7 Palliative care
Pain management
Assessment of pain
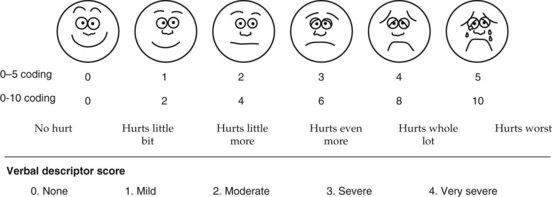
It is important to assess the multidimensional nature of pain. Intensity of pain, location, duration and factors that modify pain should be assessed. There are various tools to assess the pain and the commonly used ones are shown in Box 7.1.
Management of pain
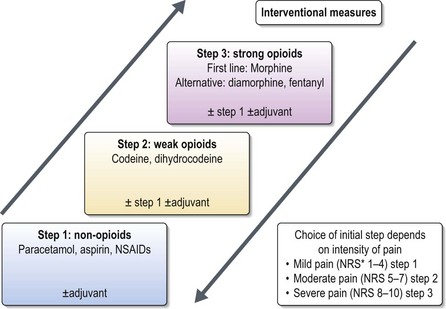
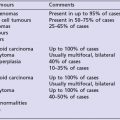
The management of pain includes analgesics as well as non-pharmacological measures. The World Health Organization (WHO) analgesic ladder (Figure 7.1) has been the gold standard in the management of pain and has been shown to eliminate pain in 80% of patients. The remaining 20% have complex pain which may require specialist interventions. Measures used in complex pain include neuro-anaesthetic interventions, palliative surgery, radiotherapy, chemotherapy, physiotherapy, occupational therapy, and psychosocial care.
Analgesics
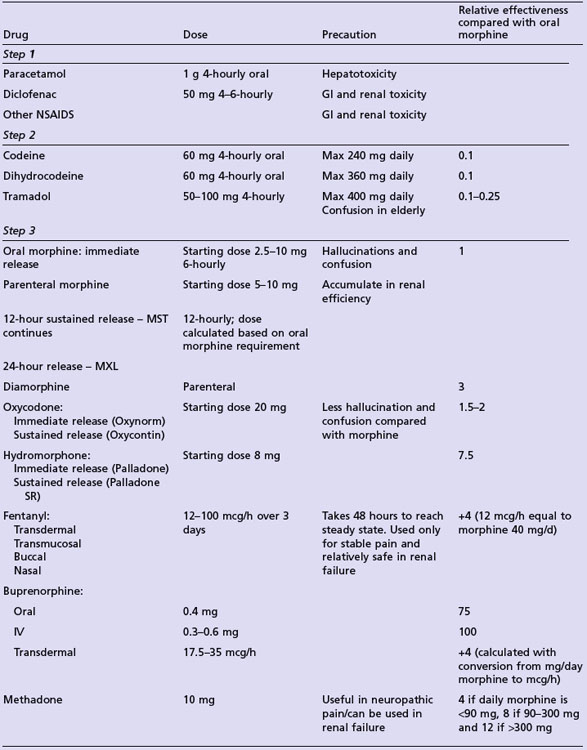
Commonly used analgesics are given in Table 7.1. Strong opioids are started at a low dose and titrated according to the clinical need (Box 7.2). Morphine is the strong agent of choice and oral administration is preferred. Transdermal preparations are useful only in stable pain. Some agents may only be prescribed by specialists in palliative care medicine or anaesthetia.
Box 7.2
Titration of opioid dose
Step 1
Step 3
Opioid side effects, toxicity and management
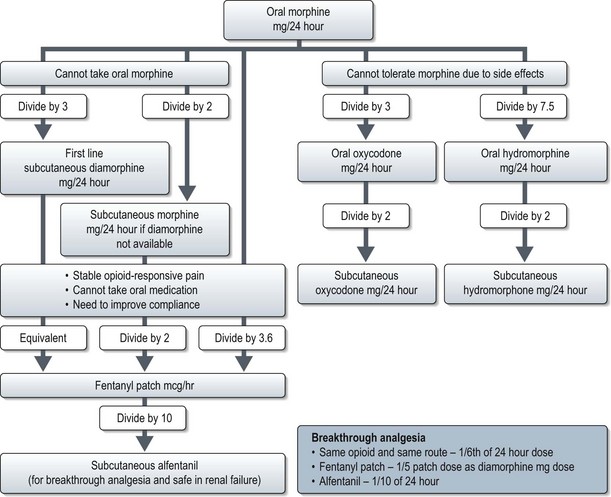
All patients feel some degree of drowsiness when starting or increasing their dosage. This usually wears off 3–5 days after being on a stable dose. Constipation is inevitable and 30–50% patients develop nausea and vomiting; these symptoms should be managed prophylactically. Intolerable side effects necessitate switching to an alternative opioid (Figure 7.2).
Opioid toxicity usually manifests pseudo-hallucinations (shadows at the peripheries of the field of vision), myoclonic jerks, cognitive impairment, and visual and auditory hallucinations. Initial management includes adequate hydration (dehydration is often a precipitant of toxicity), reduction of opioid and haloperidol (1.5–3 mg oral) for cognitive impairment. If the patient has persistent toxicity without adequate analgesia, opioid switching is needed (Figure 7.2). Though there is no best choice, oxycodone and hydromorphone are the usual alternatives. Naloxone is a short acting opioid antagonist used intravenously for reversing accidental severe opioid overdose.
Adjuvant analgesics
Adjuvant analgesics (Table 7.2) are a useful complement to regular analgesics in complex pain. These include anticonvulsants, antidepressants, antispasmodics, bisphosphonates, steroids, muscle relaxants and N-methyl-D-aspartate antagonist (ketamine).
| Indication | Drug | Dosage |
|---|---|---|
| Neuropathic pain | Dexamethasone | 8–16 mg daily |
| Gabapentin | 100–300 mg (nocte) Titrate to 600 mg TDS | |
| Amitriptyline | Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|