##
Bilateral macronodular adrenal hyperplasia (BMAH) is typically a computed tomography (CT)-based diagnosis. When patients present with primary aldosteronism (PA) and BMAH is found on the CT scan, the aldosterone hypersecretion is bilateral and usually associated with cortisol cosecretion, resulting in either clinically evident Cushing syndrome or subclinical Cushing syndrome (also referred to as “mild autonomous cortisol secretion”). Adrenal venous sampling (AVS) is usually not needed in this setting because, by definition, the disorder is bilateral. Treatment is surgical. If the patient has subclinical Cushing syndrome (mild autonomous cortisol secretion), then there is the opportunity to resect the larger adrenal gland to debulk the disease. If the patient has clinically overt Cushing syndrome, bilateral adrenalectomy is the best treatment option.
Case Report
The patient was a 69-year-old man with a 34-year history of hypertension; PA was diagnosed 9 years previously when he presented with spontaneous hypokalemia. His visit to Mayo Clinic was triggered by accelerated hypertension 6 months prior. He was treated with a four-drug program: calcium channel blocker (nifedipine 30 mg daily), β-adrenergic blocker (carvedilol 12.5 mg twice daily), an angiotensin receptor blocker (losartan 100 mg daily), and a diuretic (chlorthalidone 25 mg daily). Blood pressure control was not optimal. At the time of referral to Mayo Clinic he was taking 40 mEq of potassium chloride daily in an effort to maintain a normal serum potassium concentration. Beyond hypertension and hypokalemia, the patient was healthy. He had no signs or symptoms of overt Cushing syndrome. He did not have diabetes mellitus or osteoporosis. He had one first-degree relative who had been diagnosed with hypertension.
INVESTIGATIONS
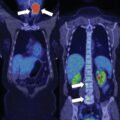
The baseline laboratory test results are shown in Table 11.1 . The patient had positive case detection testing for PA with plasma aldosterone concentration (PAC) >10 ng/dL and plasma renin activity (PRA) <1.0 ng/mL per hour. In addition, PA was confirmed because when a patient has spontaneous hypokalemia (noted prior to diuretic therapy) and PAC >20 ng/dL, there are no other differential diagnostic possibilities beyond PA. , Thus formal confirmatory testing with oral sodium loading or a saline infusion test was not needed for this patient. The diagnosis of glucocorticoid secretory autonomy was based on low serum corticotropin (ACTH) concentration, low-normal serum dehydroepiandrosterone sulfate (DHEA-S) concentration, mild elevation in 24-hour urinary free cortisol excretion, and lack of complete suppression in serum cortisol with an overnight 8-mg dexamethasone suppression test (DST) (see Table 11.1 ). An unenhanced abdominal CT scan showed bilateral macronodular hyperplasia ( Fig. 11.1 ).
| Biochemical Test | Result | Reference Range |
| Sodium, mmol/LPotassium, mmol/LCreatinine, mg/dLAldosterone, ng/dLPlasma renin activity, ng/mL per hourDHEA-S, mcg/dLACTH, pg/mL1-mg overnight DST, mcg/dL8-mg overnight DST, mcg/dL24-hour urine cortisol, mcg | 1444.01.024<0.639132.53.684 | 135–1453.6–5.20.8–1.3≤21 ng/dL≤0.6–312–22710–60<1.8<1.0<45 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree