficit.
TABLE 23.1 POTENTIAL LESIONS FOR SPINAL RADIOSURGERY | ||||||||
|---|---|---|---|---|---|---|---|---|
|
The therapy instituted depends on several factors, including the patient’s condition at the time of presentation, the nature of the underlying malignancy, the extent of systemic disease burden, and patient prognosis.8 The goals of treatment are pain relief, preservation or recovery of neurologic function, and preservation of spinal stability. Prompt administration of corticosteroids is standard if symptomatic spinal cord compression is confirmed or strongly suspected on clinical grounds. However, there is no general agreement concerning the dosage and the schedule. Dexamethasone is the most commonly used corticosteroid, in doses of 10 to 100 mg I.V. bolus (according to clinical decision based on the course of neurologic deficit, prognosis, and clinical experience) followed by 16 to 96 mg daily orally. Commonly, the regimen is 96 mg I.V. bolus of dexamethasone followed by 96 mg per day orally for 3 days and a 10-day taper. The indications for chemotherapy in the treatment of spinal cord compression are very limited and in general should be considered as the sole therapy for adults with chemosensitive tumors (lymphoma, myeloma, breast, or germ cell tumors) who are not candidates for surgery or radiation.
The best treatment for ESCC is not well defined, and the choice between surgery with radiation or radiation alone is debatable. Management by radiation must balance the need to deliver a sufficient dose of radiation to kill the tumor and the need to avoid further injuring the spinal cord. Radiation volume is usually defined by myelography, computed tomography (CT), or MRI. The standard radiation volume should include the site of cord compression and should extend two vertebral bodies above and below.9 For patients with ESCC from solid tumors, 30 Gy in 10 fractions is considered the standard of care.10 Special techniques such as image-guided intensity modulated radiation therapy (IG-IMRT) or stereotactic body radiation therapy (SBRT) should be considered. However, the routine use of IG-IMRT or SBRT are currently not recommended, because the technology is expensive, and it has yet to show definite benefit over conventional delivery of radiation in a patient population that has a median survival of 6 months or less.10 The restrictions imposed by the radiation tolerance of the cord can limit the success of therapy. The ceiling of response, defined as maintaining pretherapeutic level of ambulation/motor function, is 80% with radiation therapy alone.5 This is particularly true with extensive tumor burdens, like spinal cord compression associated with a paravertebral mass, which require high doses of radiation to achieve local control. Lung cancers, specifically apical tumors, account for 60% of the presentations of epidural spinal cord compression associated with a paravertebral mass. Complete response to radiation therapy is achieved in 30% of all tumor types, including breast cancer and malignant melanoma.11 Radiosensitive tumors, like lymphoproliferative malignancies, multiple myeloma, and germ cell tumors, have a better outcome, with 77% of these tumors achieving a complete response to radiation alone.
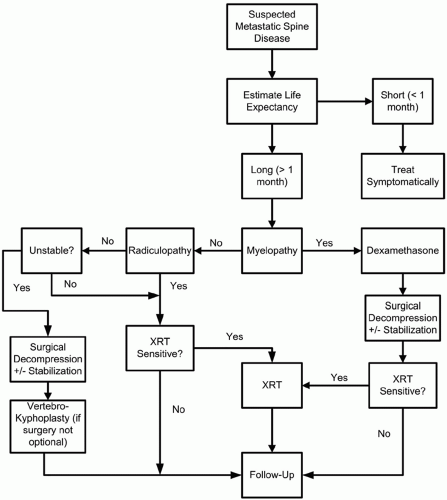 FIGURE 23.1 Treatment algorithm of patients with symptomatic epidural spinal metastasis. XRT, Radiation therapy. |
Combining surgery with radiation therapy may help improve therapeutic outcome. In some cases, surgical decompression by vertebrectomy or laminectomy can promptly reduce pain and improve neurologic status. These clinical improvements follow promptly relieving the mechanical compression produced by collapse of a vertebral body, and improving spinal stability. Surgical intervention is an alternative for patients presenting with a high-grade epidural lesion, particularly a lesion because of a radiation insensitive tumor. Surgery often is the only available option for therapy, because previously administered radiation may preclude further radiation in the area of compression. This is often the case in lung cancer because over 70% of spinal cord involvement in lung cancer is located in the thoracic spine, and many of these patients have received mediastinal radiation. Surgical intervention may provide significant benefit in specific groups with spinal cord or cauda equina compression. Patient selection should depend upon prognostic factors, so far as possible. For example, median survival in breast cancer patients with epidural metastases is significantly less if visceral metastases are evident.12 Even patients with advanced malignancies may benefit from surgical intervention if it is possible to maintain neurologic integrity.13 Decompressive laminectomy is suitable for posterior tumors in order to relieve spinal cord compression and to remove the lesion but is not considered helpful for the majority of compressions (which occur in the anterior epidural space) as laminectomy has been associated with a high rate of spinal instability14 and poor neurologic outcome.15 Anterior decompression (vertebral body resection) and stabilization is suitable in carefully selected patients (in good medical condition, with focal anterior ESCC and paraparesis), when performed in highly specialized centers. Many now advocate direct decompressive and maximal-debulking surgery with intraoperative stabilization of the spine (in appropriate cases) followed by postoperative radiation therapy.10
Measures of response involve pain and functional status. With radiation therapy alone, back pain resolves in 60% to 80% of patients.16, 17, 18, 19 Improvement in motor and autonomic dysfunction occurs in 40% to 60% of cases.16, 17 Pretreatment functional status is maintained at 3 years in follow-up after radiation therapy in over 90% of surviving patients.
FOCUSED MANAGEMENT STRATEGIES FOR PAINFUL BONE METASTASES
Metastasis to bone is a significant problem for a large number of cancer patients; up to 85% of patients dying from breast, prostate, or lung cancer primary tumors demonstrate bone involvement at autopsy.20 The morbidity of bone metastases can become significant due to pain and pathologic fracture. Pharmacologic management of pain associated with bone metastases is the mainstay of treatment and should follow the principles outlined in Chapter 16. Delaney et al.21 suggest an algorithmic approach to this problem based on well-designed randomized controlled trials, systematic reviews, or mega-analysis of published therapies (Fig. 23.2).
Not all patients with bone metastases exhibit symptoms, but as many as two thirds of patients with metastatic bone disease experience severe pain, particularly those who are in advanced stages of their diseases.22 Therapeutic strategies for painful bone metastases are listed in Table 23.2. The site of bone metastases significantly influences management strategies. In breast cancer patients, solitary bone metastases have different management implications than multiple skeletal metastases. Koizumi et al.23 showed in a multivariate analysis that a solitary metastatic bone lesion (P




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree