Preparation for Radiation Treatment Planning
INTRODUCTION
Some of the most important steps in gynecologic radiation treatment planning occur well before the first radiation field or target volume has been designated. Adequate preparation prevents wasted time but, more importantly, reduces the likelihood of suboptimal, potentially ineffective treatment. Key steps in the preplanning preparatory period include the following:
Information gathering. In every case, the quality of treatment depends critically on the quality of information about the nature and extent of the patient’s tumor. The most detailed plan can fail if a region of gross or high-risk microscopic disease is overlooked and therefore treated to an inadequate dose.
Development of an overall radiation treatment strategy. As discussed in Chapters 7, 8, and 10,11,12,13,14 and 15, some final decisions about the method of boosting gross disease may be delayed until the initial tumor response has been evaluated in the fourth or fifth treatment week. However, a decision tree mapping out potential strategies should always be developed before the initial plan is determined.
Patient set-up and preparation for external beam radiation therapy. Features of the initial simulation, including the patient’s position, placement of orienting radio-opaque markers, location of the central axis, and other factors, strongly influence the quality of the final treatment plan.
This chapter focuses on this initial stage of radiation therapy planning, with a focus on those aspects that are particularly relevant to the management of gynecologic cancers.
INFORMATION GATHERING—THE INITIAL PATIENT EVALUATION
What to Look for in the Clinical Record
Before processes of simulation, target definition, and treatment planning are begun, all potentially relevant clinical records (including pathology reports, operative reports, outside treatment records, and imaging studies) should be carefully reviewed to gain as much information as possible about the distribution of disease, recurrence risk, and any factors that could compromise treatment or contribute to the risk of treatment-related side effects.
Pathology Reports
Every treatment decision hinges on the findings described in a pathology report. Ambiguities can arise because of inexpert interpretation but also because of poorly articulated or erroneously transcribed findings. Modern synoptic reports reduce the potential for miscommunication. However, whenever there is doubt about the accuracy or clarity of the reported findings, the case should always be discussed directly with the examining pathologist or, if necessary, sent for review by an expert gynecologic pathologist.
Specific key features that guide decisions about treatment of various cancers are discussed in detail in the disease site chapters. However, in general, there should always be a clear description of the primary tumor, including:
Histology. If unusual characteristics make the tumor difficult to classify, this should be clearly explained. For müllerian tumors, the histologic variant should always be described unambiguously (Chapters 1 and 13). For mixed
tumors, the percentages of different variants within the tumor should be given. For adenocarcinomas, a histologic grade should always be specified (Chapter 1).
For biopsies, the adequacy of the biopsy specimen. Would more tissue clarify the diagnosis?
The orientation of tumor within the specimen. This should be part of the gross description. Orientation is particularly important if there are close or positive surgical margins following hysterectomy or wide local excision of a vulvar cancer.
The distance (in millimeters) between the surgical margin and the closest tumor within the specimen. We have seen reports describing margins as “negative” when the tumorfree margin was <0.1 mm! The location of any close or positive margin should also be specified.
The depth of stromal invasion. This should be described in millimeters and (for uterine and cervical cancers) as a percentage of the stromal thickness.
The size of the primary tumor. For almost all gynecologic malignancies, tumor size is an important prognostic factor.
Lymph vascular space invasion (LVSI). The presence or absence of LVSI should be noted. In some cases, this may be described as extensive or focal.
If a lymphadenectomy has been performed, the following details should always be specified:
The locations and numbers of recovered lymph nodes. This description should include the nodal stations and laterality of recovered nodes. Reports that simply state “pelvic lymph nodes, no evidence of metastasis” are inadequate even if the number of nodes removed is described, because the adequacy of dissection within nodal stations cannot be ascertained. The original pathology report often contains more complete information about nodal counts than secondary reviews.
The number and location of positive nodes.
The size of metastatic foci within nodes.
The presence or absence of extranodal extension (ECE). Although the importance of ECE has been particularly emphasized for vulvar cancers, it is undoubtedly an important prognostic factor for regional control of any carcinoma treated with adjuvant radiation therapy and is a key factor in determining the dose of radiation. If the location of ECE can be elicited from pathology, operative, or imaging reports, it can significantly reduce the size of the high-risk target volume.
Operative Reports
The reports of any potentially relevant operations should be obtained. Any ambiguities should be clarified through direct discussion with the surgeon. A thorough review of operative reports can provide key information about the following:
The location of tissues that may be at high risk for residual gross or microscopic disease.
The extent of lymph node dissections. In particular, the proximal extent of the dissection can often be determined from a careful review of the operative report.
The presence of adhesions or intraoperative events that could influence the likelihood of treatment-related side effects. In particular, injury to bowel, bladder, ureters, or other critical structures should be considered when assessing the risk of late complications of combined modality treatment.
