Epidemiology and risk factors
The seasonality of respiratory virus infections among immunocompromised children is similar to that in the community ( Fig. 21.1 ). Respiratory syncytial virus (RSV) typically circulates in the community from November through March, with peak detection in January. Human metapneumovirus follows a similar pattern although often somewhat later. Influenza epidemiology can vary somewhat from year to year, with typical seasons lasting from December to March. Influenza A tends to be more predominant early in the season and influenza B is often seen later in the season. Up-to-date influenza surveillance data for the United States are published on the Centers for Disease Control and Prevention website ( https://www.cdc.gov/flu/index.htm ), and global surveillance data are maintained by the World Health Organization ( https://www-who-int.easyaccess2.lib.cuhk.edu.hk/influenza/surveillance_monitoring/updates/en/ ).
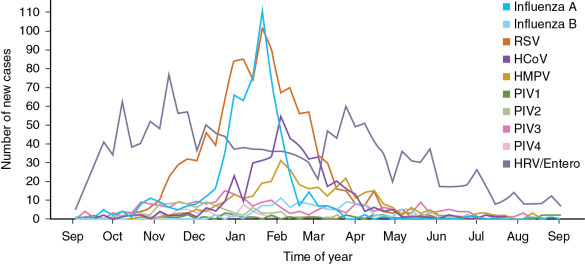
Parainfluenza viruses (PIVs) vary in seasonality by type. PIV-1 causes croup epidemics in the autumn, generally every other year. PIV-2 infections usually follow the same pattern as PIV-1 and PIV-3 outbreaks, usually occuring in the spring. PIV-3 remains the most common PIV subtype detected in both hospitalized and outpatient studies, but newer molecular epidemiology suggests that either PIV-1 or PIV-4 may be the second most common PIV detected in children, depending on the year. PIV-4 may be detected year-round. Human rhinoviruses (HRVs) and human coronaviruses (HCoVs) are present at moderate levels year-round, although there may be peaks of certain strains over the course of the year.
Exposure to sick contacts is the single most well-described risk factor for respiratory viral acquisition in immunocompromised children. Respiratory viruses are typically transmitted by respiratory secretions through direct contact, via fomites, or by large droplet spread. Entry generally occurs through contact with nasal mucosa or eyes, in contrast to the less permissive oral route. Transmission by small-particle aerosols of RSV has not been proven and, if it occurs, it is an infrequent route. Clinical observations suggest PIVs and human metapneumovirus (HMPV) are transmitted similarly to RSV. Although PIV-1 and PIV-3 have been recovered from air samples collected in the vicinity of infected patients, direct contact and transmission via fomites are likely to be more important. The high initial and subsequent infection rates, as well as outbreaks reported in hematopoietic cell transplant (HCT) recipients in both inpatient and outpatient settings, demonstrate that these viruses spread readily and that a relatively small inoculum is likely able to cause infection.
Epidemiologic patterns of respiratory viral detection in children are roughly similar among HCT recipients, solid organ transplant (SOT) recipients, and oncology patients, although risk factors for viral detection are unique.
HCT recipients.
In a surveillance study of pediatric and adult HCT recipients in the first year after transplant, the most common viruses detected were HRV and HCoV, followed by PIV, adenovirus, RSV, influenza, HMPV, and human bocavirus. In a separate multicenter retrospective study of pediatric HCT recipients, 16.6% of patient had at least one respiratory virus detected by PCR in the first year after HCT ; younger age was associated with viral detection in univariate analysis. Steroid exposure, neutropenia, and lymphopenia were commonly present in the week before respiratory viral onset.
SOT recipients.
In a large multicenter retrospective study of pediatric SOT recipients, the highest rates of inpatient respiratory virus infection occurred in intestine/abdominal multivisceral transplant recipients, followed by thoracic (heart/lung), liver, and kidney transplants. HRV was the most common detected virus (45% of respiratory virus events), followed by RSV (22%), PIV (16%), HMPV (11%), and influenza (10%). Lymphopenia was present in 22% of patients with respiratory virus detected, although this was not evaluated as a risk factor for acquisition.
Oncology patients.
In a large cohort of pediatric cancer patients with fever and neutropenia, at least one respiratory virus was detected in 46% of subjects. The most common respiratory viruses detected were HRV, RSV, PIV, influenza, adenovirus, and HMPV.
Clinical manifestations
In healthy individuals, most respiratory viral infections are associated with self-limited upper respiratory tract symptoms. Notable exceptions include a stronger association between RSV and bronchiolitis in young infants, PIV and laryngotracheobronchitis, and HRVs and reactive airway disease exacerbations. In immunocompromised patients, respiratory viral infections can be associated with prolonged shedding, lower respiratory tract disease, the need for supplemental oxygen, late airflow obstruction, and even death. Prolonged viral shedding can be associated with persistent respiratory symptoms or can be asymptomatic with durations up to 4 weeks (mean). Persistent shedding of PIV in asymptomatic immunocompromised patients for many months has been noted using sensitive molecular detection methods, and prolonged shedding has been described for HMPV, HCoVs, and HRVs. Impairment of T-cell function appears to be commonly associated in children with prolonged shedding; additional risk factors in HCT recipients include initial high viral load, use of steroids, and myeloablative conditioning.
Initial clinical symptoms related to RSV infection in immunocompromised hosts are similar to those in immunocompetent persons. Upper respiratory tract infection may progress to lower respiratory tract disease, with likelihood of progression probably related to immune status. Over 1 to 2 weeks, lower respiratory tract involvement may become evident by increasing respiratory distress, worsening hypoxia, and potentially, the need for assisted ventilation. Children or adults who acquire RSV or HMPV during or shortly after chemotherapy for malignancy may also have severe, life-threatening disease. Recovery after assisted ventilation for RSV and HMPV pneumonia occurs but remains uncommon despite advances in supportive care. The associated respiratory failure in severely immunocompromised patients may result in multiorgan system failure, with high mortality rates in patients requiring mechanical ventilation. , Severe and fatal infection attributed to HMPV has been reported in cancer patients, and HMPV is a relatively common cause of acute respiratory infection in children and adults with malignancy, HCT recipients or organ transplant recipients. Risk factors for severe HMPV infection include lymphopenia. , , Quantitative bronchoalveolar lavage (BAL) viral load has not been associated with mechanical ventilation or death for RSV, PIV, or HMPV in adult patients after HCT; however, the detection of respiratory virus RNA in serum has been associated with fatal outcomes.
PIV infection with lower respiratory tract disease in immunosuppressed patients, particularly those in the immediate posttransplantation period, may result in a similar clinical picture, although the overall mortality rate may be less than that associated with RSV. , Many immunocompromised adults with PIV infection first present with symptoms of mild upper respiratory tract disease, but in contrast to RSV, influenza, and HMPV, detection of PIV-1 and PIV-3 in asymptomatic HCT recipients is relatively common, reported in 6 of 17 (35%) infection episodes in a prospective study. Fewer than half of PIV-infected patients have a fever. In severely immunocompromised patients, such as allogeneic HCT recipients less than 100 days after transplant, PIV-3 is the most common PIV subtype detected, reported in 80% of 544 HCT recipients with PIV. In all PIV-infected transplant recipients, infection may progress to lower respiratory tract disease with more serious disease linked to supplemental oxygen requirement, low monocyte counts, and high-dose steroid use. The detection of PIV in BAL or other lower respiratory tract specimens is associated with decreased survival overall in HCT recipients. Higher pretransplant PIV-3 antibody levels were not protective against severe sequelae. Concomitant infections with other viruses, fungi, or severe graft-versus-host disease are relatively common in adult patients with PIV pneumonitis.
Influenza remains a significant cause of morbidity and mortality in immunocompromised children and adults. In a recent multicenter review of immunocompromised children hospitalized with influenza, immunocompromised children were more likely to present with fever and less likely to present with respiratory distress. They were also less likely to require intensive care but were hospitalized longer. In a study of adult and pediatric HCT and SOT recipients, 22.1% of subjects presented with pneumonia and 66.5% were hospitalized. Prior vaccination was associated with decreased disease severity. Mortality after influenza was 2.9% in adults and 0% in pediatric patients in this study, although higher mortality rates have been previously reported.
With the increased use of molecular diagnostic assays, HRVs and HCoVs are now the most common respiratory viruses detected in immunocompromised patients. HRV can be detected in 20% to 30% of HCT recipients, with progression to lower respiratory tract infection occurring in 17% of patients. , Once HRV progresses, mortality rates can be similar to other respiratory viruses, including influenza, PIV, and RSV. In addition to HRVs, other members of the Enterovirus genus, including Enterovirus-D68, can be associated with outbreaks and severe disease. Enterovirus D68 was associated with several hundred cases of severe respiratory illnesses in children in the United States in 2014 and 2018; severe disease was also seen in immunocompromised patients. HCoVs can also be associated with severe disease in the lower respiratory tract and can result in death. Specific considerations for HCT, SOT, and oncology patients are outlined in the following text.
HCT recipients.
HCT recipients of all ages may have a more fulminant course after respiratory viral infections, particularly if infection occurs around the time of transplantation. Risk factors for disease progression include lack of engraftment, decreased lymphocyte count, and older age. Evidence of pulmonary infiltrates on chest radiographs may be delayed or absent in patients with severe neutropenia but may become apparent after immune reconstitution or on chest computed tomography or magnetic resonance imaging. In a multicenter retrospective review of pediatric HCT recipients, the all-cause and attributable case-fatality rates within 3 months of hospitalized respiratory viral infection onset were 11% and 5.4%, respectively. Lower respiratory tract infection was rare except in HMPV infections; fever was more common for influenza and HMPV. Multivariate models indicated that onset within 60 days of HCT, steroid use in the 7 days before onset, and the need for respiratory support at onset were associated with subsequent morbidity or death. Several risk scores have been proposed for adult HCT recipients with respiratory virus infections to predict the risk of progression to lower respiratory tract infection and mortality.
SOT recipients.
In a large multicenter retrospective review, fever was the most common clinical sign detected, although a significant proportion had signs of lower respiratory tract infection at onset (35%). Detection of any respiratory viral infection in SOT recipients was associated with an all-cause and attributable case-fatality rate of 4% and 0%, respectively. Receipt of an abdominal/intestinal multivisceral transplant was associated with increased risk of all-cause death in multivariable models. Overall, approximately 50% of patients with respiratory viral infections required some form of respiratory support.
Oncology patients.
Adults with leukemia and profound chemotherapy-induced myelosuppression are also at risk of fatal outcome from respiratory viruses. In pediatric patients with fever and neutropenia, episodes caused by different types of respiratory viruses had no differences in the clinical outcome (days of hospitalization, days of fever, oxygen requirement, admission to the intensive care unit, and death) and when comparing patients with a single virus versus coinfection.
Disease prophylaxis/prevention
Influenza vaccination
The mainstay of influenza prevention in immunocompromised children is vaccination. Inactivated influenza vaccine (IIV) is recommended for all patients 6 months and older with hematologic malignancies by the Infectious Diseases Society of America (IDSA) guidelines. Vaccination is not recommended for in patients receiving intensive chemotherapy, such as induction or consolidation chemotherapy for acute leukemia, or those who have received anti–B-cell antibodies in the past 6 months. Live attenuated influenza vaccine (LAIV) should not be used for immunosuppressed patients except in an outbreak setting when LAIV is determined to be a more effective option owing to strain type. Quadrivalent vaccine should be offered when available. Studies are ongoing to assess the immunogenicity and safety of high-dose influenza vaccination in immunocompromised adults and children.
Influenza vaccination is recommended for all family members, close contacts, and health care workers caring for immunocompromised patients. LAIV is not recommended for household contacts of HCT recipients (within 2 months after transplant), or those with severe immunosuppression as the result of graft-versus-host disease or severe combined immune deficiency. If LAIV is given to persons caring for severely immunosuppressed patients, the Centers for Disease Control and Prevention guidelines recommend avoidance of contact for 7 days after vaccination.
HCT recipients.
Immune responses to influenza vaccination are likely more effective further out from HCT. HCT recipients 6 months or older should receive IIV annually starting 6 months after transplant or starting 4 months after transplant during a community outbreak of influenza, with second doses recommended for children depending on time from transplant. In reduced intensity HCT, pretransplant vaccination may be appropriate as host immunity is expected to extend into the early transplant period. High-dose vaccination is currently under study in pediatric and adult HCT recipients.
SOT recipients.
IDSA guidelines recommend against administering influenza vaccine during intensified immunosuppression, including the first 2-month posttransplant period, because of the likelihood of inadequate response. However, during a community outbreak, IIV can be administered 1 month or later after transplant. Earlier vaccination has been supported by recent studies, and more data regarding high-dose vaccine and repeat vaccine dosing within a season are also becoming available.
Oncology patients.
IIV is recommended for all patients older than 6 months with hematologic malignancies, although IDSA guidelines do not recommend vaccination in patients receiving intensive chemotherapy, such as induction or consolidation chemotherapy for acute leukemia, or those who have received anti–B-cell antibodies in the past 6 months. Although immune responses are generally lower in children with malignancies, a recent Cochrane review demonstrated reductions in respiratory infections and hospitalization; however, the quality of evidence is low.
Influenza chemoprophylaxis
Postexposure chemoprophylaxis should be considered in immunosuppressed patients who are in close contact with confirmed influenza cases or during influenza outbreaks. In outbreak settings, HCT recipients should receive vaccine immediately if they are 4 months or longer posttransplant. Chemoprophylaxis with oseltamivir or zanamivir should also be initiated for 2 weeks after vaccination while immunity develops. Chemoprophylaxis is also recommended for HCT recipients who are less than 24 months posttransplant or those who remain substantially immunocompromised at 24 months or longer after HCT, regardless of vaccination history. For SOT, similar concerns regarding vaccine response in the early posttransplant period exist and chemoprophylaxis should be considered, although recommendations regarding the timing of this strategy are lacking. Season-long prophylaxis has been evaluated in a randomized trial of SOT and HCT and showed reduction in culture- or polymerase chain reaction (PCR)-confirmed influenza, although this approach is not universally used and may be targeted to periods of high influenza virus circulation. Antiviral resistance may emerge with widespread prophylaxis; drug resistance patterns of circulating strains should be considered when initiating prophylaxis and/or preemptive therapy.
Other vaccines in development
New advances in the understanding of RSV and HMPV, including the characterization of the RSV fusion (F) protein in its preinfusion and postfusion states, have contributed to the development of new RSV vaccines and monoclonal antibodies with the potential to be used for prophylaxis against RSV. Vaccines stimulating antibody directed to the F protein, and specifically to the pre-F protein, are now under development. RSV-specific serum-neutralizing antibodies are efficiently transferred from the mother to the newborn, and ongoing clinical trials may offer potential protection against RSV in family members and health care workers surrounding immunocompromised patients, with the potential to protect these patients. Candidate vaccines against PIV and HMPV, as well as chimeric vaccines containing genes from more than one virus, have also been tested in preclinical models.
Prophylaxis for other viruses
The identification of serum-neutralizing antibody as a correlate of protection against serious RSV lower respiratory tract disease has been an important advance. Although a humanized monoclonal antibody directed against the RSV F protein, palivizumab, has been licensed since 1998 to prevent RSV disease in young children with underlying cardiac or pulmonary disease, it is also currently used in children who are severely immunocompromised, such as infants with severe combined immune deficiency or congenital leukemia. Children younger than 24 months who are profoundly immunocompromised may be considered for palivizumab prophylaxis. The development of a potent and long-acting RSV monoclonal antibody directed against the pre-F protein of RSV is undergoing clinical trials in young infants. This, or similar products, may be available in the future to prevent RSV infection or disease in transplant candidates. Passive immunoprophylaxis against PIV and HMPV infection has not been studied in children.
Diagnosis
Sample type and handling
The diagnosis of respiratory viral infections is critically dependent on the type and quality of the clinical specimen and proper handling of the specimen. The preferred specimens for the diagnosis of respiratory viruses in immunocompromised hosts are respiratory secretions obtained as a mid-turbinate or nasopharyngeal swab, nasal wash, nasal aspirate, or bronchoalveolar lavage. A nasal wash specimen is the classic sample used for viral diagnosis by culture and for obtaining samples to assess cytokines or antibodies.
Nasopharyngeal swabs and mid-turbinate swabs are not as sensitive as nasal washes for viral diagnosis using culture but have good diagnostic yields with molecular detection methods. In general, molecular methods of detection are preferred over fluorescent antigen-antibody detection or antigen detection tests in immunocompromised patients. Specimens from children are often more readily diagnosed than those from adults owing to higher viral loads. Other clinical specimens useful for the detection of respiratory viruses in patients of all ages include endotracheal aspirates collected from intubated patients, bronchoalveolar lavage, nasal mucosal epithelium collected by scraping, sputum, and lung tissue obtained by biopsy or at autopsy.
Nucleic acid detection
Molecular diagnostics, such as multiplex real-time PCR, have replaced cell culture, fluorescent antigen-antibody detection, and antigen detection methodologies because they have high sensitivity and specificity, excellent quality control procedures, and detect a large battery of viral and bacterial pathogens rapidly in a single sample. The use of molecular diagnostics has significantly improved the yield of detection. Numerous rapid multiplex PCR assays are now commercially available that can detect up to 18 or more viruses simultaneously. These assays are sensitive and specific and can detect RSV, HMPV, influenza, HRVs, and HCoVs and differentiate all four PIV subtypes.
Treatment
Supportive treatment
The potential hypoxemia, apnea, and poor oral intake resulting from infection in young infants, both previously healthy as well as moderately or severely immunocompromised, requires close medical management. Hospitalization may be required for immunocompromised children younger than 1 year, particularly if intravenous (IV) fluid replacement and oxygen therapy are necessary. Systemic or inhaled steroids and bronchodilator therapies are not recommended for treatment of RSV, based on studies that failed to show decreased time in the hospital or improved outcomes. Children with airway obstruction or signs of hypoxia require admission to an intensive care setting for close monitoring, and children with severe disease may require intubation. Supportive care for lower respiratory tract infections caused by PIV and HMPV in immunocompromised hosts similarly may require hospitalization and adjunct therapy, including IV fluids and oxygen support, as well as aggressive therapy of secondary fungal, bacterial, or viral infections.
Antiviral treatment
Respiratory syncytial virus.
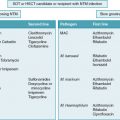
Ribavirin, a synthetic guanosine nucleoside, has been licensed for the treatment of RSV respiratory disease in children since 1986 and for the treatment of RSV disease in patients undergoing mechanical ventilation since 1993. Ribavirin is the only approved drug for lower respiratory tract disease caused by RSV, but concerns regarding efficacy, difficulties in administration, and the extremely high cost of the drug have resulted in minimal current use of the drug. Ribavirin is available in aerosolized, oral, and IV forms. Several retrospective studies, including a pooled analysis, have shown aerosolized or oral ribavirin is protective against disease progression to lower respiratory tract infection and mortality in HCT recipients; however, conclusive evidence of efficacy from randomized trials is not available. In patients with leukemia, multivariate models demonstrated similar effects. Oral ribavirin has been retrospectively evaluated in patients receiving chemotherapy or in HCT recipients, suggesting a possible effect of oral ribavirin; however, lack of randomized controls has been a limitation in all studies.
In adult HCT and hematologic malignancy patients with RSV lower respiratory tract infection, use of aerosolized ribavirin was associated with decreased mortality. Oral or IV ribavirin although not statistically significant as the effect was smaller. , Of note, some data suggest pediatric HCT recipients with RSV have little morbidity and mortality even without ribavirin therapy. Current international guidelines recommend aerosolized or systemic (oral or IV) ribavirin with intravenous immunoglogulin (IVIG) in patients with RSV upper respiratory tract infection undergoing allogeneic HCT, allogeneic HCT recipients with risk factors for progression to lower respiratory tract infection, and allogeneic HCT patients with lower respiratory tract infection. Recommendations for ribavirin administration for HCT and SOT recipients, and oncology patients are outlined in Table 21.1 . Most data and guidance for use of ribavirin are in HCT and oncology; few studies have clearly demonstrated efficacy in SOT recipients, and most data are in lung transplant when both oral and IV ribavirin have been used, For HCT and oncology patients, high-risk situations include patients with lymphopenia; additional risk factors, such as smoking history and use of high-dose total body irradiation, could be used to further risk-stratify patients. In general, aerosolized ribavirin is reserved for subjects with virologically confirmed (BAL positive for RSV) lower respiratory tract infection. It is administered by small-particle aerosol from a solution containing the drug at a concentration of 20 mg/mL sterile water via aerosol for 2 to 20 hours/day, or at a concentration of 60 mg/mL water over 2 hours 3 times daily. Aerosol administration results in high levels of ribavirin in the secretions, with levels exceeding 1000 μM and little systemic absorption. The potential environmental release of ribavirin has caused concern in hospital personnel because of the potential teratogenicity of ribavirin and thus exposure is contraindicated in pregnant women because of its teratogenic potential. Administration of ribavirin via a ventilator, using a high-dose, short-duration method of drug delivery or with a vacuum-exhausted treatment hood, results in minimal or no detectable ribavirin in the rooms of treated children.