Proliferation genes
Ki-67
STYKI5
Loss of overexpression is associated with progression from DCIS to invasive breast cancer [24]
Survivin
Inhibits apoptosis; its expression is associated with DCIS recurrence [25]
Cyclin B1
Overexpression is related to DCIS grade, Ki-67, and HER-2 overexpression [26]
MYLBL2
More frequently seen in Luminal B versus Luminal A breast cancers; it is associated with resistance to tamoxifen [27]
Hormone receptor genes
Progesterone receptor (PR)
Other genes
GSTM1
Predicts distant recurrence and survival in patients treated and not treated with tamoxifen [18]
References genes
ACTB
–
GAPDH
–
GUSB
–
RPLPO
–
TFRC
–
The E5194 trial was initiated in 1997 and was chosen as the independent study for DCIS Score validation. Of the 670 patients enrolled in the trial, 327 (49 %) had tissue that was sufficient for analysis. This trial was designed to determine which clinical and pathologic features, if any, could predict a subset of patients at low risk for local failure without the use of adjuvant radiation [19]. Of the 327 patients who had sufficient tissue for DCIS Score validation, the tumor size was smaller than the 343 patients who were not included. There were no other differences between the two groups with respect to patient and tumor characteristics. The majority of patients in the E5194 validation study had a low-risk DCIS Score (n = 230). However, there were 53 patients who had intermediate-risk scores and 44 patients who had high-risk scores. This was somewhat surprising given that patients were enrolled into E5194 on the basis of “perceived” low-risk clinicopathologic features. As a result of this validation study, the DCIS Score was made available for commercial use for women with DCIS who were treated by wide local excision, with or without tamoxifen.
DCIS Score and Ipsilateral Breast Events
The relationship between DCIS Score risk group and 10-year risk of an ipsilateral breast event, whether in situ or invasive, was highly statistically significant (P = 0.006 for any ipsilateral breast event and P = 0.003 for an invasive ipsilateral breast event) [18]. This was true with or without the adjustment for tamoxifen use. For the 230 patients with a low-risk DCIS Score, the 10-year risk of any ipsilateral breast event was 10.6 % (95 % CI 6.9–16.2 %) and 3.7 % (95 % CI 1.8–7.7 %) for an invasive breast event. For the 53 patients with an intermediate-risk DCIS Score, the 10-year risk of any ipsilateral breast event was 26.7 % (95 % CI 16.2–41.9 %) and 12.3 % (95 % CI 5.1–27.8 %) for an invasive breast event. For the 44 patients with a high-risk DCIS Score, the 10-year risk of any ipsilateral breast event was 25.9 % (14.8–43.1 %) and 19.2 % (95 % CI 9.5–36.4 %) for an invasive breast event. Multivariable models of risk for ipsilateral breast events, both excluding and including the DCIS Score, were also performed. When the DCIS Score was excluded, tumor size and menopausal status were the only factors significantly associated with risk for an ipsilateral breast event (HR 1.54, P = 0.006 and HR 0.49, P = 0.02, respectively). However, when the DCIS Score was included in the model, the 12-gene score was statistically significant (HR 2.37, P = 0.02), in addition to tumor size and menopausal status. Tumor grade and the presence of comedonecrosis were not associated with a risk for ipsilateral breast events.
DCIS Score and Adjuvant Radiation Therapy Use
There is currently no known subset of patients with DCIS who do not benefit from adjuvant radiation for risk reduction following breast-conserving therapy. This is true regardless of patient’s age, tumor size, tumor grade, and margin status [30]. In the Early Breast Cancer Trialists’ Collaborative Group analysis, the risk of an ipsilateral breast event was decreased from 18.1 to 7.6 % at 5 years and 28.1–12.9 % at 10 years in patients with ≤ 2 cm of DCIS who underwent adjuvant radiation [30]. Despite this, survival is equivalent for excision alone and excision followed by adjuvant radiation therapy. Radiation therapy is not without risk. There are short-term side effects and potential long-term consequences, some of which can be devastating. In addition, the therapy is quite costly and access to care can be difficult for many patients. Are these risks and costs justified for all patients with DCIS?
The ability to identify a subset of patients who could safely omit radiation is desirable. Thus, patients who have undergone wide local excision for DCIS who have a low-risk score could reasonably elect to omit radiation therapy, while patients in the intermediate or high-risk groups should consider adjuvant radiation therapy and tamoxifen following wide local excision.
Limitations of the DCIS Score
Despite these promising findings, the DCIS Score has not yet been universally adopted for making treatment decisions. There are several important limitations. First, the E5194 study used to validate the DCIS Score included a narrow subset of patients with DCIS. Specifically, the study included patients already considered to be at low risk for recurrence, and included patients with small volumes of DCIS and with margins of at least 3 mm. Therefore, these results cannot be applied to women with larger volumes of DCIS or with closer surgical margins. In addition, only 30 % of the patients in the E5194 study received adjuvant tamoxifen therapy, and the absolute number of tamoxifen-treated patients included in the validation study was only 96 [18]. Because tamoxifen decreases the risk of both local recurrence and contralateral breast cancer events in patients with ER-positive DCIS [6, 31], use of tamoxifen would likely mean fewer recurrences for patients with all DCIS Scores. The ER gene was specifically excluded from the DCIS Score given that it specifically predicts benefit with tamoxifen therapy. For patients with ER-negative DCIS, the DCIS Score has not been adequately studied; only nine patients with ER-negative DCIS were included in the validation study (less than 3 % of the total cohort). Additional study is needed to verify these validation results across broader populations of patients with DCIS.
Although the DCIS Score is promising for stratifying patients by risk of in-breast recurrence, it does not supplant other patient and tumor characteristics such as tumor size and menopausal status, which remained significant predictors of recurrence with and without inclusion of the DCIS Score on multivariate analysis, P < 0.02 for each [18]. The DCIS Score is therefore a helpful addition to, but not replacement for, the use of already available clinicopathologic features used to make treatment decisions.
It is important to note that the DCIS Score does not equate with recommendations for or against post-lumpectomy radiation for patients with DCIS. Rather, it provides a guide regarding expected local recurrence, of either in situ or invasive disease, when radiation therapy is omitted. Established studies demonstrating the reduced risk of in-breast recurrence due to the addition of radiation [30] should be included in the treatment discussion with patients. It also does not stratify recurrence risk into risk of only in situ or of invasive disease, the latter of which is associated with potential mortality and need for more aggressive treatment, such as lymph node evaluation, extended radiation fields, chemotherapy, and biologic therapy. Such information would be particularly informative for guiding treatment decisions. In addition, the DCIS Score does not predict response to post-lumpectomy radiation. Indeed, a trial evaluating the utilization of the DCIS Score on outcomes would be of great interest.
Although the DCIS Score is associated with in-breast recurrence, the test cannot explain the behavior of individual DCIS cases: why does some DCIS remain indolent, and why do other cases progress to invasive disease? With this information, overtreatment may truly be prevented.
Beyond Risk of Local Recurrence: Which DCIS Has the Potential for Invasion?
There is an increasing amount of knowledge of the genetic features of DCIS, but there is still not a uniformly accepted understanding of how DCIS and invasive breast cancer are related. DCIS is associated with many invasive breast cancers and tends to have similar grade, nuclear morphology, and molecular subtype as the invasive component [32–35]. In addition, low-grade DCIS is genetically similar to low-grade invasive cancers with both frequently showing loss of the 16q and gain of the 1q chromosomal regions, and poorly differentiated DCIS and high-grade invasive cancers both demonstrate more frequent amplification of 17q12 [36, 37]. Despite these findings, not all DCIS lesions left unresected develop into invasive malignancies [38, 39].
Many investigators have analyzed synchronous ipsilateral DCIS and invasive breast cancer samples from the same patient in order to identify genetic similarities and differences between the in situ and invasive components. Many of these studies have focused on specific genes such as HER-2, MYC, and CCND1 [40–43], and there appears to be significant variation both between patients and within both in situ and invasive components in individual patients [40–46]. Because of this heterogeneity in these individual genes, it has proven difficult to identify universal genetic markers of progression to invasive disease [47].
Beyond Predictive and Prognostic Information
The capability to profile entire tumor genomes relatively quickly and affordably will continue to improve understanding of the relationship between DCIS and invasive disease [22, 40]. Instead of providing information only on individual genes and gene expression, next-generation sequencing or massively parallel sequencing offers the capability to delineate the genomics of a tumor with an unprecedented amount of detail. While this information may improve understanding of the development and behavior of DCIS and invasive cancer, the ultimate goal is to use this information to provide targeted therapies to prevent DCIS from ever evolving into an invasive cancer [23, 47].
References
1.
Ernster VL, Barclay J, Kerlikowske K, et al. Incidence of and treatment for ductal carcinoma in situ of the breast. J Am Med Assoc. 1996;275:913–8.CrossRef
2.
Schwartz GF, Solin LJ, Olivotto IA, Ernster VL, Pressman PI, Consensus Conference Committee. Consensus conference on the treatment of in situ ductal carcinoma of the breast, April 22–25, 1999. Cancer. 2000;88:946–54.PubMed
 History of Ductal Carcinoma In Situ Management Based Upon Data from Prospective, Randomized Clinical Trials
History of Ductal Carcinoma In Situ Management Based Upon Data from Prospective, Randomized Clinical Trials
 Ductal Carcinoma In Situ Treated with Breast-Conserving Surgery Alone
Ductal Carcinoma In Situ Treated with Breast-Conserving Surgery Alone
 Extent and Role of Margin Control for DCIS Managed by Breast-Conserving Surgery
Extent and Role of Margin Control for DCIS Managed by Breast-Conserving Surgery
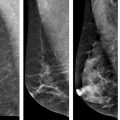 Role of Screening Mammography in Early Detection/Outcome of Breast Cancer
Role of Screening Mammography in Early Detection/Outcome of Breast Cancer
 DCIS and Hereditary Susceptibility for Breast Cancer
DCIS and Hereditary Susceptibility for Breast Cancer
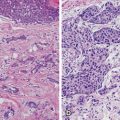 Pathology of Ductal Carcinoma In Situ: Features and Diagnostic Challenges
Pathology of Ductal Carcinoma In Situ: Features and Diagnostic Challenges
 History of Ductal Carcinoma In Situ Management Based Upon Data from Prospective, Randomized Clinical Trials
History of Ductal Carcinoma In Situ Management Based Upon Data from Prospective, Randomized Clinical Trials
 Ductal Carcinoma In Situ Treated with Breast-Conserving Surgery Alone
Ductal Carcinoma In Situ Treated with Breast-Conserving Surgery Alone
 Extent and Role of Margin Control for DCIS Managed by Breast-Conserving Surgery
Extent and Role of Margin Control for DCIS Managed by Breast-Conserving Surgery
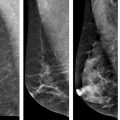 Role of Screening Mammography in Early Detection/Outcome of Breast Cancer
Role of Screening Mammography in Early Detection/Outcome of Breast Cancer
 DCIS and Hereditary Susceptibility for Breast Cancer
DCIS and Hereditary Susceptibility for Breast Cancer
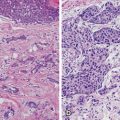 Pathology of Ductal Carcinoma In Situ: Features and Diagnostic Challenges
Pathology of Ductal Carcinoma In Situ: Features and Diagnostic Challenges
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


