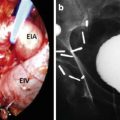
Fig. 6.1
Port position
The patient is then placed in extreme trendelenburg position. The robot is brought in and docked between the patient’s legs (Fig. 6.2). The assistant works from the patient’s right side.


Fig. 6.2
Docking of robot
Developing Space of Retzius
Visualization is initially performed with a 0° endoscope. Dissection is performed with curved monopolar scissors in the right robotic arm and bipolar forcep in the left robotic arm. The fourth robotic arm controls a grasper, such as a Prograsp forcep, and is used for grasping and retracting tissues.
To retract bowel from the surgical field and to help expose the lymph node packets, adhesions between the bowel and peritoneum are released. This most commonly is required on the left side where the sigmoid colon is released from the lateral peritoneum.
After transperitoneal access, the space of Retzius is developed and the dissection performed by an anterior technique. The bladder is dissected from the anterior abdominal wall by incising the peritoneum lateral to the medial umbilical ligaments. This incision is carried superiorly to the level of the umbilicus and inferolaterally to the level of the Vas Deferens. Care should be taken to avoid injury to the inferior epigastric vessels, which can cause troublesome bleeding or to carrying the dissection too far laterally in which case inadvertent entry into the iliac vessels may occur. The urachus is divided high above the bladder thus avoiding the presence of unnecessary tissue obstructing the field of view.
The plane between the bladder and anterior abdominal wall is then developed using a combination of blunt and sharp dissection. The correct plane is composed of fibrofatty tissue and is relatively avascular. Posterior traction on the bladder with the fourth robotic arm helps to correctly identify this tissue plane. If one is in the correct plane, one should see the pubic bone anteriorly. This dissection is continued inferiorly until the Endopelvic fascia is identified. Mobilization of the bladder is a key step in prostatectomy as it allows for a tension-free urethrovesical anastomosis to be performed.
The preceding technique, the Anterior Transperitoneal, is the most common approach to robotic prostatectomy. Another approach is the Transperitoneal Retrovesical approach in which the seminal vesicles and vas deferens are dissected first followed by bladder mobilization. Alternatively, an Extraperitoneal approach is also described but tends to be less commonly performed due to the smaller working space.
Opening Endopelvic Fascia
After release and mobilization of the bladder, the fat overlying the prostate is removed. Within this tissue lies the Superficial Dorsal Vein. It will usually lie in the midline and can lead to significant bleeding if not adequately coagulated.
At this point the endopelvic fascia and puboprostatic ligaments should be visible. Starting on the right side, the prostate is retracted medially. Opening of the endopelvic fascia is performed athermally using scissors towards the base of the prostate where the prostate is more mobile. This incision is then carried towards the apex of the prostate. The levator fibers are gently pushed away from the lateral and apical portions of the prostate (Fig. 6.3). The correct plane is avascular. If bleeding is encountered this raises the possibility that one is dissecting through the levator fibers.
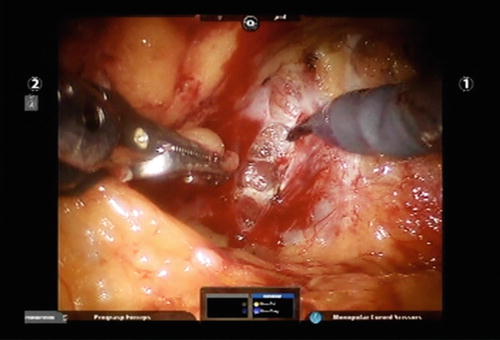
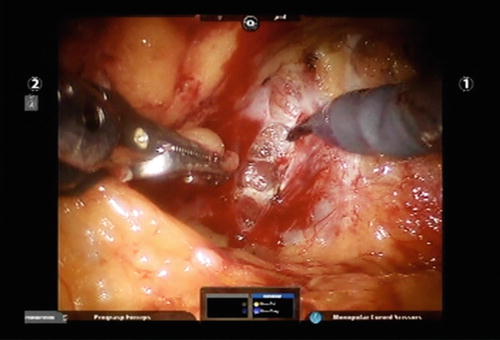
Fig. 6.3
Opening of endopelvic fascia
Towards the apex of the prostate, the puboprostatic ligaments are divided. In this area, the levator fibers may coalesce into a band of tissue requiring sharp dissection to free up the apical prostate.
The apical dissection proceeds until one identifies a notch between the dorsal venous complex anteriorly and the urethra posteriorly. A similar procedure is then repeated on the left side.
When excising the periprostatic fat or opening the endopelvic fascia, an Accessory Pudendal Artery may be encountered. When possible these arteries should be preserved. These may arise laterally coursing along the prostate, coursing above or below the endopelvic fascia or from an apical location. While these appear to be entering the prostate, they can often be dissected off the prostate using sharp dissection and bipolar cautery. Towards the apex they are in close association with the dorsal venous complex and prone to lead to venous oozing. Therefore, before performing this distal dissection, it may be wise to open the contralateral endopelvic fascia such that in case bleeding is encountered, one is prepared to suture ligate the complex. Apical dissection of Accessory Pudendal arteries proceeds until proximal suture ligation of the dorsal venous complex can be performed.
Ligation of Dorsal Venous Complex/Anterior Urethra Suspension
Various techniques have been described to control the dorsal venous complex. The complex can be suture-ligated with a 0-PDS suture on a CT-1 needle. The bladder is grasped with the fourth robotic arm and placed on cephalad traction. The notch between the dorsal venous complex and urethra is identified. The suture is passed anterior to the urethra (Fig. 6.4). After passage of the suture, both ends are grasped. The assistant then pushes the urethral catheter in/out to ensure that the suture has not caught the catheter. A second throw of the suture can then be performed and the complex secured with a square knot. Alternatively, after a single throw, a slipknot can be laid down to control the complex.
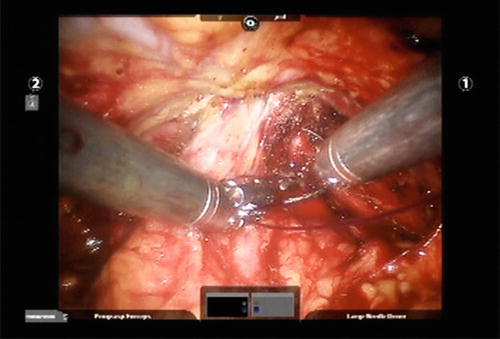
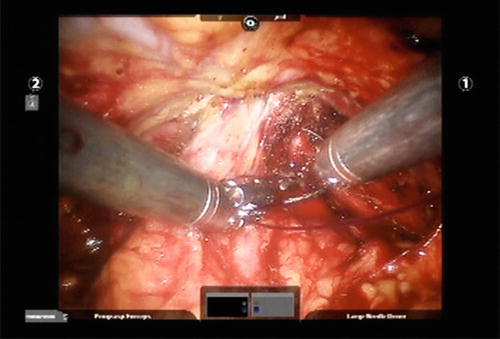
Fig. 6.4
Ligation of the dorsal venous complex
Another technique to control the dorsal vein involves the use of a laparoscopic stapling device. Conversely, while some techniques advise dividing the dorsal vein and suturing/stapling only if necessary, care should be taken in using this approach as bleeding can obscure visualization and increase the chance of a positive apical margin.
Anterior Bladder Neck
At this point it is helpful to switch to a 30° downward looking lens. While not necessary, this does help with visualization of the posterior bladder neck and during seminal vesicle dissection.
To delineate the correct plane and avoid entry into the prostate, the plane between the prostate and bladder is identified by advancing the urethral catheter in/out and applying gentle inward compression. Otherwise, the fourth arm can be used to tent the bladder anterocranially. Dissection is then initiated where the bladder tenting stops.
A horizontal incision is made in the bladder using monopolar cautery until the urethral catheter is visualized. The incision should not be made too laterally because bleeding from branches of the bladder pedicle can be encountered. The catheter balloon is then deflated and grasped by the fourth robotic arm. Simultaneously, the assistant clamps the catheter over a gauze just distal to the urethral meatus. The catheter is brought through the bladder incision and placed on cephalad retraction to elevate the prostate. Retraction can also be achieved by passing a holding suture through and through the abdominal wall, incorporating the eye of the catheter, and securing it to the outside.
Posterior Bladder Neck/Seminal Vesicle Dissection
Once the bladder is entered, the ureteral orifices are identified. In addition the presence of a median lobe should be ascertained (Fig. 6.5).
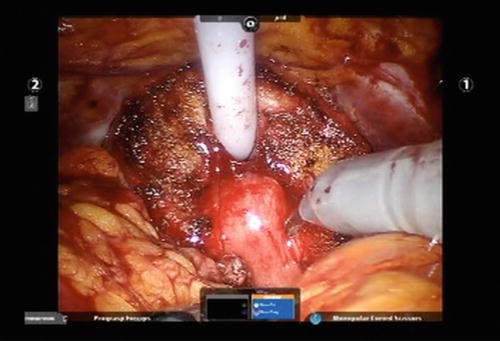
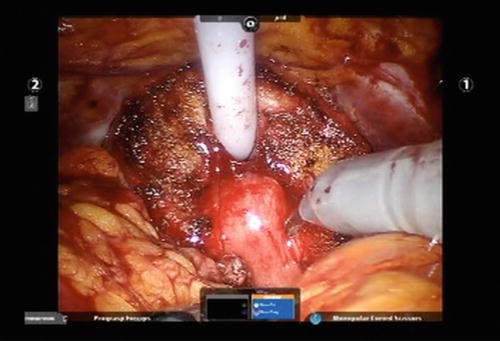
Fig. 6.5
Median lobe of the prostate. Prior to incising the mucosa below the median lobe, both ureteral orifices are identified
A horizontal incision is made in the posterior bladder neck using monopolar cautery. Dissection is carried at a 45° angle to avoid entry into the bladder or prostate. To avoid creation of an inadvertent cystotomy, frequent inspection of the bladder is performed.
Continuing along a 45° angle of dissection, one should identify the vasa deferentia in the midline. The depth of dissection can be estimated by considering that the thickness of the posterior bladder neck should approximate that of the anterior bladder neck. If it does not, or if the vasa deferentia are not encountered, this indicates that the plane of dissection is too superficial and may result in violation of the prostate. Furthermore, significant bleeding encountered in the midline or visualization of prostatic secretions is indicative of entry into the prostate. In each of the above cases, if one suspects entry into the prostate, one returns more cephalad and adjusts the angle of dissection more posteriorly.
If a prostate median lobe is present, division of the lateral bladder neck may be required to visualize beneath the median lobe and the posterior bladder neck. Again in the presence of a median lobe, identification of the ureteral orifices is critical. If required intravenous furosemide and indigo carmine can be administered. To aid with visualization, the median lobe is grasped with the fourth robotic arm and lifted anteriorly. Alternatively a 0 vicryl suture can be placed through the median lobe and lifted anteriorly by the assistant. Dissection must be below the median lobe as dissecting along its contour will result in incomplete resection and the vas and seminal vesicles will not be encountered.
Once the vas are identified, the fourth robotic arm releases traction on the urethral catheter and instead is used to grasp and retract the vas deferens anteriorly. Using blunt dissection the overlying tissue is released further mobilizing the vas. As the vas is lifted, this will bring up the corresponding seminal vesicle.
The arterial supply to the vas deferens typically runs between the vas and medial seminal vesicle. The vas is clipped and divided. The fourth robotic arm is repositioned to hold the proximal end and lifts anteriorly. When holding the vas, the wristed joint of the robotic instrument should be angled inferolaterally to maximize working space. Simultaneously, the assistant grasps the distal end and pulls laterally in the direction of the assistant port. This maneuver aids in visualization and exposure of the seminal vesicles. With the seminal vesicles exposed, the vas is released. The seminal vesicle is now held and lifted anteriorly with the robotic arm angled as described previously. With the seminal vesicle on traction, blunt dissection is used to free the gland proceeding from a medial to lateral direction. The blood supply originates inferolaterally and is controlled with clips. Electrocautery should be avoided as they may result in injury to the neurovascular bundle. After one side has completed, the same procedure is performed on the remaining vas deferens and seminal vesicle.
After both seminal vesicles and vas deferens have been dissected free, they are grasped with the fourth robotic arm and lifted anteriorly to provide exposure for the posterior dissection. Alternatively, they can be grasped on one side with the fourth robotic arm and on the other side by the assistant to provide anterior traction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree