3 Principles of radiotherapy
Introduction
After surgery, radiotherapy is the most effective curative treatment for cancer, contributing up to 25–30% of cure. At least half of the patients with cancer require radiotherapy at some time in their illness of which about 60% are treated with curative intent, often in combination with surgery and chemotherapy. Radiotherapy involves use of various types of ionizing radiation, and X-ray is the commonest type of radiation used. Other forms of radiation include electrons, protons, neutrons and gamma radiations from radioactive isotopes. This chapter intends to review the principles of practical radiotherapy (Box 3.1) and a detailed discussion on radiobiology and mathematical modelling are beyond the scope of this chapter.
Methods of delivery of radiotherapy
External beam radiotherapy (EBRT)
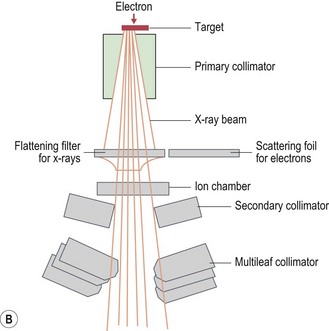
Modern radiotherapy is based on megavoltage X-rays (photons) and electrons. Megavoltage X-rays are produced by artificial acceleration of electrons through a vacuum to impact on a target in machines called linear accelerators (LINACs) (Box 3.2). The energy of the X-rays is proportional to the speed of electrons. Electrons are produced when the target in a linear accelerator is removed from the path of the electron beam (Box 3.2). Modern LINACs have facilities to produce both photons and electrons. Electrons have a predictable penetrability and hence are useful when it is important to limit the radiation dose to a deeper organ. Characteristics of photons that are useful in their clinical use are:
Box 3.3
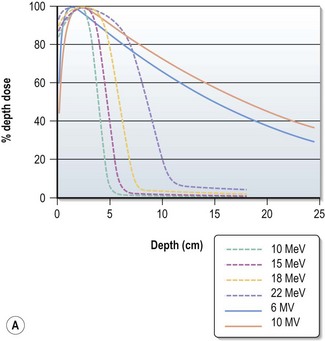
Choosing the energy (Figure 3.2)
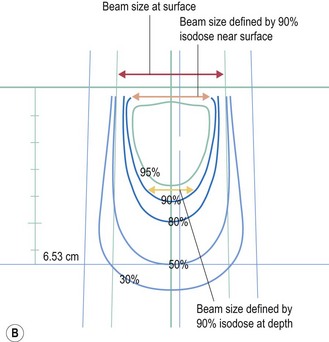
Electrons have a definite range (range in centimeters is approximately half of beam energy in MeV) and selection of electron is based on the depth needed to treat (effective treatment depth in centimeters, as defined by 90% isodose in centre, is approximately one-third of the beam energy in MeV ). With increasing energy, the surface dose decreases and hence if higher dose is needed at the surface, a bolus is used (p. 23). Bolus is also used to bring up high dose region to surface to avoid radiation to underlying critical structure. Higher energy electron beams exhibit a lateral constriction of 90% isodose line (Figure 3.2B) which need to be taken into consideration while deciding the field size at surface.
Brachytherapy
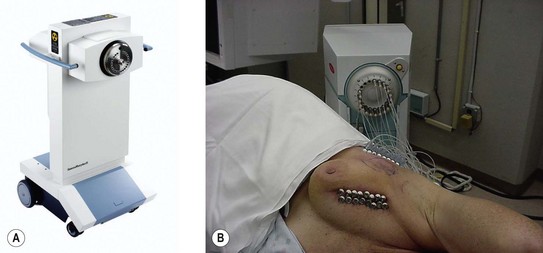
The previous problems of radiation safety for patients and staff, and prolonged treatment time, have become history with modern brachytherapy machines (Figure 3.3). Clinical applications of brachytherapy are as follows:
Radionuclide treatment
Systemic administration of radionuclides, which emit gamma-radiation, is a useful treatment for cancer. In well differentiated thyroid cancer, 131I is given to patients after thyroidectomy (p. 282). Strontium-89 and samarium-153 are used for palliation of bone metastases, particularly from prostate cancer.
Informed consent
Once a decision is made to treat with radiotherapy, this decision should be communicated to the patient. The patient should be informed of the intention of treatment, potential benefits and side effects, both short term and long term. It is also an obligation to explain to the patient the potentially serious short and long term consequences of treatment in order to obtain truly informed consent. Often patients would like to know details of how radiation works (Box 3.4), dose and length of treatment, rationale for a number of treatments (fractionation – the process of giving the total dose of radiation as small doses over a period of time) (Box 3.5) and side effects (p. 348). Side effects of radiotherapy depend on the area of treatment, total dose and dose per fraction. These can be acute (occurring during radiotherapy and within 3 months of completion of radiotherapy) or chronic (occurring 3 months after completion of radiotherapy).
Box 3.4
How does radiation work?
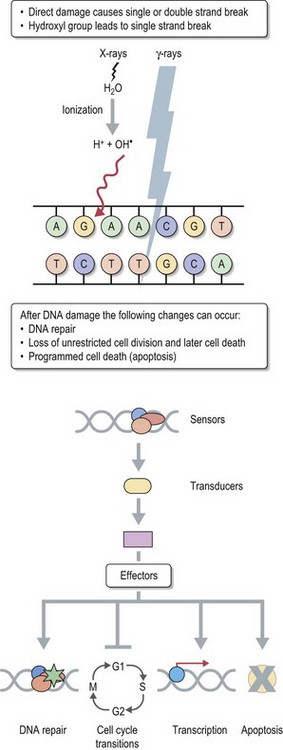
Therapeutic use of radiotherapy is born out of empiricism. Science caught up with empirical clinical use later to provide explanations for various patterns of response to treatment. The cancer cell has an unlimited capacity to multiply and radiotherapy is aimed to prevent this unlimited multiplication. The conventional explanation of radiation effect is based on radiation damage to DNA caused directly by photons and indirectly by free radicals which are produced when photons interact with water molecules in the tissue (see Figure 3.4). There are three different types of radiation damage to DNA:
Box 3.5
Rationale for fractionation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree