Summary of Key Points
- •
In patients with clinically nonmetastatic small cell lung cancer (SCLC), positron emission tomography–computed tomography (PET–CT) as well as brain imaging is suggested to classify tumor stage.
- •
To classify stage, it is recommended to use the Veterans Administration system (limited disease [LD] vs. extensive disease [ED]) as well as the International Union for International Cancer Control TNM Classification of Malignant Tumors seventh edition (2009), which recommended tumor, node, and metastasis (TNM) staging based on analysis of the International Association for the Study of Lung Cancer database. The prognostic value of clinical and pathologic T and N staging in patients with SCLC is confirmed in the eighth edition. For the M descriptors, more research is warranted.
- •
In patients with nonmetastatic SCLC or LD, combined chemoradiation is the standard. Concomitant chemoradiotherapy gives the best results and is preferred to sequential chemoradiotherapy, but the latter can be an option in fragile patients. Compliance with alternating regimens may be difficult, but promising results have been published.
- •
In fit, nonmetastatic SCLC patients, early chemoradiotherapy is recommended. In more fragile patients, for whom good compliance with early concomitant chemoradiotherapy cannot be expected, there is no survival advantage with early chemoradiation.
- •
A randomized phase III trial showed no difference between once-daily (66 Gy/33 fractions per 6.6 weeks) and twice-daily radiation (45 Gy/30 fractions per 3 weeks) given along with chemotherapy for patients with LD-SCLC.
- •
In patients with nonmetastatic SCLC who achieve a complete or partial response to initial therapy, prophylactic cranial irradiation (PCI) at the dose of 25 Gy in 10 daily fractions is recommended. It should not be administered concomitantly with chemotherapy.
- •
In metastatic SCLC, PCI is also recommended among patients with any response to chemotherapy based on a randomized trial and the meta-analysis. The same regimen (25 Gy/10 fractions per 2 weeks) or a more hypofractionated regimen (20 Gy/5 fractions per 1 week) may be administered. A recent Japanese study showed a decrease in brain metastasis rate but failed to demonstrate survival advantage with PCI in patients with extensive stage SCLC, but mature data are awaited.
- •
Patients should be informed of potential adverse effects on neurocognitive functioning that may be caused by PCI especially in elderly patients to balance the benefit of PCI on survival and risk of brain metastases.
- •
In patients with ED-SCLC who have completed chemotherapy and achieved a response, a course of consolidative thoracic radiotherapy (TR) is suggested by the results of a randomized trial. A subgroup analysis has shown that among patients with partial response in the chest, but not complete response, consolidation TR had an impact on survival.
Small cell lung cancer (SCLC) represents less than 20% of all lung cancers. It is an aggressive tumor, and only a third of patients have limited stage disease at diagnosis. As SCLC has a high propensity for early metastatic dissemination, chemotherapy has been and still is the cornerstone of treatment, but SCLC is also very sensitive to radiotherapy (RT).
Patients often have bulky mediastinal disease at presentation. After staging procedures, SCLC was classically presented as LD or ED according to the Veterans Administration Lung Cancer Study Group Classification. LD was defined as confined to a hemithorax and the regional lymphatic nodes (mediastinum, ipsilateral, and contralateral hilar regions, and supraclavicular fossa), thus theoretically encompassable with an RT field. Although this classification has been used for many years, the International Association for the Study of Lung Cancer has recommended the use of the new TNM classification for nonsmall cell lung cancer (NSCLC) for SCLC as well. The seventh and the future eighth TNM classifications split patients into a larger number of prognostically homogeneous subgroups, which could better define those patients for whom thoracic RT (TR) might be beneficial. Recent advances in the management of SCLC are principally attributed to the improved knowledge of the indications for RT, both in nonmetastatic (or limited) and in metastatic (or extensive) diseases. By contrast, in the last two decades, chemotherapy progress has reached a plateau. The integration of TR with systemic chemotherapy in SCLC as well as PCI is really a “unique success story in the field of radiation oncology and highlights the potential for effective local therapy to impact overall outcomes.”
This relative “success story” started with the publication in the early 1990s of an individual patient data-based meta-analysis of randomized trials comparing combined chemoradiotherapy with chemotherapy alone, which demonstrated an absolute overall survival (OS) benefit of 5.4% in favor of combination therapy (3-year OS of 8.9% vs. 14.3% in the chemoradiation arm). Pignon and colleagues collected and analyzed individual data from 13 trials involving 2140 patients with LS-SCLC: the relative risk of death in the chemoradiation group, as compared with the chemotherapy alone group, was 0.86 (95% confidence interval [CI], 0.78–0.94; p = 0.001). This equated to a 14% reduction in death with the addition of radiation. Warde and Payne published similar findings in a literature-based analysis of 11 randomized trials. They showed that the addition of TR to chemotherapy led to an overall benefit of 5.4% on 2-year survival, and an improved 2-year intrathoracic tumor control (from 16.5% in the chemotherapy arm alone to 34.1% in the combined modality arm), resulting in a benefit in local control of about 25%. The combination of chemotherapy and RT became a standard in the early 1990s after the publication of these two meta-analyses. Subsequently, these benefits have been confirmed by other studies. The current state-of-the-art treatment for SCLC patients with nonmetastatic disease involves cisplatin (or carboplatin in more fragile patients)–etoposide chemotherapy combined with chest RT, as reported in guidelines worldwide.
It is possible, however, that the two reported meta-analyses underestimate the results that can be obtained with platinum-based chemotherapy and contemporary RT as only a few studies included in the meta-analyses used platinum-based chemotherapy and concurrent chemoradiation, which are considered nowadays as part of the optimal treatment approach.
There are indeed different ways of combining chemotherapy and TR: they can be administered concurrently, sequentially, or in an alternating fashion. Furthermore, the issue of timing of RT has also been addressed in randomized trials: whether radiation should be given early or late in the overall course of treatment has long been a subject of debate. Sequential schedules allow the delivery of full-dose chemotherapy followed by full-dose RT; tumor shrinkage can be observed after systemic therapy, but repopulation and selection of resistant cellular clones may lead to treatment failure. The alternating schedule has a good toxicity profile, although from a practical point of view, it may be a complicated approach; the good results obtained in a French Study group randomized trial could not be reproduced by a larger European Organization for Research and Treatment of Cancer (EORTC) study. The concomitant approach has the radiobiologic advantage of reducing the overall treatment time, which is a particularly relevant issue in SCLC treatment, although it is associated with an increased risk of acute toxicity, especially esophagitis. Even so, this latter approach has now become the standard of care.
Two phase III trials have studied alternating schedules: an EORTC study, which compared an alternating chemoradiation regimen with a sequential regimen, and the “Petites Cellules” study, which compared an alternating regimen with a concomitant chemoradiation approach. It should be noted that none of these trials used platinum-based chemotherapy. Results were poor in both trials, with no difference in terms of OS between the two arms (median 15 months vs. 14 months in the first study; 13.5 months vs. 14 months in the second one).
The Japan Clinical Oncology Group (JCOG) performed a phase III trial comparing a sequential and concurrent chemoradiation approach. A total of 231 patients with LD-SCLC were randomly assigned to receive four cycles of cisplatin plus etoposide every 3 weeks followed by accelerated hyperfractionated TR at the dose of 45 Gy in 3 weeks (sequential arm) or the same four cycles of chemotherapy administered every 4 weeks with the same modality of TR starting on day 2 of the first cycle of chemotherapy (concurrent arm). The results favored the concurrent schedule with a median survival of 27.2 months versus 19.7 months of the sequential arm, even if the difference was not significant ( p = 0.097).
Timing Question
Several phase III trials have examined the question of timing, that is, administration of early versus late RT during the course of combined chemotherapy and RT; however, the issue remains controversial. To try to clarify the issue, several meta-analyses were conducted between 2004 and 2007. The definition of early and late TR differs in these literature-based meta-analyses. The first two meta-analyses were published in 2004 by Fried et al. and Huncharek and McGarry on more than 1500 patients each. Both studies showed an advantage for early RT. In the first study, late TR was defined as beginning 9 weeks after initiation of chemotherapy or after completion of the third cycle of chemotherapy. This meta-analysis showed a statistically significant benefit of 5% of early TR over late TR in terms of 2-year OS (relative risk [RR], 1.17; p = 0.03). Moreover, both studies reported that the best results could be achieved if platinum and etoposide were administrated concomitantly with early RT. In a meta-analysis published by De Ruysscher et al., early RT was defined as beginning within 30 days after the start of chemotherapy. The 2-year and 5-year OS rates were not significantly different (odds ratio [OR], 0.84; 95% CI, 0.56–1.28 vs. OR, 80; 95% CI, 0.47–1.38). However, when the only trial that delivered concurrent nonplatinum-based chemotherapy was excluded, the results were significantly in favor of early RT, with a 5-year survival rate of 20.2% for early versus 13.8% for late RT (OR, 0.64; 95% CI, 0.44–0.92; p = 0.02). Based on the same published data of four randomized trials, De Ruysscher et al. hypothesized that the start of any treatment until the end of RT (SER) was important to consider in SCLC, taking into account both overall duration of RT and timing of TR. They concluded that a shorter time between the initiation of chemotherapy and the subsequent completion of RT was prognostic for survival. There was a significantly higher survival rate in the shorter SER arms; a 5-year OS rate of 20% was reached when the SER was less than 30 days (RR, 0.62; 95% CI, 0.49–0.80; p = 0.0003). Moreover, each additional week of the SER resulted in an overall absolute decrease in the 5-year survival rate of 1.8%. Acute toxicity, and particularly severe esophagitis, is related to timing and SER with a higher incidence in case of early RT and shorter time between start and end of therapy (OR, 0.63; 95% CI, 0.40–1.00; p = 0.05 and OR, 0.55; 95% CI, 0.42–0.73; p = 0.0001, respectively). This SER concept should certainly be further evaluated and considered in designing future studies as repopulation of cells seems to be a major cause of failure. As emphasized by Brade and Tannock in an editorial, repopulation of cells between dose fractions is important for recovery in normal tissue, but repopulation of surviving tumor cells also occurs and offsets tumor cell kill. Repopulation triggered by neoadjuvant chemotherapy may inhibit the effectiveness of subsequent RT.
The same team published an update of their literature-based meta-analysis including 11 trials; there was no difference in 2-year survival, but once again excluding the only nonplatinum-based trial, the benefit of early RT became statistically significant (OR, 0.73; 95% CI, 0.57–0.94; p < 0.05).
Another interesting observation that emerges from these studies is related to treatment compliance. Two studies with the same design and therapeutic regimen have been included in this meta-analysis: the NCI-C trial and the London trial. The survival advantage observed for the early RT group in comparison with the late one (21 months vs. 16 months; p < 0.05, respectively) reported by the NCI-C trial was not confirmed by the London trial (14 vs. 15 months, respectively). However, in the latter study, patients randomized to early chest radiation received significantly less chemotherapy than in the late arm (69% in the early group and 80% in the late one, p = 0.03). In the NCI-C study, the percentage of intended total dose completed was the same for the early and late groups (both 86%). Similar disappointing survival results have also been reported by the Hellenic trial; when analyzing compliance, a significant reduction in completion of planned chemotherapy was reported in patients who had early RT (71% in the early group and 90% in the late group, p = 0.01). Hence, it would seem that only patients who can receive early RT as planned according to the protocol benefit from it. This issue has been thoroughly addressed in an individual data-based meta-analysis that concluded that there was no difference in terms of OS between “earlier or shorter” versus “later or longer” TR when all trials were analyzed together. However, “earlier or shorter” delivery of TR with planned chemotherapy significantly improved 5-year OS at the expense of more acute toxicity, especially esophagitis. The authors highlight that the hazard ratio (HR) for OS is significantly in favor of “earlier or shorter” RT where there was a similar proportion of patients who were compliant with chemotherapy in both arms (HR, 0.79; 95% CI, 0.69–0.91) and in favor of “later or longer” RT among trials with different compliance to chemotherapy (HR, 1.19; 95% CI, 1.05–1.34; interaction test, p < 0.0001). Thereby, the absolute gain between “earlier or shorter” and “later or longer” TR in 5-year OS for similar compliance trials was 7.7% (95% CI, 2.6% to 12.8%) and was –2.2% (–5.8% to 1.4%) for different compliance trials. As expected, “earlier or shorter” TR was associated with a higher incidence of severe acute esophagitis.
Finally, a large retrospective study examined the National Cancer Database to assess practice patterns and survival for TR timing in relation to chemotherapy in 8391 nonmetastatic SCLC patients. This study suggested that early initiation of TR was associated with improved survival (5-year survival rate of 21.9%) compared with late initiation (5-year survival rate of 19.1%, p = 0.01), particularly when hyperfractionated radiation was utilized (28.2% vs. 21.2%, p = 0.004).
Sun et al. published a randomized trial of 219 patients, who were allocated to receive four cycles of cisplatin and etoposide with radiation beginning with the first cycle or the third cycle. It was not included in any of the meta-analyses. Patients received a total dose of 52.5 Gy in 25 daily fractions of 2.1 Gy over 5 weeks. Late RT was not inferior to early RT in terms of complete response rate, which was the main end point (early vs. late: 36.0% vs. 38.0%, respectively). After a median follow-up of 59 months, OS was similar in the two groups (rates at 2 years and 5 years after randomization in the early vs. late radiation arms were 50.7% vs. 56.0% and 24.3% vs. 24.0%, respectively). Thus as recommended by European and North American guidelines, patients with nonmetastatic disease, with good performance status (PS) and good compliance should be treated with concurrent chemoradiotherapy. TR should be administered early in the course of treatment, in fit patients, for whom a good compliance may be expected, preferably beginning with cycle one or two of chemotherapy. According to the study of Sun et al., TR could be administered concomitantly to the third cycle with equivalent results. Nevertheless, this observation should be confirmed in another study because one should be cautious when extrapolating results issued from Asian population studies to non-Asian patients in lung cancer. Chemotherapy should consist of four cycles of a platinum agent and etoposide.
Fractionation and Dose
Historically, modest total doses of daily fractionated radiation (1.8–2 Gy daily to 40–50 Gy) were used because of the observed responsiveness of SCLC to radiation. Although the clinical response rates with these total doses are high, durable local control is poor. The hypothesis that hyperfractionated radiation therapy might be more effective than normofractionated schedules is based on in vitro marked radiosensitivity even to small doses of radiation, and on the high kinetics of SCLC proliferation and its repopulation between two fractions of treatment. The in vitro observation of the lack of a shoulder on the cell survival curve for SCLC cell lines provides some of the rationale for the hyperfractionated schedule, in which the dose per fraction is 1.5 Gy. Two phase III trials comparing conventional RT with hyperfractionated accelerated twice-daily RT schemes have been published. In both trials, concomitant cisplatin plus etoposide chemotherapy was delivered with twice-daily RT; however, in the first trial RT was delivered after three cycles of chemotherapy, whereas in the second one RT started upfront during the first cycle of chemotherapy. In the NCCTG study, the overall treatment time was similar in the conventional and hyperfractionated arms because of a 2.5-week split at the midpoint of treatment, and this could be the cause of the lack of difference in local progression (33% in the once-daily arm vs. 35% in the twice-daily arm) and OS (20.6 months in both arms). In the Intergroup trial 0096/ECOG 3588, 417 patients were randomly assigned to receive a total of 45 Gy of concurrent TR, given either 1.5 Gy twice daily over a 3-week period or the conventional once daily over a period of 5 weeks . A significant difference in OS was reported in the last trial (19 months in the once-daily arm vs. 23 months in the twice-daily arm, p = 0.04) with a benefit in 2-year and 5-year survival rates (41% vs. 47% and 16% vs. 26%, respectively). As expected, grade III esophagitis was more frequent in the investigational arm (27% vs. 11%). An individual patient data meta-analysis on hyperfractionated and accelerated regimens in lung cancer has been conducted, which included trials comparing conventional fractionation with altered fractionation schedules in both SCLC and NSCLC. This meta-analysis showed a significant OS benefit from accelerated or hyperfractionated RT in patients with NSCLC. The effect of altered fractionation on OS was similar among patients with SCLC, but not statistically significant (HR, 0.87 [95% CI, 0.74–1.02, p = 0.08]). The absolute benefit on OS was 1.7% at 3 years (from 29.6% to 31.3%) and 5.1% at 5 years. An interesting interaction between modified regimen and PS was reported (PS 0: HR, 0.81; PS 1: HR, 0.86; PS 2: HR, 2.22), underlining once again the correlation between survival benefit derived from altered fractionation regimens and the importance of patients being fit enough to undergo a more intensive regimen.
Despite the results of the Intergroup trial, showing that the 45-Gy twice-daily regimen could improve survival, accelerated hyperfractionated RT has not been widely adopted in general clinical practice. The reasons are possibly related to the logistical difficulties of delivering twice-daily RT, the increase in acute toxicity (especially esophageal), and possibly to the fact that the control arm used rather low doses of RT. However, the most important lesson that came from INT 0096 is the demonstration that intensified RT with concomitant chemotherapy could have an impact on survival.
A recent randomized phase II Norwegian trial compared two schedules, one using twice-daily fractionation (45 Gy in 30 fractions) and the other once-daily (42 Gy in 15 fractions) so that the overall radiation treatment time was the same. Although survival favored the twice-daily regimen in this small trial, it was not statistically significant (median 25.1 months vs. 18.8 months, p = 0.61). Response rates were significantly higher with the twice-daily regimen, with no difference in severe toxicities between schedules. The way to intensify local therapy can be summarized in two strategies: total dose escalation and further exploration of altered fractionation schedules (i.e., applying concomitant boost).
Modern data on RT dose escalation come from several Cancer and Leukemia Group B (CALGB) studies starting with a phase I trial to determine the maximum tolerated dose of the twice-daily regimen and of the once-daily treatment delivered concomitantly to the fourth cycle of platinum-based chemotherapy. The total recommended dose was 45 Gy for twice-daily RT, and 70 Gy for conventional fractionation. These promising results led to several phase II trials, which all confirmed the feasibility of delivering 70 Gy with concomitant chemotherapy. The concomitant regimen (carboplatin and etoposide based) was administered after two cycles of chemotherapy with paclitaxel and topotecan. The median survival was 23 months in patients who had a weight loss over 5% compared with 31 months in patients with weight loss less than 5% before diagnosis . In a pooled analysis of limited-stage SCLC patients treated with two cycles of induction chemotherapy followed by concurrent platinum-based chemotherapy and RT, the authors analyzed 200 patients from three consecutive CALGB L-SCLC phase II trials (39808, 30002, and 30206) using high-dosage once-daily RT with concurrent chemotherapy. The median follow-up was 78 months. Grade 3 or greater esophagitis was 23%. The median survival for pooled population was 19.9 months, and the 5-year rate was 20%. The 2-year progression-free survival was 26%. The authors concluded that 2-Gy daily RT to a total dosage of 70 Gy is well tolerated, and with similar outcome to twice-daily RT administered with chemotherapy. However, this hypothesis should be confirmed in a randomized trial, which is ongoing (NCT00433563).
The second method for intensifying local treatment was applied by Radiation Therapy Oncology Group (RTOG) researchers conducting some clinical studies with a hybrid approach, consisting of once-daily RT at standard fractionation in the first part of treatment followed by twice-daily RT to counter repopulation. The RTOG applied this dose escalation method from a total dose of 50.4 Gy to 64.8 Gy. The esophagitis rate was lower than in the INT 0096 trial (18% in comparison with 27%), and so were the median and 2-year survival rates (19 months and 36.6% in comparison with 23 months and 47%, respectively).
To establish the optimal dose and fractionation, two phase III trials have been undertaken comparing two modalities of concurrent chemoradiation: hyperfractionated accelerated RT (45 Gy in 3 weeks as given in the INT 0096 study) and once-daily RT at higher dosage (66–70 Gy in 6.5 weeks) corresponding to a higher biologic effective dose but with superior overall treatment time.
The Intergroup trial CALGB 30610/RTOG 0538 (NCT00632853) started as a three-arm study. It was decided that the experimental arm with the higher rate of toxic events would be discontinued. Arm B was then closed in 2013. This trial is continuing as a two-arm study comparing arm A (twice-daily RT of 45 Gy) with arm C (once-daily RT of 70 Gy).
- •
Arm A: twice-daily RT up to a total dose of 45 Gy delivered concurrently to the first cycles of four cisplatin and etoposide chemotherapy regimens;
- •
Arm B: hybrid approach applied concurrently to the same chemotherapy regimen (this arm has been discontinued after a preplanned interim analysis);
- •
Arm C: once-daily RT at standard fractionation up to a total dose of 70 Gy with the same chemotherapy regimen.
The second phase III trial is the CONVERT intergroup study (concurrent once-daily vs. twice-daily RT; NCT00433563), which is a United Kingdom–led study comparing twice-daily and once-daily RT. The results of the CONVERT study were presented at the American Society of Clinical Oncology Annual Meeting, in 2016. The study enrolled 547 patients with proven SCLC from 73 centers in seven European countries and Canada between 2008 and 2013. Patients were randomized to receive either concurrent twice-daily radiation therapy (45 Gy in 30 twice-daily fractions over 3 weeks) or concurrent once-daily radiation therapy (66 Gy in 33 once-daily fractions over 6.5 weeks), both starting with the second cycle of chemotherapy on day 22. Four or six cycles of cisplatin–etoposide were given according to the investigator’s prespecified choice. Patients with any response were offered prophylactic cranial radiation. At a median follow-up of 45 months, 2-year and 3-year survival rates and median survival were 56%, 43%, and 30 months, respectively, for the twice-daily radiation therapy versus 51%, 39%, and 25 months for the once-daily radiation therapy (HR, 1.17; 95% CI, 0.95–1.45; p = 0.15). Toxicities were comparable; grade 3/4 esophagitis rate was 19% in the twice-daily arm and 18% in the once-daily arm. The results of CONVERT support the use of either regimen for standard-of-care treatment of nonmetastatic SCLC with good PS. The authors insisted that survival in both arms was higher than previously reported probably because of better patient selection.
To summarize, the evidence strongly supports concurrent chemotherapy and RT for patients with LS-SCLC. The available data also suggest that RT should begin early in good performance patients; the RT fractionation programs that satisfy these parameters have been associated with better survival.
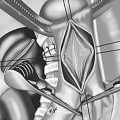
Radiation Treatment Volumes
The two major issues regarding treatment volume in SCLC can be summarized as follows:
- •
Is it appropriate to use the postchemotherapy target volume after induction chemotherapy in cases where RT is delayed?
- •
Do we need to electively treat clinically uninvolved regional lymph nodes?
An evolution in target volume definition can be recognized over the last two decades. In the early 1990s, emerging evidence demonstrated that smaller radiation target volumes did not adversely affect tumor control in the management of LD-SCLC. In fact, more than 80% of failures occurred in-field, suggesting that inadequate radiation doses rather than inadequate volumes were the primary cause of intrathoracic recurrence. Therefore the prevailing issue of recent research has been to reduce the treatment field size while increasing the radiation dose and sparing surrounding organs at risk. The analysis of the site of recurrence after chemoradiation may help define the optimal treatment volume. In the randomized study by Kies et al. published in 1987, patients achieving a partial response or stable disease after induction chemotherapy were randomized to receive RT either to the prechemotherapy volume or to the postinduction reduced tumor volume. The local recurrence rate was not significantly different in the two arms (32% vs. 28%). Liengswangwong et al. and Arriagada et al. came to the same conclusions in their studies. Consequently, treating the residual tumor after induction chemotherapy may be sufficient. However, it should be underlined that most patients treated in these older studies had no chemotherapy-based treatment planning. More recent trials have explored the role of involved-field RT. In 2008, a report from the International Atomic Energy Agency explored whether one should electively treat all mediastinal nodes, or selectively include those with some clinical risk for harboring disease, or perhaps omit elective nodal irradiation (ENI) altogether. This review revealed how limited the evidence was for defining the place of ENI in SCLC at that time. The authors suggested the need for prospective clinical trials and recommended that, given the lack of strong evidence regarding ENI in LD-SCLC, the use of ENI should be considered on a case-by-case basis.
More recently, prospective clinical trials have explored this issue and have reported on isolated mediastinal relapse, defined as failure in an initially uninvolved lymph node region in the absence of local recurrence or distant metastasis. A small prospective study (37 patients) from the Netherlands Cancer Institute reported only two out-of-field isolated nodal failures (5.3%) with an excellent 5-year survival of 27% using involved-field RT as part of combined modality treatment. In another small study from the United Kingdom (38 patients), where patients were treated omitting ENI based on CT imaging, no isolated nodal failure was reported. Eight patients were found to have an intrathoracic recurrence: two within the planning target volume only, four within the planning target volume and distantly. There were only two cases of thoracic nodal relapse (6.5%), and both were accompanied by distant metastases. The Maastricht group outlined the possible importance of PET–CT in defining treatment volumes in SCLC. In the first prospective study, with the gross tumor and nodal volume being defined by CT imaging, they reported an isolated nodal failure in 3 of 27 patients (11%), all in the supraclavicular region. Thus the omission of ENI on the basis of CT scan resulted in a higher-than-expected rate of isolated nodal failure in the ipsilateral supraclavicular fossa. However, the authors stated that because of the small sample size, no definitive conclusion could be drawn, and recommended to continue use of ENI outside of clinical trials. However, they started a small prospective trial evaluating selective nodal irradiation based on F-2-deoxy- d -glucose (FDG)-PET for LD-SCLC. Of the 60 patients enrolled, 39 (65%) developed a recurrence, but only two patients (3%) experienced isolated nodal failure. These findings are in contrast with the previous experience of CT-based selective nodal irradiation.
In 2012, Xia et al. examined the pattern of failures in 108 patients included in two successive trials and treated with combined involved-field RT and chemotherapy. They reported an isolated nodal failure rate in 5 patients (4.6%) treated with involved-field RT and chemotherapy using CT imaging for target definition, all in the ipsilateral supraclavicular area. Moreover, another four supraclavicular nodal failures with simultaneous distant metastases were also observed. To try to clarify the role of prophylactic irradiation of the supraclavicular area, a retrospective analysis on 239 patients has been conducted by Feng et al. The supraclavicular metastasis incidence was 34.7%; multivariate analysis showed that upper mediastinal involvement (level 2 or 3) was significantly associated with supraclavicular metastasis. Thus such patients with upper mediastinal involvement could theoretically benefit from prophylactic irradiation of the supraclavicular lymph nodes. The lesions located in the right upper lobe had a higher incidence of supraclavicular involvement. In patients with supraclavicular involvement, 36% had bilateral or contralateral lymph node metastases and the frequency of contralateral involvement was higher for left-sided tumors than for those on the right.
The available data suggest that FDG-PET scans are more accurate than CT in the primary staging of SCLC and subsequently may lead to a reduction in the rate of isolated nodal failure. A systematic review suggests that compared with conventional staging, PET can alter management in at least 28% of SCLC patients, resulting in the addition of life-prolonging RT in 6% and averting unnecessary RT with associated toxicity in 9%. The cost analysis revealed that the PET-based strategy and the conventional methods do not seem significantly different, but PET may reduce health-care costs through avoidance of inappropriate TR. A planning study on FDG-PET–based selective mediastinal node irradiation in 21 LD-SCLC patients showed a change in the PET treatment plan compared with the CT-based plan in 24% of cases.
In a retrospective study by Shirvani et al. examining the role of FDG-PET–based treatment planning before intensity-modulated RT combined with chemotherapy in 60 patients with SCLC and omitting ENI, a low rate of isolated nodal failure was found (2%). The authors concluded that ENI could be safely omitted in patients who underwent staging with PET–CT and treatment with intensity-modulated RT. Recently, a continuation of the work by Van Loon et al. has been published by Reymen and colleagues, expanding the initial series of 59 patients to 119 patients treated with concomitant chemotherapy and accelerated hyperfractionated RT, with only CT-PET–positive or pathologically proven nodal sites being included in the target volume. Isolated elective nodal failure occurred only in two patients (1.7%) as in other studies using PET–CT for treatment planning. Median follow-up was 38 months, median OS was 20 months (95% CI, 17.8–22.1 months), and 2-year survival was 38.4%. In multivariate analysis, only total gross tumor volume (corresponding to postchemotherapy tumor volume and prechemotherapy nodal volume) and PS significantly influenced survival ( p = 0.026 and p = 0.016, respectively).
A comparison of treatment outcomes between involved field and ENI in LS-SCLC was conducted retrospectively in a Korean study of 80 patients. The two groups had similar overall and progression-free survival; however, for patients who had no PET scan, survival was significantly longer in patients who had ENI. All the isolated nodal recurrences were observed in patients who had no PET scan in their initial workup.
In a retrospective study of 253 patients treated in one institution over more than 10 years, the authors focused on locoregional failures. The cumulative locoregional failure rate was 29% and 38% at 2 years and 5 years, respectively. About 30% of local and regional failures were in-field, so most failures were marginal or out-of-field. Thus, according to these authors, it may be possible to prevent locoregional failure with improved RT target definition and careful consideration of the initial extent of disease.
In conclusion, if patients do not have PET staging, the extension of the initial disease should be carefully evaluated to reduce the risk of isolated nodal failure and impaired survival outcome, and elective irradiation of the supraclavicular region should be considered. Subsequently, involved-field irradiation for limited stage SCLC can be considered with pretreatment PET–CT scan implementation. The two phase III trials investigating once-daily versus twice-daily RT will hopefully contribute to clarify volume issues. They do not recommend ENI, but require that both FDG-PET–avid lymph nodes and enlarged regional lymph nodes by CT criteria (regardless of FDG-PET activity) are included in the radiation treatment volume.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree