Radiologic Imaging Concerns
Jeffrey A. Bennett
MRI is generally preferred over CT for the imaging of salivary gland neoplasms. This is because of its ability to better characterize the internal morphology of the tumor, its boundaries, and to determine perineural spread. For example, benign mixed tumors often appear very bright on T2-weighted images with variable enhancement (Fig. 25-15). However, imaging cannot confidently predict whether the lesion is benign or malignant.1 Features that suggest a benign mass are sharp margins of the lesion and no lymphadenopathy or signs of perineural spread. A malignant lesion is suggested by indistinct margins, enhancement, and edema of the facial nerve suggesting perineural invasion, and lymphadenopathy (Fig. 25-16). Nevertheless, many benign and malignant salivary gland tumors will appear to be well circumscribed both on CT and MRI.2 Suggested protocols are given in Figures 25-17 and 25-18.
Imaging is often performed to plan an approach for biopsy, as therapy is different depending on whether the mass is a primary salivary gland tumor, or lymphoma, or other metastasis such as squamous cell cancer from a skin primary site. Fine-needle aspiration has proven to have reliable sensitivity and specificity for salivary gland neoplasms.3 Ultrasound guidance is usually excellent for more superficial parotid and submandibular gland lesions. CT is often better for biopsy of lesions in the deep lobe of the parotid, as a transfacial approach (Fig. 25-19) can often be used to avoid crossing the facial nerve. In most cases, a core biopsy can be safely obtained when FNA is not diagnostic and is often helpful in the workup of lymphomas or sarcomas. Core-needle biopsies can be obtained either with ultrasound guidance or CT guidance.4
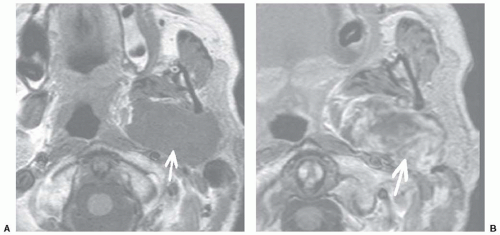
MRI is particularly useful for evaluating the presence of perineural spread. This is very common in certain types of neoplasm such as adenoid cystic carcinoma. Intravenous contrast is essential for making this diagnosis, and the use of fat suppression often makes perineural spread more apparent. The axial plane is excellent for demonstrating perineural spread of cancer along the auriculotemporal nerve, which is a connection between the facial nerve and mandibular nerve (Fig. 25-20). The coronal plane is better for demonstrating tumor spread along the descending facial nerve canal (Fig. 25-21).
In the recent past, surface coils were very useful to obtain high-resolution MR images of the superficial parotid gland. The prevalence of multichannel head coils and 3T magnets has made surface coils unnecessary.
It has been found that dynamic contrast-enhanced MRI may be useful in the identification of Warthin tumor as this tumor demonstrates rapid enhancement and rapid attenuation.5 Presumably, this enhancement pattern could be detected with dynamic contrast-enhanced CT as well. Other investigators have found the detection of low-signal areas in a parotid tumor on short tau inversion recovery and T2-weighted sequences, as well as low apparent diffusion coefficient values on diffusion-weighted imaging suggested Warthin tumor.6,7
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree