Most patients with corticotropin (ACTH)-dependent Cushing syndrome (CS) will have an ACTH-secreting pituitary microadenoma—50% of which are so small that they cannot be seen on magnetic resonance imaging (MRI). Pituitary-dependent CS is typically associated with mild-to-moderate CS, and 24-hour urinary free cortisol (UFC) excretion is typically 100–500 mcg and very rarely >1000 mcg. When patients with ACTH-dependent CS present with spontaneous hypokalemia and 24-hour UFC >1000 mcg, the clinician should suspect an ectopic ACTH-secreting tumor. However, there is a subset of patients with pituitary-dependent CS who have large pituitary adenomas and the clinical presentation can overlap with that of ectopic ACTH secretion. Herein we present such a case.
Case Report
The patient was a 28-year-old woman who was self-referred for possible CS. She experienced a 62-pound centrally distributed weight gain over 3 years. She had noticed a rounding and redness of her face, hirsutism on her cheeks and upper lip, and acne on her arms. She had marked weakness in her legs when going up stairs. Recently, she was diagnosed with mild hyperglycemia and placed on metformin. Elevated blood pressure readings were noted on her last few blood pressure checks. She had also developed secondary amenorrhea. As a registered nurse, she raised the possibility of CS to explain her signs and symptoms. Her medications included metformin 500 mg twice daily and ranitidine 150 mg daily. Amlodipine and metoprolol were added to treat her hypertension. On physical examination her body mass index was 38.9 kg/m 2 , blood pressure was 138/98 mmHg, and heart rate 76 beats per minute. She appeared markedly cushingoid compared to photographs taken 3 years previously ( Fig. 57.1 ). She had a full round and plethoric face. She had marked supraclavicular and dorsocervical fat pads. Her lower extremities were thinner than the rest of her body. There were thin red striae on her flanks.

INVESTIGATIONS
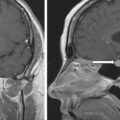
The laboratory test results are shown in Table 57.1 . She had spontaneous hypokalemia. The cortisol concentrations in the blood and urine were diagnostic of severe hypercortisolism. The serum concentration of ACTH was markedly elevated. Computed tomography of the chest and abdomen did not reveal a neoplasm in the lung, pancreas, or small bowel. However, head MRI did identify an 8-mm right-sided pituitary tumor ( Fig. 57.2 ). The patient was informed that her marked CS was most likely because of a relatively large corticotroph pituitary tumor. We advised that IPSS does carry some risk and was not needed in her case. Brain stem injury has been reported to occur in 1 out of 508 (0.2%) patients undergoing IPSS at the National Institutes of Health. In our early Mayo Clinic series of IPSS (1990–97) in 92 patients we had 2 (2%) serious complications (venous subarachnoid hemorrhage, lower extremity deep venous thrombosis). In a series of 86 patients who had IPSS in Grenoble, France, 2 (2%) patients had transient sixth nerve palsies.
| Biochemical Test | Result | Repeat Test Result | Reference Range |
| Sodium, mEq/L Potassium, mEq/L Fasting plasma glucose, mg/dL Glycosylated hemoglobin, % Creatinine, mg/dL eGFR, mL/min per BSA 8 am serum cortisol, mcg/dL 4 pm serum cortisol, mcg/dL 24-Hour UFC, mcg 24-Hour urine volume, L ACTH, pg/mL DHEA-S, mcg/dL Prolactin, ng/mL | 146 3.5 102 5.4 0.8 >60 33 33 1057 2.1 192 181 17.3 | 42 | 135–145 3.6–5.2 70–100 4–6 0.6–1.04 >60 7–25 2–14 3.5–45 Goal <4 L 10–60 44–332 4.8–23.3 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree