Radiation Therapy Technique
William M. Mendenhall
PYRIFORM SINUS
Parallel-opposed portals are used to treat the primary cancer and both sides of the neck to include lymph nodes in levels II, III, IV, V, and the retropharyngeal nodes at the level of the C1-C2 vertebral bodies. It is difficult to detect subclinical disease at the pyriform sinus apex, which is located somewhere between the top and the bottom of the cricoid cartilage, even at direct laryngoscopy. Therefore, the inferior border of the initial portals is located 2 cm below the bottom of the cricoid cartilage. It may be difficult to obtain this margin if the patient has large shoulders and a low-lying larynx. If this is the case, the lateral portals are angled approximately 10 degrees inferiorly and the anterior portal used to treat the low neck is eliminated. The anterior field border may be placed just behind the skin of the anterior neck to avoid tangentially irradiating this area for patients with T1-T2 cancers and early-stage neck disease. The superior border is placed at, or just below, the jugular foramen, and the posterior border is placed just posterior to the spinous processes of the vertebral bodies (Fig. 19-27).1 Reduction off the spinal cord is performed at approximately 45 Gy, and a second mucosal reduction occurs at 60 Gy. Electron beam is used to treat the posterior strips, if necessary, after reduction off the spinal cord.
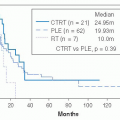
Intensity-modulated radiation therapy (IMRT) may be employed to treat patients with a clinically negative neck or ipsilateral positive nodes to reduce the dose to the contralateral parotid to 26 Gy or less and to avoid a difficult match between the conventional lateral fields and the anterior low neck portal in the patient with a low-lying larynx and a short neck. Patients may be treated once daily or with an altered fractionation schedule.2 The concomitant boost technique is employed at our institution and consists of 72 Gy in 42 fractions over 30 treatment days to gross disease (Fig. 19-28). Subclinical disease receives 49.5 to 54 Gy.3 Alternatively, patients are treated to 74.4 Gy in 62 twice-daily fractions over 31 treatment days. Patients with a clinically negative neck receive elective RT to bilateral levels II, III, IV, V, and the retropharyngeal nodes.4 Patients with ipsilateral positive nodes receive RT to ipsilateral levels IB, II, III, IV, V, VI, and the retropharyngeal nodes, as well as contralateral levels II, III, IV, VI, and the retropharyngeal nodes. Patients with stages III to IV cancers receive concomitant weekly cisplatin 30 mg/m2. Those with positive nodes undergo a computed tomographic scan 1 month after RT to determine whether a neck dissection is indicated.5
The radiation therapy treatment technique after surgery that entails partial laryngectomy is as described above. The technique employed after a total laryngectomy is the same as that described in the “advanced larynx” chapter.
PHARYNGEAL WALL
Because squamous cell carcinomas of the pharyngeal wall tend to spread submucosally, wide margins for the primary cancer are initially utilized. The portals are parallel opposed and usually weighted 1:1. The field margins for the initial fields usually extend to the bottom of the cricoid cartilage, 0.5 to 1.0 cm behind the skin of the anterior neck, the posterior processes of the vertebral bodies, and to (or just below) the jugular foramen. Because large tumors tend to extend posterolaterally around the vertebral bodies, the posterior border of the off-cord reductions is placed at the anterior edge of the spinal cord (Fig. 19-29).6 The low neck is treated with an anterior field with a thin, tapered midline tracheal block. Electrons are used to treat the posterior strips after reduction off the spinal cord, if necessary.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree