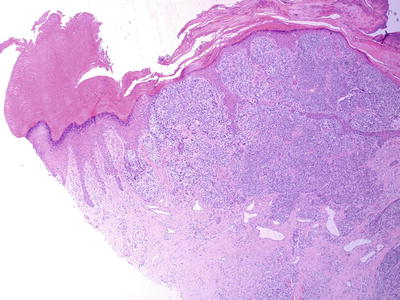
Figure 8.1
Toe melanoma
A 4 mm punch biopsy was taken under local anesthetic digital block. Histology was reported as ‘invasive malignant melanoma with Breslow thickness of at least 1.2 mm’.
The patient was referred to the local regional melanoma service where a partial amputation of the toe was performed together with sentinel lymph node biopsy of the L groin.
Histology was reported as follows:
(Histology report from initial partial amputation of 4th toe)
Macroscopic description
Partial amputation 43 × 6 × 18 mm. The toe nail bed area consists of red brown crusted tissue 14 × 15 mm and a fragment of nail 4 ×4 mm. Three representative samples have been processed through this area. Remaining tissue submitted for decalcification.
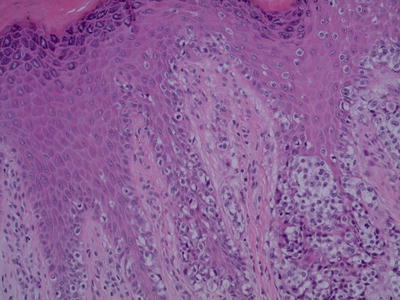
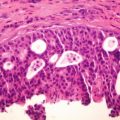
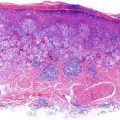
Microscopic description – synoptic report – malignant melanoma
Site – Left 4th toe
Breslow thickness 4.2 mm
Clark level 4 (at least)
Architectural type – acral lentiginous
Predominant cell type – epithelioid
In situ component – present
Invasive component – present
Mitotic index – 13 mitoses per square mm (5 high power fields)
Tumour infiltrating lymphocytes – absent
Microsatellites – absent
Perineural invasion – absent
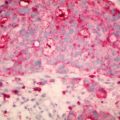
Lymphovascular invasion – present, lymphatic space invasion
Ulceration – present 5 mm wide
Regression – absent
Associated nevus – absent
Margins – in situ and invasive melanoma is completely excised with a minimum of 11 mm clearance of the proximal skin margin. Decalcified bone sections contain no melanoma
Sentinel lymph node biopsy was reported as positive with ‘multifocal & nodal deposits of metastatic melanoma with maximum diameter 4 mm’.
Further amputation of the L 4th toe was undertaken together with inguinal lymph node dissection. Two further lymph nodes were positive for metastatic melanoma.
Within 2 months the patient developed multiple small (<5 mm) purple coloured raised lesions on the skin of her dorsal foot. Biopsy confirmed local melanoma deposits suggestive of in-transit cutaneous metastases.
Staging CT scan of brain, chest, abdomen & pelvis showed two 2 mm pulmonary nodules and at least three L pelvic lymph nodes the largest 3 cm diameter.
Her current stage is 3B with an expected 57 % 5 year survival.
BRAF mutation testing was negative and she has now been commenced on Ipilimubab.
Discussion
White populations have a much greater risk of developing toe melanoma than Asians or Africans. Contrary to conventional wisdom non-white races overall have a much lower rate of the disease, they are just most likely to develop melanomas in acral locations such as the palmar, plantar surfaces and nail bed [11].
Melanoma of the toe is prevalent at different rates in black populations of America and Africa, getting some authors like Oettlé [12] to suggest that shoe-wearing may reduce the incidence of toe and foot melanoma. However, the following year, Lewis [13] studied several tribes in Uganda and concluded that shoe wearing did not make any difference. More recently, Green undertook a study of 275 melanomas diagnosed on the soles and palms to investigate risk factors and concluded that sun exposure was a significant risk factor in the development of ALM despite their plantar and nail bed location [14].
The iconic reggae musician, Bob Marley died in 1981 of an acral melanoma and one he had attributed to an injury while playing soccer barefoot. Indeed 23–44 % of patients report direct trauma as causing their subungual melanoma [15, 16]. While the overall incidence of acral melanomas is the same across all races, subungual melanomas represent approximately 20 % in dark-skinned and oriental populations compared to about 2 % of cutaneous melanomas in white populations [16]. Just as squamous cell carcinomas are reported after burns, Möhrle and others feel that in subungual melanoma, trauma is likely to be an etiologcal factor [16].
Does diabetes increase foot melanoma risk? In a case report about a diabetic foot ulcer that turned out to be a melanoma, the authors suggested that ‘one of possibilities for the relatively fast growth of acral lentiginous melanoma may point to the diabetes’ [17, 18]. However, there has been no causal link established between diabetes and toe melanoma. However, interestingly, Metformin when used in combination with melanoma drugs like bevacizumab shows synergistic effect. Metformin inhibits the growth of most tumor cells, but BRAF-mutant melanoma cells are resistant to metformin in vitro, and metformin even accelerates their growth in vivo. Unexpectedly, drugs used for advanced melanoma like VEGF inhibitors and metformin synergize to suppress growth of BRAF-mutant tumors, revealing that a combination of drugs may be effective in patients [19]. Other authors concluded that Metformin blocks melanoma invasion and metastasis development in AMPK/p53-dependent manner [20]. Therefore more work needs to be done in the realm of melanoma in diabetic patients and some diabetes medications seem to have a role in combination therapy.
Another interesting aspect of foot and toe melanoma is the different genetic mutations involved with acral melanomas when compared with melanomas in other cutaneous sites. Recent studies provide evidence that acral melanoma is distinct from common cutaneous melanoma at the genomic level, and show that the genomic landscapes of acral and mucosal melanomas are more similar to each other than to other subtypes [21]. These findings open the door to more research into managing these acral melanomas differently to cutaneous melanomas. This may also explain the differing mortality levels.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree