Rectal Cancer
EPIDEMIOLOGY
In 2013 there were approximately 143,000 Americans diagnosed with colon and rectal cancer. Approximately 2/3 will involve the colon and 1/3 the rectum. Epidemiological factors and pathogenesis are similar for rectal cancer as for colon cancer.
ANATOMY
The rectum is generally divided into three portions: lower rectum, mid-rectum, and upper rectum. The distances from the anal verge are approximations and may vary with flexible endoscopic techniques.
• Lower rectum: 4–8 cm from anal verge
• Mid-rectum: 8–12 cm from anal verge
• Upper-rectum: 12–16 cm from anal verge
• Anal canal: 4 cm in length
 IMPORTANT LANDMARKS
IMPORTANT LANDMARKS
Dentate Line
The dentate line is the transition point between the squamous mucosa of the anus/perineum and the columnar mucosa of the rectum. Below the dentate line, the lymph drainage flows through the inguinal nodes and has implications for treatment.
Rectum/Sigmoid Boundary
In contrast to the sigmoid colon, peritoneum does not cover the circumference of the rectum. Rectal cancer has higher rates of local failure following surgery than colon cancer and requires aggressive local treatment.
Generally, rectal tumors should be no less than 6–7 cm from anal verge if a sphincter sparing operation is to be attempted in order to preserve muscle function while obtaining adequate margins.
DIAGNOSIS AND STAGING
 DIAGNOSIS
DIAGNOSIS
Presenting Symptoms
The majority of patients diagnosed with rectal cancer present with symptoms, although many are nonspecific and this may lead to a delay in diagnosis. Common symptoms include bleeding (gross or occult), constitutional symptoms, abdominal pain, changes in stool caliber, and changes in bowel habits.
WORKUP
When cancer is in the differential diagnosis, the workup entails history and physical including digital rectal examination (DRE), complete blood count, liver and renal function tests, carcinoembryonic antigen (CEA), and endoscopy.
DRE DRE should be used to assess the location of the tumor in relation to the anal verge, the dentate line, and the anal sphincter. If possible, the tumor should be assessed with respect to anal sphincter involvement, circumferential extent, and possible fixation to normal structures. Baseline sphincter tone should be assessed.
Rigid proctosigmoidoscopy This is used both to assess the location of the tumor (especially when nonpalpable), and to take biopsies for tissue diagnosis.
 STAGING
STAGING
Staging system
Rectal cancer is staged using clinicopathological parameters and classified using the AJCC TNM system (see Table 47-1). Preoperative staging is used for prognostic purposes and to estimate the risk of recurrence after surgery to guide adjuvant therapy.
T and N Stage
Endorectal ultrasound and MRI are commonly used to assess the extent of the primary tumor. Nodal status can be determined using MRI, CT, and EUS, but may be difficult to assess radiographically.
Endorectal Ultrasound (Eus)
EUS is able to distinguish the five layers of the rectal wall with good spatial resolution. The accuracy for T stage ranges from 67% to 97% with a propensity to overstage tumors as indicated by a reported specificity of 24% for peri-rectal penetration. EUS is operator dependent and associated with a fast learning curve (1, 2).
Magnetic Resonance Imaging (Figure 48-1)
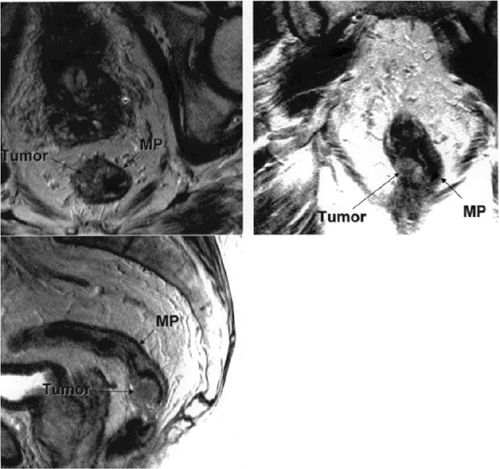
FIGURE 48-1 (Clockwise from lower left) sagittal, axial, and coronal T2 weighted MRI of the pelvis showing a rectal tumor invading through the muscularis propria (MP) making this a T3 lesion.
When MRI is used for primary determination of T stage, a surface phased array coil is employed enabling differentiation of rectal wall layers. Accuracy is operator dependant with interrater accuracies in one study of 67% and 83%. MRI can also be used for preoperative assessment of the likely circumferential margin (CFM) following surgery. The accuracy of N stage evaluation is similar to that of CT in that both are based on size criteria (3).
Assessment of Metastatic Disease
Computed tomography (CT) CT is used primarily for preoperative assessment of metastatic disease in the lungs, liver, or abdomen. It is less useful for the assessment of T stage with accuracy rates of only 33%–77% resulting from the inability to distinguish layers of rectal wall. The sensitivity for detection of nodal disease ranges from 45% to 73% (1).
Residual or Recurrent Disease
Positron emission tomography may be used for the assessment of residual or recurrent disease and may be helpful in areas of scarring or radiation changes (1).
TREATMENT
A general treatment algorithm is included in Figure 48-2.
FIGURE 48-2 Treatment algorithm. The type of surgery (LAR, APR) depends on the location of the tumor and the ability to spare the anal sphincter while maintaining adequate surgical margins. Chemoradiation consists of 5FU given concurrently with radiation to a pelvic field.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree