PREVENTION, DIAGNOSIS, AND MANAGEMENT
Part of “CHAPTER 61 – RENAL OSTEODYSTROPHY“
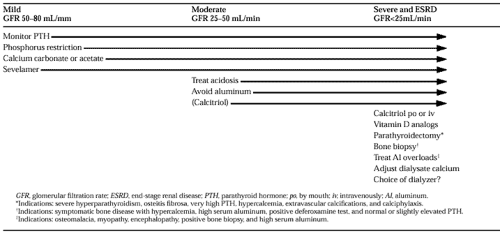
An understanding of the pathogenesis of renal osteodystrophy leads to a number of maneuvers that are effective in its prevention and treatment; these are summarized in Table 61-1.
DIETARY PHOSPHORUS RESTRICTION
The cornerstone for the prevention and treatment of renal osteodystrophy is the restriction of phosphorus and the prevention of hyperphosphatemia. The usual phosphorus intake by normal adults is 1 to 1.6 g per day, from meat and dairy products. The dietary restriction of these foods is useful, but as renal failure becomes advanced, additional strategies to limit phosphate absorption are required. This is achieved by the use of calcium salts, calcium carbonate or calcium acetate, or sevelamer, a non–calcium-containing phosphate-binding polymer, taken with meals, which bind the ingested phosphorus in the gastrointestinal tract and prevent its absorption.58,59,60,61 and 62 The goal of this treatment is to reduce the serum phosphate level to ˜5 mg/dL. Serum phosphate levels should be closely monitored to avoid hypophosphatemia. Although aluminum-containing antacids are extremely effective in controlling serum phosphorus levels, these agents are not often used except for short-term administration because of the toxicity of aluminum in causing dialysis dementia and osteomalacia.46,63 The administration of antacids such as calcium carbonate, calcium acetate, or sevelamer must be adjusted according to the approximate phosphorus content of the meal. Thus, a small breakfast (50–75 mg of phosphorus) may require small amounts of a phosphate binder, whereas a larger meal (600 mg of phosphorus) may require increased amounts. Calcium citrate should not be used, because aluminum absorption may be increased.
CALCIUM SUPPLEMENTATION
Because intestinal calcium absorption is decreased in patients with advanced renal failure, and because their diets are usually low in calcium, the supplementation of calcium intake is required.64,65 The minimum requirement is 1.5 g per day of elemental calcium; larger doses may be given, especially if hypocalcemia persists. As discussed previously, large doses of calcium carbonate or calcium acetate are also useful as phosphate binders for the control of hyperphosphatemia and prevention of hyperparathyroidism; if such doses of calcium are given, the levels of serum calcium and phosphate must be monitored frequently to avoid hypercalcemia and an elevation of the calcium-phosphorus product.
USE OF VITAMIN D STEROLS
Because low levels of calcitriol play a major role in the pathogenesis of hyperparathyroidism in chronic renal disease, the administration of calcitriol has an important role in its treatment. In some countries, 1α-hydroxycholecalciferol, which is metabolized to calcitriol, is used. The administration of calcitriol is effective in achieving suppression of PTH levels with significant improvements in skeletal histology.66 The use of calcitriol may vary according to the degree of renal insufficiency and the degree of hyperparathyroidism. In early renal failure, the oral administration of calcitriol, 0.25 to 0.5 μg per day, may be effective in minimizing hyperparathyroidism. However, that therapy should be monitored closely so that hypercalcemia and hypercalciuria do not occur, because a risk exists that renal function may be compromised. In end-stage renal disease, larger doses of calcitriol may be required. In patients on hemodialysis, the intravenous administration of calcitriol is associated with marked suppression of elevated PTH values and improvement in renal osteodystrophy. The
doses required are 1 to 3 μg given intravenously with each dialysis. As before, levels of calcium and phosphorus and their products must be monitored closely to avoid severe hypercalcemia, an elevated calcium × phosphate product, and metastatic calcification. The intermittent administration of large doses of calcitriol orally (2–5 μg twice per week) has also been shown to be effective, and this pulse dosing can achieve a significant reduction in PTH levels, comparable to that achieved with intravenous administration.67,68 and 69 This mode of administration is also applicable to patients on CAPD.70 The increased efficacy of intermittent administration, whether by intravenous or oral routes, may be due to the high levels achieved in serum, which allow increased delivery to peripheral tissues, including the parathyroid glands.71 In the parathyroid, the induction of the vitamin D receptor by calcitriol may allow the glands to become more responsive to the prevailing levels of calcitriol and calcium. If the degree of hyperparathyroidism is severe (e.g., intact PTH of >2000 pg/mL), suppression of PTH by calcitriol may prove difficult. This may be explained by the relative lack of vitamin D receptor and calcium-sensing receptor in nodular hyperplastic parathyroid glands; thus, the administered calcitriol or elevations in serum calcium would be less effective in suppressing PTH biosynthesis. Such large glands may require excision. An analog of calcitriol with less calcemic effects, 19-nor-1α-25-dihydroxy-vitamin D2 (paricalcitol) is available for the treatment of hyperparathyroidism in renal failure.72 Other analogs, 22-oxacalcitriol, falecalcitriol, and 1α-hydroxy vitamin D2, are in clinical trials for the same purpose.73,74 and 75
doses required are 1 to 3 μg given intravenously with each dialysis. As before, levels of calcium and phosphorus and their products must be monitored closely to avoid severe hypercalcemia, an elevated calcium × phosphate product, and metastatic calcification. The intermittent administration of large doses of calcitriol orally (2–5 μg twice per week) has also been shown to be effective, and this pulse dosing can achieve a significant reduction in PTH levels, comparable to that achieved with intravenous administration.67,68 and 69 This mode of administration is also applicable to patients on CAPD.70 The increased efficacy of intermittent administration, whether by intravenous or oral routes, may be due to the high levels achieved in serum, which allow increased delivery to peripheral tissues, including the parathyroid glands.71 In the parathyroid, the induction of the vitamin D receptor by calcitriol may allow the glands to become more responsive to the prevailing levels of calcitriol and calcium. If the degree of hyperparathyroidism is severe (e.g., intact PTH of >2000 pg/mL), suppression of PTH by calcitriol may prove difficult. This may be explained by the relative lack of vitamin D receptor and calcium-sensing receptor in nodular hyperplastic parathyroid glands; thus, the administered calcitriol or elevations in serum calcium would be less effective in suppressing PTH biosynthesis. Such large glands may require excision. An analog of calcitriol with less calcemic effects, 19-nor-1α-25-dihydroxy-vitamin D2 (paricalcitol) is available for the treatment of hyperparathyroidism in renal failure.72 Other analogs, 22-oxacalcitriol, falecalcitriol, and 1α-hydroxy vitamin D2, are in clinical trials for the same purpose.73,74 and 75
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree