Skin Cancers and Sarcomas
Skin Cancers and Sarcomas
BASAL AND SQUAMOUS CELL CARCINOMAS
Parisa Momtaz
Allan C. Halpern
Epidemiology
Most common
CA in US; collectively known as nonmelanoma skin
CA
BCC is 5× more common than
SCC
Rarely
met, however, can be locally aggressive & disfiguring;
SCC w/greater potential for
met
Risk Factors/Pathogenesis
Sunlight: UVB strongly correlated
w/SCC; correlation
w/BCC is more complex
Fair-skinned individuals at greatest risk
Radiation exposure at a young age
Immunosuppression (organ transplantation)
For
SCC, other RFs include
HPV (types 16, 18, 31, 33, 38), chemical carcinogens
SCC arise from keratinocytes
Most
BCC arise from the epidermal cells differentiated in the primitive hair bulb
Genetics
Mts in
BCC frequently involve the
PATCH gene or members of the sonic
hedgehog signaling pathway → overexpression of transcription factor Gli 1
Specific UV-induced Mts in the tumor suppressor p53
gene
Genetic syndrome predispose to
BCC,
SCC: Albinism, xeroderma pigmentosum, Nevoid
BCC syndrome
Nevoid
BCC syndrome (aka basal cell nevus syndrome, Gorlin-Goltz syndrome)
Treatment Localized Disease: BCC, SCC
Treatment Metastatic Disease: BCC
Treatment Metastatic Disease: SCC
Prognosis and Follow-up
Localized disease has good prognosis
Worse prognosis for
SCC of the genitalia, mucous membranes
Perineural involvement increases the risk of recurrence for
BCC &
SCC & increases
met risk for
SCC
Close surveillance for high-risk pts (immunosuppression, organ transplantation)
Encourage sun protection strategies & self skin checks
Pts
w/h/o
BCC or
SCC are likely to develop more lesions; perform annual or bi-annual skin exams
MELANOMA
James J. Harding
Paul B. Chapman
Pathology
Histologic Subtypes
Cutaneous (most common)
Superficial spreading: Most common, radial growth
Nodular: Vertical growth into dermis, worse prognosis
Lentigo maligna: Sun-damaged skin in elderly or middle-aged pts,
usu on face
Acral lentiginous: Most common in Asians or African Americans,
usu on palms or soles
Desmoplastic/Neurotropic: Locally invasive, less likely to metastasize,
CN involvement
Uveal: Arise from melanocytes in iris, ciliary body or choroid
Mucosal: Arise from melanocytes in mucosal surfaces (ie, nasopharynx, anus, vagina)
Molecular Subtypes
The majority of melanomas are driven by overactivation of the
MAPK pathway
BRAF V600 (˜50-60%): V600E >V600K, commonly observed in younger pts w/nodular/superficial spreading melanoma of the trunk. Sensitive to vemurafenib or dabrafenib
NRAS (15-20%): No specific targeted
Rx available (MEK inhibition in clinical trials)
KIT: ↑ In mucosal, chronically sun-damaged skin, acral sites (˜20%); similar Mts as in
GIST
GNAQ/GNA11: Not observed in cutaneous melanomas, ↑ in uveal melanomas (>80%), activates heterotrimeric G-protein coupled receptors → activates
MAPK pathway
Other Mts: PIK3CA/AKT, PTEN loss, NF-1, & BAP1
Clinical Manifestations
Sx: Cutaneous: Most melanomas found by pt at early stage;
adv disease → enlarged
LN, skin nodules,
sx related to lung, liver, bowel/mesenteric, or brain
mets;
uveal: Incidental finding or visual complaints;
mucosal: Mucosal bleeding
PEx: Evaluate skin & mucosal surfaces;
ABCDEs: Asymmetry,
Borders irregular,
Color variegated,
Diameter >5 mm.
Evolution; check for
LAN or subcutaneous
met, sequela of widespread
met disease,
melanosis → rare, blackening of the skin & urine due to ↑ melanin production, poor prognosis
Labs: Microcytic anemia, suspect chronic blood loss from bowel
mets; ↑
LDH
Diagnostic Evaluations and Staging
Punch
bx preferred over shave
bx; shave
bx can transect the tumor & prevent proper depth assessment (T-staging)
EOD w/CT-CAP or
CT-Chest w/PET (especially if
1° lesions is in the distal extremity), if distant disease,
FNA or Core
bx
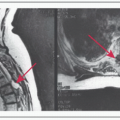
Baseline MRI-brain w/gadolinium for Stage III disease or higher to
r/o intracranial
met.
Evaluation/staging/
tx of uveal melanoma is different
Treatment of Localized Cutaneous Melanoma (Stages I-III)
Wide local excision of 1°: Margin of 1 cm if tumor ≤1 mm deep, margin of 2 cm for all other lesions
Sentinel LN mapping & bx: Lymphoscintigraphy w/Tc99 colloid,
usu used for lesions >1 mm, if <1 mm consider if high-risk features
Completion LND: Performed if sentinel
LN positive, whether this procedure improves
OS is subject of ongoing phase III study
Adjuvant Rx & surveillance: IFN-α ↑
RFS; radiotherapy ↑ local regional control, no
RFS/
OS advantage; clinical trial participation; or observation (serial exam/imaging in IIB-IV
NED)
Metastatic Cutaneous Melanoma
Metastatectomy: In properly selected pts, long-term
OS 20-40%
Immunotherapy:
Ipilimumab (CTLA-4 blocking Ab): ↑
OS in 2
RCT (
NEJM 2010;363:711 &
NEJM 2011;364:2517), slow acting, monitor for immune-mediated
tox (ie, colitis, dermatitis, hepatitis, etc.)
Programmed D-1 receptor: RR ˜30% (
NEJM 2012;366:2443)
IL-2: Given in
ICU setting, 2-6% pts w/durable disease control/cure
Adoptive cellular Rx/TILs: Experimental, high
RR
Chemotherapy: Dacarbazine (
DTIC)/Temozolomide,
RR 7-19%; Combination chemotherapy: Cisplatin, vinblastine, temozolomide (
CVT)
RR 30-40%, Carboplatin/Taxol
RR 20-30%, no
OS advantage; Biochemotherapy = chemo + IL-2 + IFN-α, has ↑
RR, no
OS advantage over chemo
GASTROINTESTINAL STROMAL TUMOR
James J. Harding
William D. Tap
Get Clinical Tree app for offline access