##
Mineralocorticoid receptor antagonists (MRAs) (e.g., spironolactone and eplerenone) prevent aldosterone from activating the receptor, resulting, sequentially, in sodium loss, a decrease in plasma volume, and an elevation in renin. If plasma renin activity (PRA) or plasma renin concentration (PRC) is not suppressed in a patient treated with a MRA, then no further primary aldosteronism (PA)-related testing can be performed, and the MRA should be discontinued for 6 weeks before retesting. However, if the patient is hypokalemic despite treatment with a MRA, then the mineralocorticoid receptors are not fully blocked, and PRA or PRC should be suppressed in such a patient with PA. In addition, most patients with PA are treated with suboptimal dosages of MRAs, and the mineralocorticoid receptors are not fully blocked. Thus for case detection testing, blood pressure medications, including MRAs, should not be discontinued. In the setting of suppressed PRA or PRC, clinicians can proceed with case detection testing in all patients treated with MRAs, and the MRA does not need to be discontinued for confirmatory or subtype testing with adrenal venous sampling (AVS).
Case Report
The patient was a 57-year-old woman with an 11-year history of hypertension. She was treated with a four-drug program: β-adrenergic blocker (atenolol 50 mg daily), calcium channel blocker (nifedipine extended release 60 mg per day), an angiotensin-converting enzyme inhibitor (lisinopril 20 mg daily), and a mineralocorticoid receptor antagonist (spironolactone 100 mg daily). She was also taking 60 mEq of potassium chloride twice daily. Hypokalemia was first noted 1 year previously when her serum potassium level was 2.2 mEq/L. Her home blood pressures averaged 117/72 mmHg. Before the hypokalemia was treated, she had frequent nocturia, which improved with restoration of her serum potassium to normal. She had been treated with spironolactone for the past 1 year. There was a strong family history of hypertension in both parents and her son, as well as the paternal aunts and uncles. She had no other major medical health issues. She had no signs or symptoms of Cushing syndrome.
INVESTIGATIONS
The baseline laboratory test results are shown in Table 13.1 . The patient had positive case detection testing for PA with a PAC >10 ng/dL and the PRA <0.6 ng/mL per hour. In addition, PA was confirmed because when a patient has spontaneous hypokalemia and the PAC >20 ng/dL, there are no other differential diagnostic possibilities beyond PA. , Thus formal confirmatory testing with oral sodium loading or a saline infusion test was not needed.
| Biochemical Test | Result | Reference Range |
| SodiumPotassiumCreatinineeGFRAldosteronePlasma renin activityDHEA-S | 1383.50.9>6075<0.6112 | 135–1453.6–5.20.8–1.3>60 mL/min per BSA≤21 ng/dL≤0.6–3 ng/mL per hour16–195 mcg/dL |
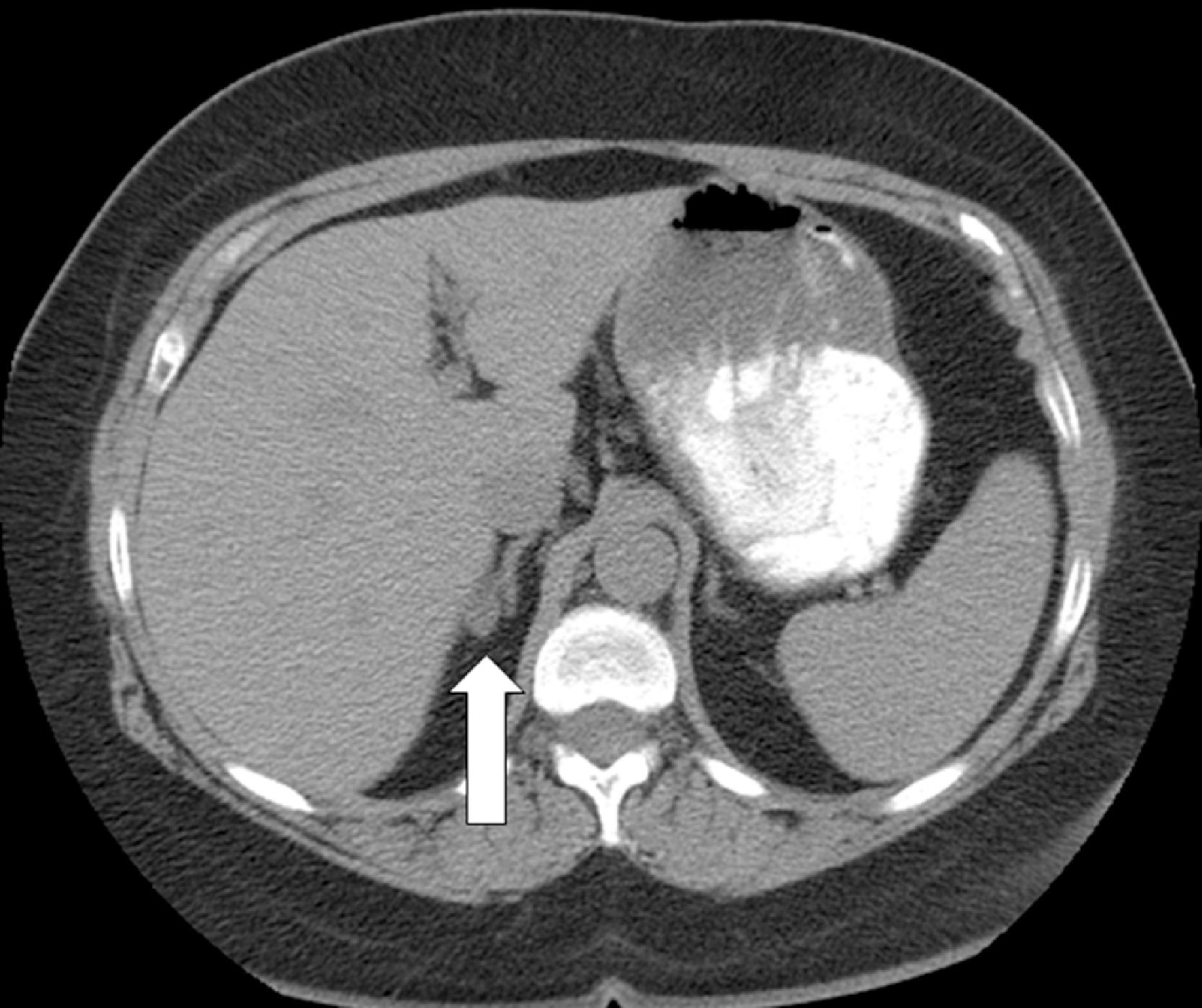
An unenhanced adrenal-dedicated computed tomography (CT) scan showed an indeterminate attenuation 1.2-cm right adrenal nodule and a 0.3-cm left adrenal nodule ( Fig. 13.1 ).