Radiation Therapy Technique
William M. Mendenhall
T1N0-T2N0 GLOTTIC LARYNX
The portals used to treat T1N0 and T2N0 glottic carcinomas are limited to the primary lesion. The risk of occult disease in the neck nodes is very low, even for patients with T2B tumors, and elective neck irradiation is not indicated.
Patients may either be treated in the lateral decubitus position with the fields set up daily by the physician using the anatomic landmarks or in the supine position with aquaplast to ensure accurate repositioning. Parallel-opposed fields are used and weighted 3:2 toward the side of the cancer, if it is lateralized. Weighting the fields reduces the dose to the contralateral posterior larynx. The field borders for a T1N0 cancer involving the anterior two-thirds of the cord are the middle of the thyroid notch, the bottom of the cricoid cartilage, 1 cm posterior to the thyroid lamina, and 1.5 cm fall off anteriorly (Fig. 18-22).1 The fields are enlarged for T2 cancers depending on the sites of disease extension. Approximately 5% of the dose may be delivered with an anterior field centered over the tumor, with the patient in the supine position, in order to reduce the dose laterally. Patients are treated with 60Co, 4 MV x-rays, or 6 MV x-rays; the dose delivered to the tumor is similar for these beams.2 Alternatively, patients may be treated with intensity-modulated radiation therapy (IMRT) to reduce the dose to the carotid arteries and reduce the long-term risk of stroke.3 Patients with cancers that extend anteriorly though the cricothyroid membrane into the soft tissues of the neck may be underdosed with 6 MV x-rays. However, these lesions are T4 by definition, and the treatment techniques are addressed elsewhere.
Patients with T1 or T2 vocal cord cancer treated with once-aday fractionation at the University of Florida are irradiated with 2.25 Gy fractions to 63 Gy for T1 and T2A cancers and 65.25 Gy for T2B lesions.
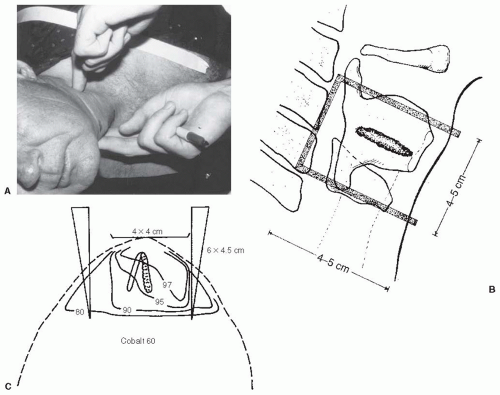 FIGURE 18-22. Radiation treatment technique for carcinoma of glottic larynx, stage T1-2. A: Patient is in lateral decubitus position. To locate the posterior border of the thyroid cartilage, fingers of one hand are positioned under the patient’s neck and the larynx is lifted gently a few millimeters while the index finger of the other hand simultaneously locates the posterior edge of the thyroid lamina. B: For T1 cancer, the superior border of the field is usually at mid thyroid notch (height of the notch typically is approximately 1.0 cm or slightly more in male adults); for minimal lesions (e.g., carcinoma in situ), the bottom of the thyroid notch is chosen. If the ventricle or false vocal cords are minimally involved, the top of the notch (which corresponds to the cephalad portion of the thyroid lamina as palpated just off midline) is often selected; more advanced lesions call for greater superior coverage. If only the anterior half of the vocal cord is involved, the posterior border is placed at the back of the mid portion of the thyroid lamina. If the posterior portion of the cord is involved, the border is 1.0 cm behind the lamina. If the anterior face of the arytenoid is also involved, the posterior border is placed 1.5 cm behind the cartilage. If no subglottic extension is detected, the inferior border of the irradiation portal is at the bottom of the cricoid arch as palpated at the midline. If computed tomography demonstrates subglottic extension, the portal is adjusted accordingly. Anteriorly, beam fall off (by 1.5 cm) over patient’s skin. C: The three-field technique (two lateral wedge fields and an anterior open field) is commonly used to treat vocal cord cancer at the University of Florida. Lateral fields are differentially weighted to involved side. The anterior field, which usually measures 4 × 4 cm, is centered approximately 0.5 cm lateral to midline in patients with one cord involved and typically delivers approximately 5% of total tumor dose (usually on last 2 treatment days) after treatment from the lateral portals is completed. The anterior portal is essentially a reduced portal that centers high dose to the tumor. The isodose line at which the dose is specified is that which covers gross disease. By appropriate field weightings, encompassing the tumor within 95% to 97% of maximum isodose line is virtually always possible. Source: Parts A and C from Parsons JT, Palta JR, Mendenhall WM, et al. Head and neck cancer. In: Levitt SH, Khan FM, Potish RA, et al., eds. Levitt and Tapley’s Technological Basis of Radiation Therapy: Practical Clinical Applications. 3rd ed. Baltimore, MD: Lippincott Williams & Wilkins; 1999:269-299 (Fig. 16.1A and C, p. 270); Part B from Million RR, Cassisi NJ, Mancuso AA, et al. In: Million RR, Cassisi NJ, eds. Management of Head and Neck Cancer: A Multidisciplinary Approach. 2nd ed. Philadelphia, PA: JB Lippincott; 1994:431-497 (Fig. 18-21, p 464.), with permission. |
T1-T2N0 SUPRAGLOTTIC LARYNX
The risk of occult disease in the neck nodes is relatively high, even for early-stage lesions, so that the nodes at risk are treated bilaterally in conjunction with the primary malignancy. For patients with a clinically negative neck, the nodes at highest risk are those in levels II, III, and IV. Nodes in levels I, V, and VI, and the retropharyngeal lymph nodes are unlikely to harbor metastatic disease, and the fields are not enlarged to include these areas.
Patients are treated with parallel-opposed fields weighted to the side of the cancer, if it is lateralized. The fields usually extend from the bottom of the cricoid cartilage to 1 to 2 cm above the angle of the mandible, to the posterior of the spinous processes, and fall off 1.5 cm anteriorly, if the cancer extends to the anterior commissure and/or petiole. If not, a strip of anterior skin may be spared (Fig. 18-23).4 The low internal jugular lymph nodes are included in a tight low neck field with a small, tapered, midline block (see Fig. 18-23).4 The fields are reduced off the spinal cord at approximately 45 Gy, and a second mucosal reduction is performed at 60 Gy to encompass the initial gross disease, with a 1.5- to 2.0-cm margin.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree