Paragangliomas (PGLs) arise from paraganglia in the parasympathetic and sympathetic chains, which track along large blood vessels. PGLs can be found from the skull base and inner ear to the scrotum. Most skull base and neck PGLs have a parasympathetic origin and are biochemically nonfunctioning. However, 3%–5% of skull base and neck PGLs are of sympathetic origin and can hypersecrete dopamine and/or norepinephrine. The considerations for the endocrinologist when seeing a patient with a skull base and/or neck PGL include addressing the following questions: (1) Is the PGL hypersecreting catecholamines; (2) does the patient have a germline pathogenic variant in a gene that predisposes to PGLs; (3) does the PGL have associated metastatic disease; and (4) are there additional PGLs elsewhere in the body?
Case Report
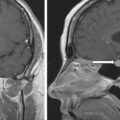
The patient was a 46-year-old woman seen in endocrine consultation for a large right neck glomus vagale PGL. She had noticed “a knot in my right neck” for about 10 years. It had been attributed by physicians to “swollen glands” over the years. Recently she developed symptoms of episodic heart racing. In addition, although usually normotensive, she had episodic elevated blood pressure (e.g., 188/110 mmHg). To investigate the neck mass, magnetic resonance imaging (MRI) was performed elsewhere and detected a large right glomus vagale PGL. On physical examination her body mass index was 26.8 kg/m 2 , blood pressure was 140/86 mmHg, and heart rate was 77 beats per minute. Palpation of the neck revealed a mass high in the neck that extended under the angle of the mandible.
INVESTIGATIONS
The plasma fractionated metanephrines and 24-hour urine for fractionated metanephrines and catecholamines were normal ( Table 44.1 ). Skull base and neck PGLs should always be screened for dopamine hypersecretion. A clinical pearl not well known to most endocrinologists is that because of the high sulfation rate of dopamine at the kidney, 24-hour urine for measurement of dopamine may be unreliable. Thus either plasma dopamine or methoxytyramine should be measured. Plasma catecholamines were obtained from in indwelling cannula after the patient was in the supine position and rested condition for 30 minutes. Despite the normal 24-hour urinary excretion of dopamine, the plasma dopamine concentration was more than 19-fold above the upper limit of the reference range (see Table 44.1 ).
| Biochemical Test | Result | Reference Range |
| Sodium, mmol/L | 139 | 135–145 |
Potassium, mmol/L | 4.2 | 3.6–5.2 |
Creatinine, mg/dL | 0.9 | 0.6–1.1 |
Plasma metanephrine, nmol/L | 1.1 | <0.5 |
Plasma normetanephrine, nmol/L | 14.0 | <0.9 |
Plasma norepinephrine, pg/mL | 388 | <750 |
Plasma epinephrine, pg/mL | <25 | <111 |
Plasma dopamine, pg/mL | 575 | <30 |
24-Hour urine: | ||
Metanephrine, mcg | 129 | <400 |
Normetanephrine, mcg | 263 | <900 |
Norepinephrine, mcg | 35 | <80 |
Epinephrine, mcg | 5.7 | <20 |
Dopamine, mcg | 333 | <400 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree