Radiologic Imaging Concerns
Jeffrey A. Bennett
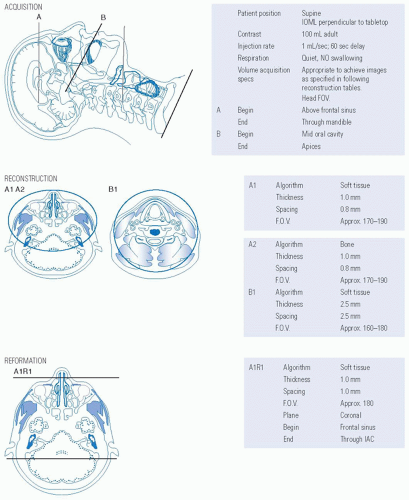
Imaging is critical in cases of cancer of the nasal cavity and paranasal sinuses, and computed tomography (CT) and magnetic resonance imaging (MRI) are complementary in evaluating lesions extending to the skull base and the orbit.1,2 Both modalities are good at differentiating benign mucosal disease from more aggressive disease.3 CT is typically performed first because of its speed and superior ability to show bony detail and destruction. CT must be performed with very thin sections, down to 0.5 mm, and reconstructed in bone and soft tissue algorithms. It is no longer necessary to acquire direct coronal CT images because the speed of imaging limits motion artifact, and very good quality coronal and sagittal reformations can be obtained from the very thin axial data. Both CT and MRI should be performed with contrast when a mass is suspected or known.4 A combination of CT to evaluate bone and MRI to evaluate tumor versus obstructed mucosal disease has been shown to be essential.5,6 Suggested protocols are given in Figures 21-13 and 21-14. The value of FDG PET-CT in the initial workup of sinonasal tumors is still being debated. These studies have a high negative predictive value, which is very useful for evaluation of tumor recurrence. However, the high rate of false-positive studies require the results to be viewed with caution.7
The approach to interpreting the images, as in other regions of the head and neck, is to determine the full extent of the primary tumor and to determine the presence of perineural and lymphatic spread.
In the nasal cavity and paranasal sinuses, a description of the local extent of a tumor includes a discussion of the amount of bone destruction present in the nasal cavity, facial bones, and sinuses and whether some of the abnormalities seen are a result of obstructed mucosal drainage, such as mucocele formation (Fig. 21-15) rather than tumor. Occasionally, imaging features will suggest a certain histology, such as lymphoma when the tumor is low signal on T2-weighted images and restricts on diffusion-weighted sequences, but usually determination of histology is reserved for the biopsy results. Both MRI and contrastenhanced CT can demonstrate features of hypervascular tumors, showing large flow voids on MR and large vascular pedicles on
CT angiography. These findings can warn the surgeon to expect bleeding during biopsy or resection.
CT angiography. These findings can warn the surgeon to expect bleeding during biopsy or resection.
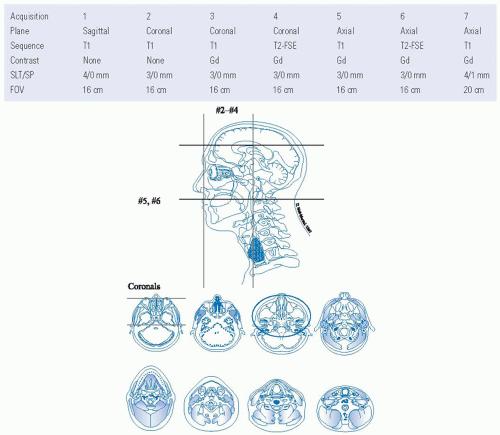 FIGURE 21-14. Protocol for MRI of the sinonasal region with intravenous contrast. Source: Reprinted from Mancuso AA, Hanafee WN. Head and Neck Radiology. Philadelphia, PA: Lippincott Williams & Wilkins; 2011:2243, with permission.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|