Figure 4.1
Single rotation flap plan
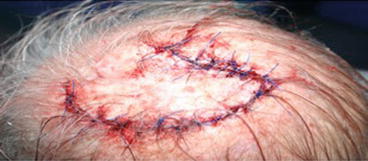
Figure 4.2
Single rotation flap sutures in place

Figure 4.3
Single rotation flap post op
Case Study 2
A 65 year old lady was referred to my clinic with a large 3 cm basal cell carcinoma on her scalp. A skin graft would had left her with a 3 cm area of hair loss. A skin graft would also result in a color-mismatched contour defect. It was not possible to close this defect primarily. I elected to use a double rotation flap (O to S flap) as the biomechanics and line of closure would not distort the hair pattern at the vertex and also allow for a smaller area of mobilization than if I had used a single rotation flap. The planning and biomechanics of the double-rotation flap is discussed (Figs. 4.4 and 4.5).



Figure 4.4
Double rotation flap plan

Figure 4.5
Double rotation flap sutured in place
Case Study 3
A 60-year old bald gentleman was referred with a large 3.5 cm exophytic lesion on his scalp which turned out to be a squamous cell carcinoma. Options of closure in this case involved a skin graft (given the gentleman was already bald), a single or double rotation flap. On examination of the scalp, due to previous radiotherapy to the scalp (not close to the present lesion) there was limited mobility to allow for a rotation arc of a single rotation flap. While, the O to S (double rotation flap) was also an option, I elected to use a tripolar-rotation flap given the location of the lesion at the vertex of the scalp. I have found this particularly useful on the vertex of the scalp where dissection of each of the pedicles is begun at 3, 7 and 11 O’clock positions. The planning of this flap is discussed. Unlike a ‘Mercedes Flap’ this flap is more a rotation than an advancement flap (Figs. 4.6 and 4.7). While there was some bruising of the flap at the end of surgery the flaps remained fully viable with no tip necrosis or need for any further dressings or procedure.



Figure 4.6
Triple rotation flap plan

Figure 4.7
Triple rotation flap sutured in place. The bruising was temporary and flaps remained fully viable
The Single-Rotation Flap
The classical rotation flap is pivoted around a fixed point at the base of the flap and rotated along an arc toward the defect (Fig. 4.8).
Figure 4.8
Rotation flap
Classically, rotation flaps are designed to move along an arc of 30° or less with the radius approximately two to three times the diameter of the defect and the arc length approximately four to five times the width of the defect [4].
Larrabee conducted a series of elegant experiments [5] to test the tension and closure lengths of rotation flaps. He created a series of single rotation flaps. The variables he measured included the radius of each semicircle, the size of the defect, and the amount of undermining that was needed to close the defect using the flap. He also measured the force needed to close the defect at each stage i.e. no flap (primary closure), 45° flap, 90° flap, 135° flap and 180° rotation flaps. What he found was that tension was concentrated at 90° and 135°. In other words, extending the semicircle of the flap beyond 135° did not allow for easier closure, although sometimes there were cosmetic indications for doing so (Fig. 4.9).
Figure 4.9
Rotation flap biomechanics
In another series of experiments, Throckmorton [6] and others studied the relationship between the length of the incision and the amount of linear movement required to cover a defect using a rotation flap by trigonometric analysis. Their analyses showed the amount of flap stretch required to close defects, assuming a 2-dimensional surface and uniform ‘deformation’ of the flap during rotation. They found that for any incision longer than twice the diameter of the defect, the linear distance that the flap must be rotated ends up between 1.0 and 1.5 times the diameter of the defect.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree