##
The differential diagnosis in a patient with primary aldosteronism (PA) when bilateral adrenocortical nodules are found on adrenal computed tomography (CT) scan includes bilateral idiopathic nodular hyperplasia, bilateral aldosterone-producing adrenal adenomas, unilateral aldosterone-producing adenoma and contralateral nonfunctioning nodule, and a mix of aldosterone- and cortisol-producing adrenal adenomas. All patients who have an adrenal nodule on CT should be evaluated for cortisol secretory autonomy with baseline blood dehydroepiandrosterone sulfate (DHEA-S) concentration and an overnight dexamethasone suppression test (DST). Whether to pursue subtype evaluation with adrenal venous sampling (AVS) is based on a shared decision-making discussion with the patient. If the patient would like to pursue the surgical treatment option and is a reasonable surgical candidate, then AVS is the best next step.
Case Report
The patient was a 69-year-old African American man with a 15-year history of hypertension. He was treated with a three-drug program: β-adrenergic blocker (carvedilol 25 mg twice daily), direct vasodilator (hydralazine 100 mg three times per day), and an angiotensin receptor blocker (losartan 50 mg daily). Blood pressure control was not optimal, with systolic blood pressures typically in the mid-150s mmHg. Spontaneous hypokalemia was first noted 7 years previously with serum potassium concentrations of 3.2 mmol/L and 3.1 mmol/L, but remarkably, he was not tested for PA until recently. At the time of referral to Mayo Clinic he was taking 160 mEq of potassium chloride daily to maintain a normal serum potassium concentration. Beyond hypertension and chronic kidney disease (CKD), the patient was healthy. He had no signs or symptoms of Cushing syndrome.
INVESTIGATIONS
The baseline laboratory test results are shown in Table 9.1 . The serum creatinine concentration was consistent with stage 3a CKD—likely the result of long-standing untreated PA. The patient had positive case detection testing for PA with a plasma aldosterone concentration (PAC) >10 ng/dL and plasma renin activity (PRA) <0.6 ng/mL per hour. In addition, PA was confirmed because when a patient has spontaneous hypokalemia and the PAC >20 ng/dL, there are no other differential diagnostic possibilities beyond PA. , Thus formal confirmatory testing with oral sodium loading or a saline infusion test was not needed. The low-normal levels of DHEA-S and corticotropin (ACTH) suggested that there may be a component of subclinical glucocorticoid secretory autonomy—a suggestion that was confirmed with lack of normal suppression of the serum cortisol concentration with the overnight 2-mg DST (see Table 9.1 ).
| Biochemical Test | Result | Reference Range |
| SodiumPotassiumCreatinineeGFRAldosteronePlasma renin activityDHEA-SACTH2-mg overnight DST | 1464.51.65271<0.637.3122.6 | 135–1453.6–5.20.8–1.3>60 mL/min per BSA≤21 ng/dL≤0.6–3 ng/mL per hour25–131 mcg/dL7.2–63 pg/mL<1.8 mcg/dL |
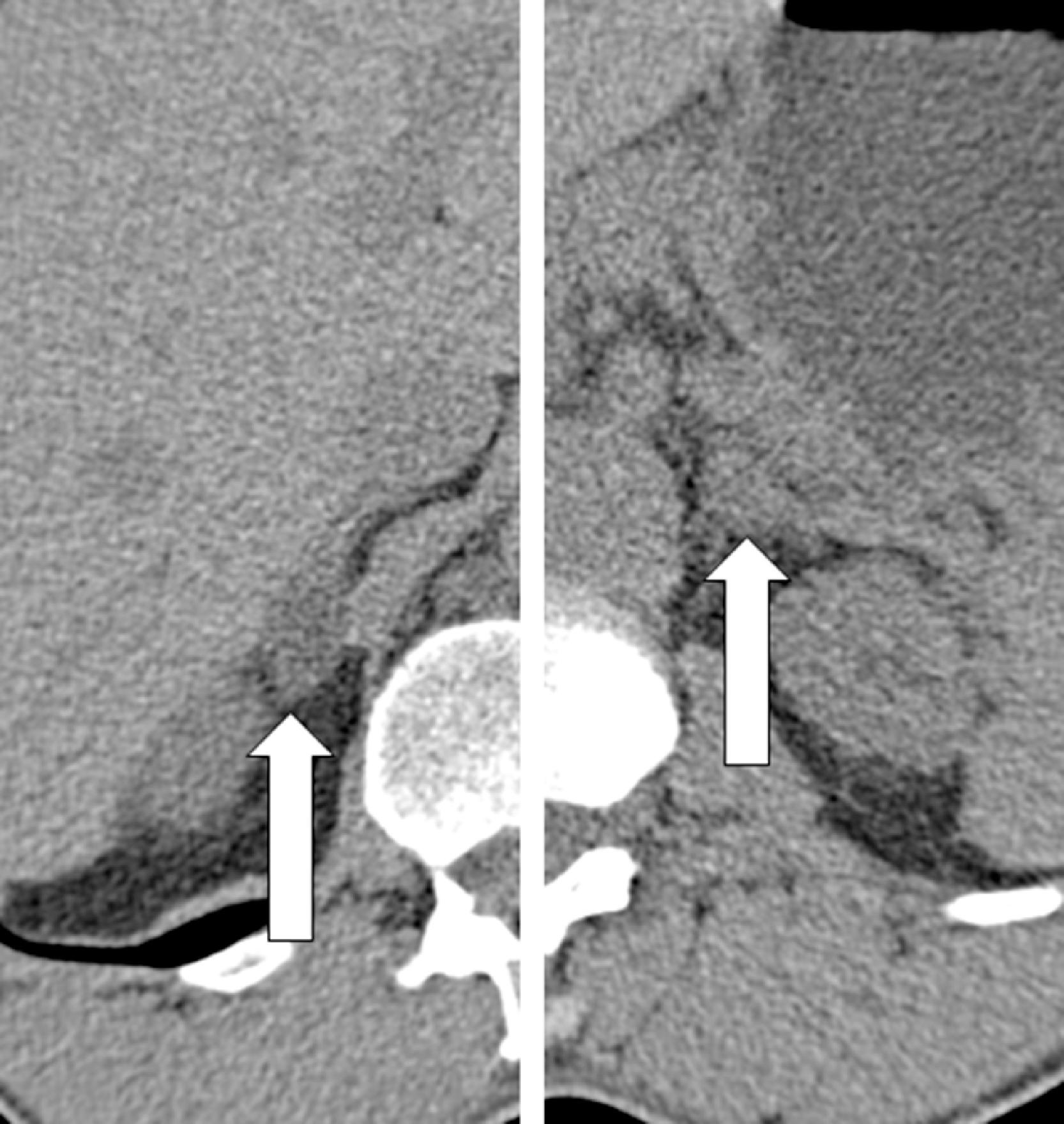
An unenhanced adrenal-dedicated CT scan showed a lipid-rich 1.2 × 1.6 cm right adrenal nodule and a lipid-poor 1.0-cm left adrenal nodule ( Fig. 9.1 ).
After a thorough discussion with the patient, it was clear that the patient was keen to pursue a surgical cure of hypokalemia and better control of his hypertension on less medication. He understood that a cure of his hypertension with surgery was not a reasonable goal in view of the duration of hypertension of >10 years and the presence of CKD. , He was also counseled that patients with PA hyperfiltrate at the kidney the degree of renal insufficiency is actually worse than it appears—PA “masks” the degree of underlying CKD. , This is not a reason to avoid effective therapy for a patient, but rather something that the patient and all of his or her physicians need to understand because the serum creatinine will rise after effective treatment with either surgery or treatment with a mineralocorticoid receptor antagonist. ,
AVS was performed as the next step. The patient was well hydrated with intravenously administered saline. In addition, care was taken to limit the use of contrast dye. AVS was successful based on adrenal vein-to-inferior vena cava (IVC) cortisol gradients of more than 5-to-1 ( Box 9.1 ). , With the continuous cosyntropin infusion protocol (cosyntropin 50 mcg/h administered intravenously starting 30 minutes before AVS and continued throughout the procedure), the adrenal-to-IVC cortisol gradients are typically well above the 5-to-1 cutoff (in this case, 22.8-to-1 on the right and 13.1-to-1 on the left). Each adrenal aldosterone concentration is divided by the respective cortisol concentration for the A/C ratio (see Box 9.1 ). The A/C ratio from the dominant adrenal is divided by the A/C ratio from the nondominant adrenal for the aldosterone lateralization ratio. In this case, 46.8 on the left is divided by 1.9 on the right, yielding an aldosterone lateralization ratio of 24.6-to-1 (left-to-right). When the aldosterone lateralization ratio is >4-to-1, unilateral adrenalectomy will be curative. , It is also reassuring to confirm relative suppression of aldosterone secretion from the nondominant adrenal by dividing the A/C ratio from the nondominant adrenal by the A/C ratio from the IVC. , In this case, the A/C ratio of 1.9 on the right was divided by 9.4 from the IVC, yielding a value of 0.2. Contralateral adrenal suppression is confirmed when this value is <1.0. Thus the larger adrenal nodule in the right adrenal gland was not the source of aldosterone excess.