Sentinel lymph node (SLN) surgery has largely replaced axillary dissection for nodal staging in clinically node negative breast cancer patients. However, in patients with previous breast and/or axillary surgery, pregnant patients, male patients, multifocal/multicentric breast tumors, DCIS, and patients receiving neoadjuvant chemotherapy, the use of SLN surgery is more controversial. Lymphoscintigraphy is important in patients with prior surgery to evaluate for drainage to extra-axillary sites.
Surgical staging of the axillary lymph nodes in patients with breast cancer has evolved from axillary lymph node dissection (ALND) to sentinel lymph node (SLN) surgery. Although SLN surgery has become the standard of care for clinically node-negative early-stage breast cancer, controversies exist regarding its applications in some special circumstances. American Society of Clinical Oncology (ASCO) published guideline recommendations for use of SLN surgery in 2005 with a section devoted to SLN in special circumstances. The literature was more limited at that time, and additional data have since been published in these areas. In this article, an update of the information on the role of SLN surgery in uncommon circumstances is provided.
Breast cancer in men
In general, men with breast cancer have larger tumors than women have and are more likely than women to have positive nodes. At the time of issuance of the ASCO panel recommendations, data on the use of SLN surgery in men with early-stage breast cancer were limited. Therefore, no categorical recommendations about the use of SLN surgery for men with breast cancer were made, despite it being unlikely that SLN surgery would be any less accurate in men than it was in women.
There have been several additional studies with larger numbers of patients showing technical feasibility and accuracy of SLN surgery in men similar to that in women. Boughey and colleagues compared 30 men and 2784 women with breast cancer who underwent SLN surgery. The SLN was identified in 100% of men and in 98.3% of women. The incidence of positive SLNs was higher in men than women (37.0% vs 22.3%), although this did not reach statistical significance. In cases with positive SLNs, male patients had increased risk of additional disease in nonsentinel axillary lymph nodes compared with women (62.5% vs 20.7%). Additional data and review of literature by Rusby and colleagues reported combined data from 110 men who had undergone SLN surgery and showed a 96% SLN identification rate. There were no false negatives in the 13 patients with negative SLNs who had undergone concomitant ALND. Gentilini and colleagues reported an identification rate of 100% in 32 men with early breast cancer who underwent SLN surgery. No backup axillary dissection was performed in 26 patients with negative SLNs; however, after a median follow-up of 30 months no axillary recurrence occurred. SLN surgery in 78 men at Memorial Sloan-Kettering Cancer Center reported an SLN identification rate of 97%. Negative SLNs were found in 39 of 76 (51%) patients. In 3 (8%) patients with negative SLNs, a positive non-SLN was identified by intraoperative palpation. At a median follow-up of 28 months, there were no axillary recurrences.
As a result of data comparable to breast cancer in women, although not formally validated, SLN surgery is now advocated as the procedure of choice in men with clinically node-negative breast cancer. Given the higher rate of SLN positivity in men and higher rate of non-SLN involvement in patients with a positive SLN, intraoperative evaluation of the SLN should be considered in the surgical management of male patients with breast cancer and completion ALND recommended in cases with positive SLN.
Pregnant patients with breast cancer
Significant fetal radiation exposure may result in malformations, mental retardation, and childhood cancer. The ASCO 2005 guidelines on use of SLN surgery, while acknowledging that the dose of radiation to the fetus was minimal, nevertheless concluded that there were insufficient data to recommend the use of SLN surgery in pregnant women. Understandably, the radiation effects are most harmful during early fetal life at the time of organogenesis. The use of phantom models, based on radiation-absorbed dose calculations in nonpregnant women who have undergone SLN surgery, estimated the fetal absorbed dose to be 0.014 mGy or less, using 0.5 mCi activity (18.5 MBq). In another study, Keleher and colleagues estimated the maximum absorbed dose to the fetus in 2 nonpregnant women using 92.5 MBq tracer activity to be 4.3 mGy. These absorbed doses are well below the acceptable radiation dose to the pregnant woman.
More recent guidelines, however, including those on breast and head and neck cancers and melanoma, do not consider pregnancy a contraindication for SLN surgery, especially beyond the first trimester. Despite theoretical safety, surgeons are reluctant, and currently studies of the use of SLN surgery in pregnancy are limited to a few case reports and series with few patients. At the European Institute of Oncology in Milan, SLN surgery is offered to women with breast cancer diagnosed during pregnancy, and Gentilini and colleagues recently reported on 12 pregnant patients who underwent SLN surgery. The SLN was identified in all patients. Of the 12 patients, 10 had pathologically negative SLNs. One patient had micrometastasis in 1 of 4 SLNs. One patient had metastasis in the SLN and underwent axillary clearance. No detrimental effect on the fetus was observed. There was no overt axillary recurrence in the patients with negative SLNs after a median follow-up of 32 months. Similar results have been reported from the Moffitt Cancer Center where 10 patients with an average gestation of 15.8 weeks underwent SLN surgery. In all cases the SLN was identified and the sentinel node was positive in 50%. Nine patients delivered healthy children and 1 patient elected to terminate her pregnancy. Due to lack of data on the safety of blue dye in pregnancy, most surgeons performing SLN surgery in pregnant women use radioactive tracer only.
SLN surgery in pregnant women must be considered on an individual basis, with thorough counseling regarding level of the risk of fetal damage and benefits. When SLN surgery is used, efforts should be made to reduce fetal radiation exposure including the use of same-day surgery following injection of the radiolabeled colloid, which allows reduction of injected activity down to 10 to 15 MBq and reduction of exposure time.
Pregnant patients with breast cancer
Significant fetal radiation exposure may result in malformations, mental retardation, and childhood cancer. The ASCO 2005 guidelines on use of SLN surgery, while acknowledging that the dose of radiation to the fetus was minimal, nevertheless concluded that there were insufficient data to recommend the use of SLN surgery in pregnant women. Understandably, the radiation effects are most harmful during early fetal life at the time of organogenesis. The use of phantom models, based on radiation-absorbed dose calculations in nonpregnant women who have undergone SLN surgery, estimated the fetal absorbed dose to be 0.014 mGy or less, using 0.5 mCi activity (18.5 MBq). In another study, Keleher and colleagues estimated the maximum absorbed dose to the fetus in 2 nonpregnant women using 92.5 MBq tracer activity to be 4.3 mGy. These absorbed doses are well below the acceptable radiation dose to the pregnant woman.
More recent guidelines, however, including those on breast and head and neck cancers and melanoma, do not consider pregnancy a contraindication for SLN surgery, especially beyond the first trimester. Despite theoretical safety, surgeons are reluctant, and currently studies of the use of SLN surgery in pregnancy are limited to a few case reports and series with few patients. At the European Institute of Oncology in Milan, SLN surgery is offered to women with breast cancer diagnosed during pregnancy, and Gentilini and colleagues recently reported on 12 pregnant patients who underwent SLN surgery. The SLN was identified in all patients. Of the 12 patients, 10 had pathologically negative SLNs. One patient had micrometastasis in 1 of 4 SLNs. One patient had metastasis in the SLN and underwent axillary clearance. No detrimental effect on the fetus was observed. There was no overt axillary recurrence in the patients with negative SLNs after a median follow-up of 32 months. Similar results have been reported from the Moffitt Cancer Center where 10 patients with an average gestation of 15.8 weeks underwent SLN surgery. In all cases the SLN was identified and the sentinel node was positive in 50%. Nine patients delivered healthy children and 1 patient elected to terminate her pregnancy. Due to lack of data on the safety of blue dye in pregnancy, most surgeons performing SLN surgery in pregnant women use radioactive tracer only.
SLN surgery in pregnant women must be considered on an individual basis, with thorough counseling regarding level of the risk of fetal damage and benefits. When SLN surgery is used, efforts should be made to reduce fetal radiation exposure including the use of same-day surgery following injection of the radiolabeled colloid, which allows reduction of injected activity down to 10 to 15 MBq and reduction of exposure time.
Ductal carcinoma in situ
The management of the axilla for ductal carcinoma in situ (DCIS) has changed dramatically over the years. In the past, DCIS accounted for a small proportion of all breast cancer cases and was diagnosed after presentation with a palpable mass, nipple discharge, or Paget disease. DCIS now accounts for approximately 20% of all new breast cancers diagnosed in the United States, more than 90% of which are asymptomatic and detected on screening studies, most commonly by the presence of microcalcifications on mammography. By definition DCIS is preinvasive, and should not have the potential to invade beyond the basement membrane and spread to the regional lymph nodes.
However, the need for SLN surgery in patients with a preoperative diagnosis of DCIS is debated. Some 10% to 30% of patients with a preoperative percutaneous biopsy diagnosis of DCIS will be found to have invasive disease in their final surgical pathology specimen. Such a finding results from sampling error as well as limitations of sampling techniques that may miss a small cancer within a large area of DCIS. These patients are thus upstaged to invasive cancer at final pathology and therefore need nodal evaluation.
Some investigators argue that performing SLN surgery in patients with a preoperative biopsy diagnosis of pure DCIS allows those found subsequently to have invasive disease to avoid further surgery. There are several observational studies that report results of SLN surgery in patients with DCIS. In a meta-analysis of observational studies, Ansari and colleagues reported that the frequency of a positive SLN in patients with a preoperative diagnosis of DCIS ranged from 0% to 16.7%, with an overall incidence of SLN positivity of 7.4%. This result contrasted with an overall SLN positivity rate of 3.7% in patients with a definitive (postoperative) diagnosis of DCIS.
Therefore, it is desirable to predict the subset of patients with a biopsy diagnosis of DCIS who are at higher risk of harboring invasive disease. For these patients, performing SLN surgery at the time of their tumor surgery would be advantageous. In most studies a palpable mass, a mammographic mass, a large-size lesion, and a high-grade lesion were associated with a significant risk of invasive disease in the final resection specimen.
Current recommendations for SLN surgery in patients with biopsy revealing DCIS include those patients who are at high risk of occult invasive disease, in an attempt to prevent a second operation. This group may include patients with a palpable tumor, an extensive area of DCIS, high-grade DCIS, or microinvasion on preoperative biopsy. In addition, patients with DCIS who are undergoing mastectomy or breast reduction or reconstruction should also be considered for SLN surgery because should they be found to have invasive disease, SLN surgery is not usually possible after such procedures. When immediate autologous tissue reconstruction is being performed in patients with DCIS (or invasive cancer), it may be appropriate to carry out SLN surgery as an initial separate procedure to avoid tissue reconstruction in node-positive patients in whom postmastectomy radiation may be recommended.
Multicentric/multifocal breast cancer
Patients with multicentric and/or multifocal breast cancer were initially considered not to be candidates for SLN surgery because of concerns of higher false-negative rates and technical feasibility. The dominant view regarding the flow of the lymph in the breast considers the entire breast tissue as a single lymphatic unit that drains to specific primary SLNs. In other words, no matter where the sites of the tumors within the breast or what the methods of the injections are, the primary lymphatic drainage seems to be the same, although some controversy continues. The implication of this concept has prompted the use of SLN surgery in multicentric/multifocal disease.
To date, numerous small and larger series have reported on the feasibility and accuracy of performing SLN surgery in multifocal/multicentric breast cancer. Identification rates and false-negative rates, from most series, have ranged from 90% to 100% and 0% to 15%, respectively. Various injection methods have been used, in particular subareolar or intradermal, with or without preoperative lymphoscintigraphy, with acceptable identification and false-negative rates. Earlier smaller studies reported higher false-negative rates. One study of 21 patients using intratumoral blue dye only reported a 33% false-negative rate with a 85.7% identification rate, and another study reported 21% (8 of 38 patients) false-negative rate in patients with multicentric/multifocal disease. In one of the largest prospective series, out of 3730 patients in the Austrian Sentinel Node Study Group, a multi-institutional validation study of SLN surgery, 125 patients with multicentric cancer underwent ALND after SLN surgery with a false-negative rate of only 4%.
Based on current evidence, SLN surgery may be considered in clinically node-negative patients with multicentric/multifocal disease. However, given the possibility of higher false-negative rates observed in some reports, especially in patients with large tumor burdens, careful intraoperative palpation of the remaining axillary nodes, including excision of any suspicious nodes, should be performed to reduce the possibility of missing axillary metastases in this high-risk group.
Neoadjuvant chemotherapy
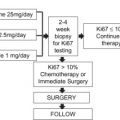
In early experience with SLN surgery, patients receiving neoadjuvant chemotherapy (NAC) were excluded from SLN surgery and underwent ALND at the time of their definitive breast cancer surgery after completion of chemotherapy. With increasing use of NAC for operable breast cancer and earlier-stage disease, data have accumulated on SLN surgery after completion of NAC. In early smaller series, the SLN identification rates ranged from 85% to 100% and the false-negative rate ranged from 0% to 33%. More recent studies have documented higher identification rates and lower false-negative rates.
In the National Surgical Adjuvant Breast and Bowel Protocol (NSABP) B-27 study evaluating NAC, 420 patients (18%) underwent SLN surgery after completion of chemotherapy. The SLN identification rate was 85% and the false-negative rate 11%. Recent meta-analyses have shown that SLN surgery after NAC is feasible and accurate. The initial meta-analysis in 2006 reported a pooled SLN identification rate of 90% and sensitivity of 88%. A more recent meta-analysis reported an overall SLN identification rate of 90% and false-negative rate of 8.4%.
The nodal status before chemotherapy provides staging information useful in adjuvant treatment planning for chemotherapy as well as adjuvant radiation. Therefore, one of the advantages of axillary staging before chemotherapy is that it may help determine which patients benefit from irradiation to the nodal basins because nodal staging is a strong predictor of local and distant failure. However, when the SLNs are removed before NAC, this limits the ability to evaluate the axillary response to NAC because the SLN, which may be the only positive node, is removed. In addition, this approach requires 2 operations, one at presentation for SLN surgery and the second after completion of NAC for definitive breast surgery. Also, patients who have node-positive disease detected by SLN surgery before chemotherapy undergo ALND after completion of NAC, even though preoperative chemotherapy eradicates nodal disease in up to 40% of patients with axillary nodal disease at initial diagnosis.
Performing SLN surgery after completion of NAC allows assessment of response to NAC. Status of the axillary lymph nodes after NAC has been shown to be the best prognostic indicator for patients with nodal disease. It also allows the nodal staging and definitive breast surgery to be performed at one operation.
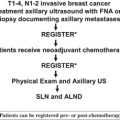
In the context of documented node positivity at presentation, ALND remains the recommended procedure after completion of NAC. Studies have reported false-negative rates of 11% to 29.6% in these patients. A multicenter trial evaluating this question is currently under way. American College of Surgeons Oncology Group ACOSOG Z1071 is a phase 2 prospective study evaluating the reliability of SLN surgery after NAC in women with documented node-positive breast cancer (T1–4, N1–2, M0) at presentation.
In the authors’ clinical practice, axillary ultrasound is routinely used with fine-needle aspiration (FNA) of suspicious nodes at the time of presentation. For patients receiving NAC, those who were node positive by FNA before chemotherapy undergo ALND and patients with normal-appearing lymph nodes or negative FNA undergo SLN surgery for axillary staging after NAC.
Previous breast surgery
With the increasing number of patients who have breast cancer with previous breast surgery, the question is raised about the feasibility and accuracy of SLN surgery in patients who have had previous breast and/or axillary surgery cosmetically, diagnostically, or therapeutically.
Published evidence in this regard is mostly limited to small, retrospective single-institution case series. Various SLN surgery techniques have been used in these settings with the use of blue dye, isotope, or both, and various injection methods have been described. Preoperative lymphoscintigraphic visualization has been used to ensure identification of SLN mapping before proceeding to SLN surgery.
Excisional Biopsy
SLN surgery has been shown to be reliable after prior excisional breast biopsy with a low false-negative rate, ranging from 0% to 15%, and high identification rate ranging from 81% to 99%. In the NSABP B-32 trial the false-negative rate was significantly higher in patients who had a prior excisional biopsy (15.3%) compared with those who had FNA or core needle biopsy for diagnosis (8.1%). Where possible, excisional biopsy should be avoided and percutaneous biopsy rather than excisional biopsy of breast lesions is advocated for preoperative diagnosis of malignancy. This option has been shown to increase negative margin resection, and also allows nodal staging with SLN surgery to be performed at the initial operation without a prior excisional biopsy.
Breast Augmentation
Despite the possibility of interruption of the breast and axillary lymphatics, there are several small series reports of successful lymphatic mapping and SLN surgery in the setting of breast implant augmentations. Jakub and colleagues examined the effectiveness of lymphatic mapping and SLN surgery in 49 patients with breast cancer who had prior implant breast augmentation with 100% identification rate, and no clinically detected axillary recurrences in the patients who had a negative SLN. Similar results have been reported in smaller studies. In the largest study to date by Rodriguez Fernandez and colleagues at the European Institute of Oncology in Milan, SLN surgery was performed with a 100% identification rate and no axillary recurrence after 19 months’ follow-up in 50 patients with breast cancer who had undergone breast augmentation previously. The augmentations were through inframammary or periareolar approach, which is less likely to cause disruption of the lymphatics to the axilla. There is more concern about the feasibility of SLN surgery in women who have had previous transaxillary breast augmentation. Lymphoscintigraphy has been reported successful in identifying the SLNs in these women, with emphasis of meticulous technique at the time of augmentation to minimize the dissection in the axilla. There are more limited data on this approach, with case reports of 2 women undergoing successful SLN surgery after transaxillary breast augmentation.
Breast Reduction
In breast reduction there is greater disruption of the breast tissue and lymphatics than with excisional biopsy or breast augmentation. The data on reliability of SLN surgery in axillary staging of patients with breast cancer who have had previous breast reduction surgery is scarce. Golshan and colleagues described 6 patients who underwent successful SLN surgery for occult carcinomas detected after breast reduction surgery, and concluded that SLN surgery should not be considered a contraindication after breast reduction surgery. In their recent study, Rodriguez Fernandez and colleagues reported on SLN surgery in 20 patients with breast cancer who had previously undergone breast reduction surgery showing a 100% SLN identification rate and no axillary recurrence after 19 months’ follow-up.
Overall data regarding SLN surgery after prior breast reduction are significantly limited, and this remains controversial. The use of SLN in these patients should be on a case-by-case basis. If the breast reduction was recent or the tumor is large, then ALND should be considered for accurate staging of the axilla. In women where the breast reduction was many years before the breast cancer, SLN surgery may be an option. Lymphoscintigraphy with mapping to document drainage patterns should be obtained and the patient should be counseled regarding the unknown false-negative rate.
Previous axillary surgery
Reoperative SLN surgery in patients with previous axillary surgery in the form of SLN surgery or ALND has been described. Port and colleagues reported on 117 patients with SLN surgery performed in patients with local recurrence after previous breast conservation surgery and either SLN surgery or ALND. The SLN identification rate was 55% (64 of 117). No axillary recurrences were observed at a median follow-up of 2.2 years. Multiple smaller single-institution series have been reported on SLN surgery in this setting. The SLN identification rate can be much lower than in patients without prior surgery, ranging from 55% to 100%. In addition, drainage of the breast to extra-axillary sites is much more common with reports of drainage to the internal mammary (IM) chain, contralateral axilla, and other sites, making lymphoscintigraphy with mapping important in surgical planning for these cases.
The SLN identification rate is higher when fewer than 10 axillary nodes have been removed previously. Although the SLN identification rate is generally low in these patients, SLN surgery in the setting of recurrent breast cancer can provide additional staging information of the recurrence that can guide adjuvant radiation and medical treatment recommendations.
Overall, data regarding SLN surgery in patients with previous axillary surgery are limited to small series and show higher rates of identification failures. As the number of lymph nodes removed at prior surgery increases, the likelihood of failure to identify the SLN and the likelihood of extra-axillary drainage increase, and patients should be counseled appropriately.
Internal mammary SLN surgery
Advent of SLN surgery allowed focused dissection to evaluate the status of the IM lymph nodes. Historically IM lymph nodes were not routinely sampled at the time of modified radical mastectomy, which raises some debate about the need for IM nodal staging. Information regarding IM nodal status can be used for staging, prognosis, and treatment decisions, and IM nodal involvement has the same significance as axillary nodal involvement in adjuvant treatment recommendations. Drainage to the IM lymph nodes is detected on lymphoscintigraphic mapping with use of parenchymal or peritumoral injection. Dermal and subareolar injections are less likely to demonstrate IM drainage. On visualization of the IM node as the first lymphatic drainage site, IM SLN surgery can be performed, provided the surgeon is comfortable with the procedure .
However, many centers do not perform preoperative mapping and argue against the need for extra-axillary SLN surgery. The issue of IM SLN surgery has been addressed in a recent systematic review by Chen and colleagues. Opponents of IM SLN base their view on the low incidence of isolated IM metastases in early breast cancer (up to 10%), low incidence of clinical recurrence in the IM nodal chain, and the lack of conclusive data on the survival benefits of IM resection or irradiation. In addition, as opposed to axillary SLN surgery, the accuracy of IM SLN biopsy has not been as vigorously studied and various injection techniques have been used.
In many recent series, on the other hand, the advocates of preoperative lymphoscintigraphic and IM SLN surgery have reported tailoring individualized treatment decisions, which have included employment of more intensive systemic treatment given the poorer prognosis with positive IM SLN, and addition of IM chain irradiation. However, the results of clinical trials are awaited to show whether these additional interventions can lead to better survival rates. Alternatively, in the case of negative IM SLN, “unnecessary” IM chain irradiation and its associated morbidities may be avoided.
IM SLN surgery significantly changes the treatment recommendations only in situations where there is a positive IM node and a negative axilla. The ASCO 2005 sentinel node biopsy guidelines leave the decision to perform IM SLN surgery procedure to the clinical judgment of the treating physicians. The 2010 National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines state that if the preoperative mapping identifies SLNs in the IM chain, IM nodal excision is optional. These guidelines also state that IM lymph nodes should be irradiated if clinically or pathologically positive, with the caveat that CT-based simulation should be used in radiotherapy planning to reduce cardiac and lung irradiation. At this time, evaluation of IM SLN remains controversial and varies from center to center.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree