External
External radiotherapy has several advantages as the radiation modality of choice for carcinoma of the penis. It is widely available, delivers a reliably homogeneous dose, and does not require the specific expertise of brachytherapy. Well-localized CIS (Tis) may be treated effectively to a depth of less than full thickness of the penile shaft using 125 to 250 kV orthovoltage beams, or 13 MeV electrons (
14), using fractionation schemes commonly employed for skin cancer such as 35 to 40 Gy in 10 fractions over 2 weeks. However, most penile cancers, because of uncertainty of the depth of invasion, require irradiation to the full thickness of the penis with full dose to the skin surface. Various techniques have been devised for this purpose. Fraction sizes <2 Gy (
4) may be associated with higher recurrence rates, whereas fraction sizes >2 Gy (
15) may be associated with greater long-term sequelae such as urethral strictures. The most commonly prescribed dose is 60 Gy in 30 fractions over 6 weeks. Treatment interruptions because of acute reactions (edema, pain, desquamation) should be avoided (
4). Circumcision is required before definitive radiotherapy to prevent acute radiation balanitis and long-term phimosis. A setup that is easily reproducible over a 6-week period, comfortable for the patient despite increasing local reaction, and easily verified by technologists is desirable.
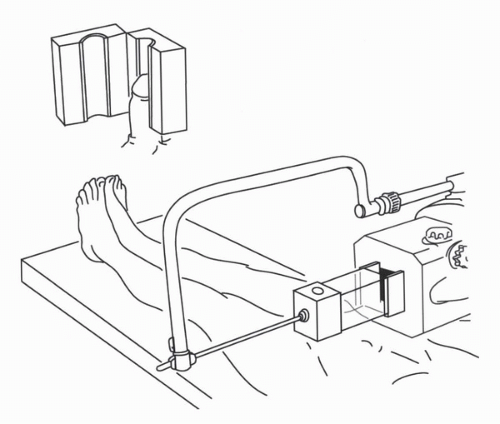
Wax Block
A 10 × 10 cm to 10 × 15 cm wax block is used to encompass the penis for each treatment (
16). The block is constructed in two halves, with a central cylindrical chamber fashioned internally. The patient is positioned supine on the treatment couch, and the penis is supported in a vertical position, encased in the wax block. A tissue-equivalent “cork” must be placed in the opening. Parallel opposed beams treat the entire length of the penis. External beam radiation (EBRT) using
60Co, or 4 to 6 MV photons can be used (
Fig. 48.1). Daily setup may become increasingly uncomfortable as treatment progresses and penile swelling may require modification of the wax block to enlarge the central chamber. Furthermore, it is not possible to verify penile position within the wax and if the fit is not snug, the penis may “slump” inside the wax, resulting in treatment of a shorter length of the shaft than planned.
Molds
Neave et al. (
15) have reported experience with iridium molds for Jackson stage 1 or 2 (
19) (
Table 48.1) penile carcinoma. A hollow cylindrical Perspex tube is fitted over the penis along its long axis and is held in place by a girdle fitting around the patient’s groin and upper thighs. Iridium-192 wire is arranged circumferentially in concentric rings in a second outer sourcecarrying tube, which is positioned daily for periods of approximately 12 hours. Hospitalization is required, and the patient must be cooperative. One advantage of a mold over EBRT is that the acute reaction develops after the treatment is finished. Unlike interstitial brachytherapy, a mold is not invasive and does not require anesthesia. A surface dose of 55 to 60 Gy (
16) is prescribed, with a central axis dose of 46 to 50 Gy. The total treatment duration is approximately 1 week.
Akamoto et al. (
20) have reported a custom mold technique using silicon monomer. The penis is suspended using traction on a catheter to hold it centrally in a plastic cylinder. Silicon monomer mixed with a catalyst is poured into the cylinder, around the penis, and hardens into a sponge-like material within 10 minutes. The material can be removed easily after it has set, and hollow catheters are inserted longitudinally for after-loading sources. The authors describe using a variety of sources, including 226Ra, 137Cs, and 192Ir. Patients were treated with one to three fractions. Fraction size ranged from 10.7 to 40 Gy (median 20 Gy), with total dosages ranging from 32 to 74 Gy.
Interstitial Brachytherapy
There is a wide experience with interstitial brachytherapy for T1 and T2 penile carcinoma, with reports from many
European countries, from Canada, and from India. Implants are generally performed under general anesthesia, but local or spinal anesthesia is also an option. The Paris system of dosimetry (
21) is most commonly employed and is applicable to both manually after-loaded implants and remote after-loading pulse dose rate (PDR), although for the latter, some optimization can be introduced.
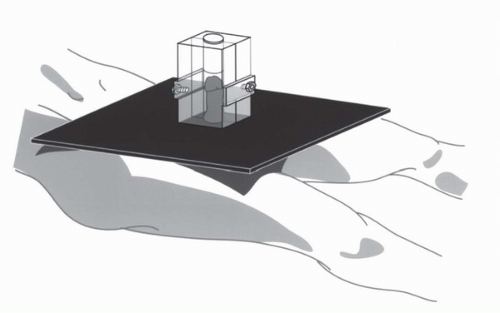
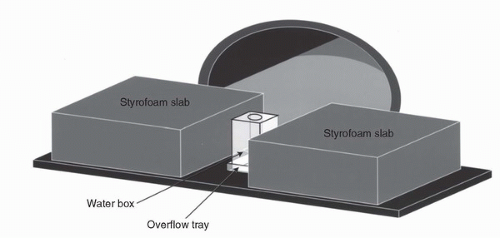
Penile brachytherapy is generally performed as a volume implant delivering treatment to the full thickness of the glans, although well-selected, very superficial tumors, or Tis disease, may be treated with a single-plane implant. For volume implants, two or three parallel planes of sources are inserted, with intersource and interplane spacing being equal and ranging from 12 to 18 mm.The distribution, spacing, and total number of needles depend on tumor size. Four (2 × 2), six (2 × 3), or nine (3 × 3) needles may be required. Planes are usually oriented with the needles passing from the dorsal to the ventral surface of the glans, but a left-right orientation may be acceptable depending on tumor location. Needle placement requires 30 to 45 minutes in the operating room. Catheterization of the patient during the procedure aids in identification of the urethra so as to avoid transfixing it with implant needles. 19.5-gauge needles are used in association with manually after-loaded 192Ir wire, and 17-gauge needles are compatible with a PDR remote after-loader. The needles are held in place through the duration of the implant with predrilled plexiglass templates. The prescribed dose is generally 60 Gy over 4 to 5 days at a classic low dose rate (LDR) of 50 to 60 cGy/hr (<1 Gy/hr). No dose rate correction is required for PDR as compared with continuous LDR. On the contrary, high dose rate brachytherapy (HDR) requires compensation in total dose because of the elevated dose rate and smaller number of fractions. Suggested fractionation schemes for HDR brachytherapy for penile cancer have not been published.
At the completion of the procedure, a Styrofoam collar is positioned around the base of the penis proximal to the needles to support the penis in the upright position and to thereby minimize unnecessary irradiation of the adjacent abdominal wall, thigh, or scrotal skin. If preservation of fertility is a concern, a thin sheet of lead can be inserted into the Styrofoam collar to minimize transmitted dosage to the testicles. Thermoluminescent dosimeters measurements for PDR penile brachytherapy after incorporation of a layer of 2 mm of lead into the Styrofoam collar around the penis indicate a total dose of 53 to 58 cGy to the anterior testicle and of 26 cGy to the posterior testicle (Crook, personal experience).
The brachytherapy needles are remarkably well tolerated. The patient remains catheterized and in bed for the duration of the implant, although with PDR the source cables can be disconnected from the needles to allow the patient to mobilize for a brief period between fractions if desired. Sufficient analgesia is usually provided by acetaminophen, with or without codeine. Leg exercises and subcutaneous heparin (5,000 U q12h) are recommended as prophylaxis against deep vein thrombosis. Removal of the needles occurs at the bedside following premedication with a narcotic analgesic.
Interstitial brachytherapy has the advantage of being completed within 4 to 5 days, with the peak acute reaction occurring 2 to 3 weeks after treatment has finished. Interstitial brachytherapy minimizes unnecessary treatment to the penile shaft, and because the lesion is clearly visible as the needles are being placed, visual verification of coverage can be readily accomplished. Needle placement should be such that the prescription isodose should allow for about 10 mm of coverage beyond visible or palpable tumor. Care must be taken to adhere to the rules of the Paris system (
21) and to be aware of the relation of the treated volume to the needles such that the entire tumor and desired margin are contained within the highdose volume (
Fig. 48.4). The technical aspects of implanting meatal or unilateral tumors have been described (
22).