More recently, platinum combinations with topotecan and irinotecan have emerged as potential regimens for initial therapy. Irinotecan was shown to have single-agent efficacy in Japanese studies.
107 The Japan Clinical Oncology Group compared cisplatin and irinotecan to EP as initial treatment in extensive disease.
108 The study was terminated after 154 of the planned 230 patients were enrolled because median (12.8 months versus 9.4 months) and 2-year (19.5% versus 5.2%) survival were significantly better in the group treated with cisplatin and irinotecan. Significant diarrhea occurred only in the irinotecan group, and myelosuppression was the most common toxicity in both groups and more frequent with EP. Two confirmatory studies were subsequently launched in the United States. In the first trial, the irinotecan/cisplatin schedule was modified in an effort to decrease toxicity, leading to equivalent response rates (48% for irinotecan/cisplatin versus 44% for EP), median time to progression (4 versus 5 months), and median OS (9 versus 10 months).
425 The Southwest Oncology Group (SWOG) compared these two regimens with the same dose and schedule used in the Japanese trial and also showed, in a well-powered study, that outcomes are equivalent with the two regimens in Caucasian patients.
109 High response rates have been reported in several trials using irinotecan and carboplatin with varied dosing schedules.
110,111 A phase III trial comparing that regimen with etoposide/cisplatin showed improved survival, but the median survival of 7 months in the control arm, which used oral etoposide, was lower than expected.
112 Many hypothesize that population-based polymorphisms in uridine 5′-diphospho (UDP)-glucuronosyltransferase (UGT1A1), the enzyme responsible for detoxifying SN-38, the active metabolite of irinotecan, may account for differences in toxicity and efficacy between Japanese and Americans.
113 The regimen of topotecan plus cisplatin also has undergone phase II and III testing.
114,115 Eckardt et al.
115 reported the results of a randomized trial including 784 patients in which patients received oral topotecan (1.7 mg/m
2 per day for 5 days) plus cisplatin, or standard etoposide and cisplatin. The response rates, median survival, and 1-year survival were identical. Severe neutropenia occurred more often with EP, but oral topotecan and cisplatin caused more anemia and thrombocytopenia.
Strategies to Improve Outcomes with Chemotherapy Regimens
Alternating Cycles of Combination Chemotherapy Regimens. The recognition of clonal heterogeneity within a tumor and the intolerability of treatment regimens that included more than four drugs due to overlapping toxicity led to trials of alternating chemotherapy combinations. The somatic mutation model developed by Goldie et al.
116 predicted that the best probability of cure was achieved by the earliest possible introduction and the most rapid alternation of all active agents. If two equally effective non-cross-resistant
regimens were available, the model predicted that alternating between regimens every other cycle would be more effective than alternating after every three cycles or giving one regimen continuously for five cycles before switching to the second regimen.
Many randomized clinical trials have tested the concept of alternating multidrug combinations.
100,117,118,119,120,121 The fact that the EP regimen was effective in patients who had progressed after cyclophosphamide-based chemotherapy suggested that these drug combinations were non-cross-resistant.
122 With this in mind, the National Cancer Institute of Canada conducted a study in which 289 patients were randomized to CAV or CAV alternating with EP.
119 Chemotherapy was given for a total of six cycles. The response rate (65% versus 47%), PFS, and median survival time (10 months versus 8 months) favored the patients who had received alternating therapy. The authors postulated that these findings could be the result of the inclusion of a more active regimen (i.e., EP) within the alternating arm, an advantage due to greater drug diversity with five effective drugs rather than three, or support of the Goldie et al. concept. A Japanese study compared CAV to EP to alternating CAV/EP in 288 patients with limited or extensive stage disease.
99 Patients with limited disease received four cycles of chemotherapy followed by thoracic irradiation and were found to have improved survival with the alternating regimen compared with CAV (
p = 0.058) or EP (
p = 0.032). No differences in survival were noted in the patients with extensive disease. Roth et al.
100 evaluated 437 patients with extensive disease in a randomized trial comparing EP for four cycles, CAV for six cycles, or CAV alternating with EP for a total of six cycles. Although a slight improvement occurred in PFS (
p = 0.052) with the alternating regimen, there was no difference in response rate or OS among the treatment arms. The patients whose tumors did not respond to CAV and were crossed over to EP were twice as likely to benefit as individuals who initially received EP and were crossed over to CAV, although these differences were not significant (28% versus 14% for induction responders who relapsed and 15% versus 8% for patients with primary resistance). The modest activity seen when refractory patients were crossed over from one of these regimens to the other suggests that the CAV and EP combinations are not entirely cross-resistant, which works against a primary assumption of the Goldie et al. hypothesis. Taking all of these studies together, alternating regimens appears to have slight or no benefit over initial treatment with EP alone.
Additional studies have evaluated alternating chemotherapy introduced after achieving a response to an induction regimen.
123,124,125 The National Cancer Institute of Canada designed a randomized trial in which 300 patients with limited disease received either CAV for three cycles followed by EP for three cycles or CAV alternating with EP for a total of six cycles.
126 Response rates, time to treatment failure, or survival did not differ. Wolf et al.
123 randomized 321 patients to treatment with ifosfamide plus etoposide given until a response plateau, followed by CAV or ifosfamide plus etoposide alternating with CAV. A total of six cycles of chemotherapy were delivered in each arm. No difference in outcome was noted.
Studies also have evaluated alternating more intensive regimens. For example, a German multicenter trial demonstrated that an alternating eight-drug regimen was superior to CAV.
127 Two other European trials testing three drugs regimens alternating with four drug regimens found no survival advantage to that approach.
120,128 Again, the median survival times observed in these studies were no different from those that used EP alone.
99,100Addition of a Third Chemotherapeutic Agent to Etoposide Plus Cisplatin. All efforts to add a third drug to the standard EP regimen have resulted in more toxicity with little or no improvement in survival. The three-drug regimen of etoposide, ifosfamide, and cisplatin (VIP), developed initially for refractory germ cell tumors, also has been evaluated in SCLC.
129 In randomized trials comparing VIP to EP, one study, which included patients with limited and extensive disease, found no difference in survival between the two treatment groups,
130 whereas another, which was larger and enrolled only patients with extensive disease, identified a significant difference in median survival (9 months versus 7 months) and 2-year survival rates (13% versus 5%).
131 In both studies, myelosuppression was more severe in the ifosfamide-containing arm. Single-arm studies substituting carboplatin for cisplatin in ifosfamide, carboplatin, and etoposide (ICE) have shown impressive response rates, yet cumulative myelosuppression.
132,133 A large trial comparing ICE plus a midcycle dose of vincristine to other standard therapy demonstrated an improvement in the median and 1-year survival rates.
134 However, an increased rate of septicemia was noted with ifosfamide, carboplatin, and etoposide-vincristine (ICE-V) (15% versus 7% in the control arm).
Studies that added paclitaxel to EP reach the same conclusion: enhanced toxicity with similar efficacy. Two studies that compared EP to EP plus paclitaxel showed that the addition of the third drug increased toxicity, as well as treatment-related mortality, without improving survival.
135,136 A German study that added paclitaxel to etoposide and carboplatin demonstrated a significantly better median survival (13 months versus 12 months) and 3-year survival (17% versus 9%) only in patients with limited disease as compared to treatment with etoposide, carboplatin, and vincristine.
137Maintenance Therapy. A large number of randomized studies have examined whether maintenance chemotherapy prolongs survival in SCLC.
117,138,139,140,141,142,143,144,145,146,147,148 Three studies that randomized patients in complete remission after induction therapy to maintenance treatment or observation identified improved survival with the prolonged treatment program in some patient groups.
117,141,144 The Cancer and Leukemia Group B (CALGB) randomized 258 patients to one of four chemotherapy regimens, and 57 patients in complete remission underwent a second randomization to maintenance therapy or observation. Among the 46 patients with limited disease who proceeded to the second randomization, the median survival was improved with maintenance chemotherapy (17 months versus 7 months).
144 However, the initial regimens used in this study might be considered inferior to currently used treatments. In a second study, patients treated with six cycles of CAV and in complete remission were randomized to six additional cycles of the same chemotherapy or observation.
141 For the patients with extensive disease, the median survival was improved by approximately 4 months with maintenance treatment. In an ECOG trial, patients were randomized to CAV alternating with another three-drug combination or CAV alone and, subsequently, those in complete remission after six to eight cycles of induction underwent a second randomization to maintenance treatment or observation.
117 Patients assigned to CAV and maintenance therapy had a longer PFS and OS (
p = 0.09) than patients who received only CAV with no maintenance. In contrast, for the patients who received the six-drug regimen, those who were given no maintenance survived longer than the patients who received maintenance treatment. These studies suggest that there may be patients—perhaps those with particularly chemotherapysensitive disease—who derive a benefit from maintenance. In unselected patients, however, clinical trials that have evaluated treatment programs that extend beyond six cycles of chemotherapy have not demonstrated an advantage in survival.
The Medical Research Council randomized 265 patients who had responded to six cycles of induction chemotherapy to an additional six cycles of maintenance or observation.
138 Overall, there was no difference in survival between patients treated with 6 or 12 cycles of chemotherapy, although for patients in complete remission at the time of randomization, a subset analysis suggested that maintenance provides a survival benefit. Three other large studies that randomized patients responding to 5 or 6 cycles of induction to a total of 12 cycles of chemotherapy or observation found no difference in outcome.
142,143,146 Another study that randomized patients with limited disease from the start of chemotherapy to a total of 6 or 12 cycles identified inferior survival in the arm treated with the longer course of therapy.
140Other studies have evaluated whether four cycles of chemotherapy are adequate.
139,145,149 Spiro et al.
149 designed a study that included a double randomization at diagnosis. Patients received four or eight cycles of CEV and on relapse were given additional chemotherapy or supportive care. Of the four treatment arms, patients who received four cycles of chemotherapy and only supportive care at relapse had a significantly inferior median survival of 30 weeks. Four cycles of treatment were found to be adequate, provided that chemotherapy was offered to patients appropriate for additional therapy at relapse. Two additional studies evaluated four cycles of induction with longer treatment programs. A European trial randomized patients with limited and extensive disease who responded to four cycles of EP to CAV for up to 10 additional cycles or to observation with no survival differences, although the study had limited power due to small sample size.
139 ECOG enrolled 402 eligible patients with extensive-stage disease into a trial that delivered four cycles of EP followed by a randomization of patients with at least stable disease to four additional cycles of topotecan or to observation.
145 Although maintenance therapy increased the time before documentation of disease progression, there was no difference in OS.
Two recent meta-analyses have been conducted evaluating maintenance chemotherapy showing small improvements in survival and an increase in toxicity.
150,151 Bozcuk and colleagues
150 reported an improved 1- and 2-year survival by 9% and 4%, respectively. Although Rossi et al.
151 showed a significant OS benefit (hazard ratio [HR], 0.89, 95% confidence interval [CI], 0.81 to 0.92;
p = 0.02) for maintenance treatment, this improvement was projected to an additional 2 weeks.
151 Further, there was a high heterogeneity among the included trials.
In summary, four to six cycles of chemotherapy appear to be optimal in the management of limited and extensive SCLC. After the completion of this initial treatment, patients should be monitored closely and then offered further chemotherapy at the time of progression. Both the NCCN and the European Society of Medical Oncology Guidelines support this approach.
52,152Dose Intensification. In experimental models, numerous chemotherapy drugs display log-linear or near linear dose-response curves,
153 and high-dose chemotherapy has proven effective at treating hematologic diseases. It seemed reasonable to test the hypothesis that more intensive chemotherapy could improve outcomes in SCLC. Methods used have included the use of higher chemotherapy doses without or with hematopoietic growth factor support, shortened cycle length, or extreme dose intensification with marrow or peripheral blood stem cell support.
Several investigators evaluated whether increasing the dose of drugs beyond the usual dose improves survival.
154,155,156,157,158,159 Three randomized trials comparing standard versus high-dose CAV
156,158 or EP
157 found no difference in response rates or median survival. No hematopoietic growth factors were used in these three trials, and, as such, myelosuppression and infections were significantly more severe in the high-dose arms. A randomized trial that did utilize granulocyte-macrophage colony-stimulating factor (GM-CSF) with dose escalation found that excess toxicity actually resulted in lower drug delivery and poorer response and survival rates in the dose-intense arm.
159 Only a French study with 105 limited-stage patients demonstrated improvements in PFS at 2 years (28% versus 8%) and OS (43% versus 26%) with the administration of higher drug doses.
154 Few oncologists have embraced this approach.
A number of studies have evaluated whether shortening the interval between chemotherapy cycles improves survival. A multicenter study randomized 300 patients, mostly with limitedstage disease, to six cycles of ICE-V delivered every 4 weeks or every 3 weeks.
160 In a second randomization, patients were given GM-CSF or placebo after each chemotherapy cycle. The delivered dose intensity was increased by 26% in the group receiving chemotherapy every 3 weeks compared to those treated every 4 weeks. The median survival (443 days versus 351 days) and the 2-year survival rate (33% versus 18%) were better in the intensified arm (
p = 0.0014). GM-CSF did not reduce the incidence or the duration of febrile neutropenia, and there was no difference in survival between the patients who received GM-CSF or placebo. In a subsequent study, ICE given every 4 weeks was compared to ICE given every 2 weeks with support of GM-CSF, and autologous blood collected before the cycle was reinfused 24 hours after the chemotherapy.
161 Although the median delivered dose intensity was increased by 82% without significant increased toxicity, no survival benefit was identified. Two studies compared treatment with cyclophosphamide, doxorubicin, and etoposide given either every 3 weeks, or every 2 weeks with GM-CSF support.
162,163 The larger trial,
163 which also included a higher percentage of limitedstage patients, showed an improvement in complete response rate and OS, but the other trial did not. No fewer than four randomized trials have shown that intensive multidrug weekly regimens are no better, yet significantly more toxic than standard regimens.
164,165,166,167Numerous reports cite the use of high-dose chemotherapy with autologous bone marrow or stem cell rescue for treating SCLC.
168,169,170,171,172,173,174,175,176,177,178,179,180,181,182,183,184,185,186 These studies have included small numbers of highly selected patients.
161,182,183,187,188,189 Survival has not been shown to be better than conventional treatment. As in other chemosensitive solid tumors like breast cancer, high-dose chemotherapy with stem cell support does not appear to have a role in SCLC.
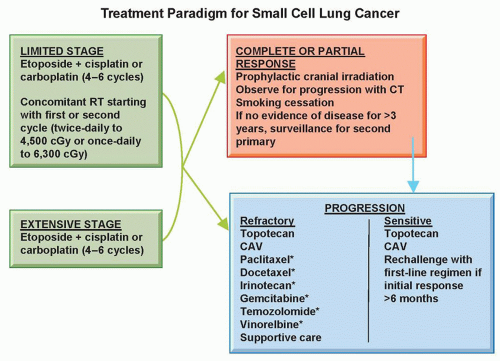
Treatment After Relapse Following Initial Therapy. The strongest predictor of outcome for patients with relapsed SCLC is the duration of remission. As such, patients are distinguished as having sensitive or refractory disease. The term sensitive implies an appropriate response to initial therapy that is maintained for 3 months or more. These patients have a higher likelihood of response to any additional chemotherapy; although, at best, it is approximately half that expected in the first-line setting. Survival from the start of a second regimen averages around 6 months. Patients with refractory disease either had no response to initial therapy or progressed within 3 months after completing treatment. Their chance of response to additional therapy is less than 10%, and their median survival from the start of a second regimen is 4 months.
The only approved agent in relapsed disease is topotecan. Ardizzoni et al.
190 reported a phase II trial in which topotecan, administered at a dose of 1.5 mg/m
2 daily for 5 days, yielded a response rate of 38% in sensitive patients and 6% in refractory patients. Median survival from the start of second-line therapy was 7 and 5 months, respectively. A randomized trial compared topotecan, administered at that same dose and schedule, to CAV in patients who relapsed at least 2 months after initial therapy.
191 The response rates for topotecan (24%) and for CAV (18%) were similar. The median survival was 6 months in both arms. Symptom improvement was better with topotecan for four of the eight symptoms queried, and as such, the U.S. Food and Drug Administration approved intravenous topotecan for sensitive relapsed SCLC. Oral topotecan has also undergone extensive testing in patients with relapsed SCLC. In a randomized phase II study, oral topotecan at a dose of 2.3 mg/m
2 daily for 5 days was comparable to intravenous topotecan 1.5 mg/m
2 daily for 5 days with regard to response rate (23% versus 15%), median survival (32 weeks versus 25 weeks), and symptom control.
192 Subsequently, the Medical Research Council showed that oral topotecan improved survival in relapsed sensitive and refractory SCLC over best supportive care alone (26 versus 14 weeks, respectively).
193 Oral topotecan led to a response rate of 7%, with a slower deterioration of quality of life and symptomatology. Another phase III study randomized 309 SCLC patients who had relapsed ≥90 days after first-line therapy to receive oral topotecan or intravenous topotecan.
194 The overall response rate and median survival time were 18.3% and 33 weeks, respectively, for patients who received oral topotecan compared to 21.9% and 35 weeks, respectively, for those who received intravenous topotecan. Although oral topotecan was associated with a lower
incidence of grade 4 neutropenia, diarrhea occurred more often in this group of patients. Oral topotecan also has received regulatory approval for second-line therapy of SCLC.
Amrubicin, a third-generation synthetic 9-amino-anthracycline with diverse molecular effects including DNA intercalation, inhibition of topoisomerase II, and stabilization of topoisomerase IIa cleavable complexes, has been studied extensively and has received approval in Japan for SCLC treatment.
195 A randomized phase II trial conducted there showed higher response rates and PFS compared with topotecan.
196 Two North American phase II trials of amrubicin showed encouraging results.
197,198 In patients with refractory SCLC, the overall response rate for single-agent amrubicin was found to be 21%, with median PFS and OS of 3.2 and 6 months, respectively. Subsequently, 76 patients with sensitive SCLC were randomized in a 2:1 fashion to receive amrubicin or topotecan. Amrubicin treatment resulted in a significantly higher response rate than topotecan (44% versus 15%,
p = 0.021), which led to improved PFS (4.5 versus 3.3 months) and OS (9.2 versus 7.6 months).
198 Despite phase II activity, preliminary results of the phase III study, which compared amrubicin to topotecan, were disappointing.
199 Although the activity of amrubicin was apparent, there was no statistically significant difference in OS observed between the two arms. The trend favored amrubicin (HR, 0.82; 95% CI, 0.68 to 0.99;
p = 0.036), especially in the subgroup of patients with primary refractory disease (HR, 0.77; 95% CI, 0.59 to 1.0;
p = 0.047). Although lower hematologic adverse events were noted in the amrubicin arm, these patients had a higher incidence of infections. The role of amrubicin for the treatment of patients with relapsed SCLC remains to be defined.
Temozolomide is an oral alkylating agent that crosses the blood-brain barrier. A phase II clinical trial of temozolomide in 64 patients with relapsed sensitive or refractory SCLC has been performed.
200 Temozolomide therapy was well tolerated and associated with an overall response rate of 20% in this patient population, with a 23% response rate in the sensitive group (n = 48) and a 13% response rate in the refractory cohort (n = 16). Responses also were noted in patients receiving temozolomide as third-line treatment and in those with brain metastases.
200 There is an ongoing multicenter phase II study comparing temozolomide and veliparib (a poly [ADP-ribose] polymerase [PARP] inhibitor) versus temozolomide and placebo in patients with relapsed sensitive and refractory SCLC (ClinicalTrials.gov identifier: NCT01638546).
Multiple trials have been conducted using other agents in this patient population. A list of single agents and their activity in relapsed SCLC is found in
Table 38.2, many of which also have been tested in combination studies. In summary, the optimal drug or combination of drugs in relapsed SCLC has not been established. Single-agent topotecan or CAV are appropriate for patients with sensitive relapse. These regimens also could be used for patients with refractory SCLC, although the response rates are lower. Agents evaluated in phase II trials with activity in SCLC can be considered. For patients with relapse 6 months or more after initial therapy, rechallenging with the same regimen as used in first-line treatment is also a consideration.
52