Outside Imaging Studies
Whenever possible, the original images from diagnostic studies should be obtained and reviewed, particularly if the results could have an influence on decisions about the treatment volume or radiation dose. Review of outside reports can be valuable but is often insufficient for the purposes of radiation oncology planning for a number of reasons.
In many cases, the original studies are shown to be of poor quality or fail to include an area of interest.
A second review can often pick up important findings that were missed in the initial interpretation.
The initial extent and anatomic locations of tumors and lymph nodes are much more readily appreciated when the report is read while viewing the actual images.
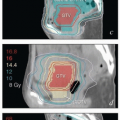
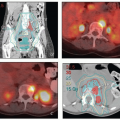
Digital imaging and communications in medicine (DICOM) images of contrast-enhanced CT scans, PET scans, and MRIs can be fused with treatment planning CTs, dramatically improving the speed and accuracy of target definition.
Outside Radiation Therapy Records
Detailed records should always be obtained before treating or denying treatment to a patient who has had radiation therapy in or close to the region of interest. Treatments described as, for example, “whole pelvic radiation” can vary widely. Detailed review of previous treatments often reveals that a lesion thought to represent an in-field recurrence is actually marginal to the prior radiation fields.
Written treatment summaries in the form of textual descriptions are insufficient unless previous treatment fields were far from the new area of interest. Color axial isodose distributions at intervals of 1 cm or less covering the entire treatment volume combined with central axis sagittal and coronal reconstructions may be sufficient to determine whether retreatment is possible. For patients who have had 3-D conformal treatment, digitally reconstructed radiographs showing the treatment fields are very helpful. In some cases, it is worthwhile to attempt to obtain original DICOM files; with some physics support and compatible treatment planning systems, these can be used to gain more detailed information about the doses of radiation delivered from previous treatments.
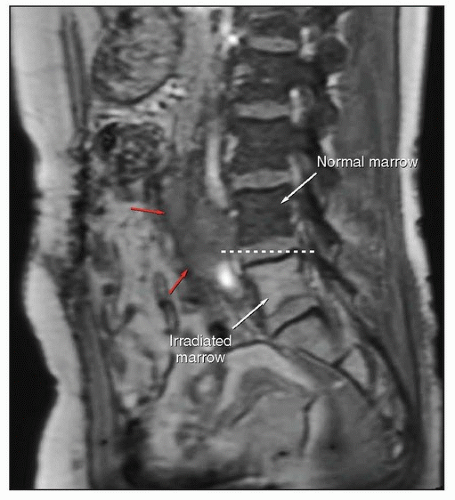
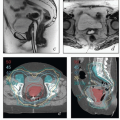
If the radiation therapy records have been destroyed or are unobtainable for other reasons, an estimate of the proximal border of the treatment fields may be made using T1-weighted MRI (Fig. 4.1).
Clinical Examination of the Pelvis
A detailed pelvic examination is a critical part of the evaluation of every patient considered for radiation therapy of a gynecologic cancer. Because clinical descriptions cannot always impart the details required for treatment planning, the treating radiation oncologist should personally perform an examination before initiating treatment. Although high-quality MRI can provide remarkable anatomic detail, superficial vaginal disease and small vulvar lesions are poorly visualized on MRI. Clinical examination commonly complements the findings of diagnostic imaging, allowing evaluation of the mobility and tenderness of abnormal lesions and clarifying the relationship between tumor and critical structures. Pelvic examination also provides an excellent and inexpensive means of following tumor response and is used to assess a patient’s suitability for brachytherapy.
The goal of pelvic examination is to define the extent of tumor involvement without causing the patient unnecessary discomfort or bleeding. The examination of a patient with probable or known cancer should include several steps:
Preparation and reassurance. Ferric subsulfate (Monsel) solution, rectal swabs, and vaginal packing should be at hand in case they are required to achieve hemostasis after the examination. Several sizes of two-blade speculums should be available to accommodate narrow or spacious vaginas. A pediatric speculum may be needed to examine a very narrow or surgically reconstructed vagina, and extralarge Grave speculums may be required to visualize the cervix of obese patients. The patient should be placed in the lithotomy position with the perineum at the very edge of the table. She should be encouraged to relax her legs and perineal muscles. Before the examination, the patient should be reassured that she will be informed of each step of the examination and questioned about previous negative experiences or specific concerns about the examination. In every aspect, the examination should be approached at a careful pace with emphasis on obtaining high-quality information while causing the patient as little bleeding or discomfort as possible.
Inspection and palpation of the external genitalia and anus. Describe the size, appearance, and location of any abnormal lesions and their distance (in millimeters) from critical structures (anus, urethra, or clitoris). Any evidence of infection should also be noted.
Initial evaluation of the vagina. Before inserting a speculum, it is wise to gently place a finger in the distal vagina to evaluate the width of the vagina, determine the optimal speculum size, assess the presence of tumor near the introitus, and prepare the patient before inserting the speculum.
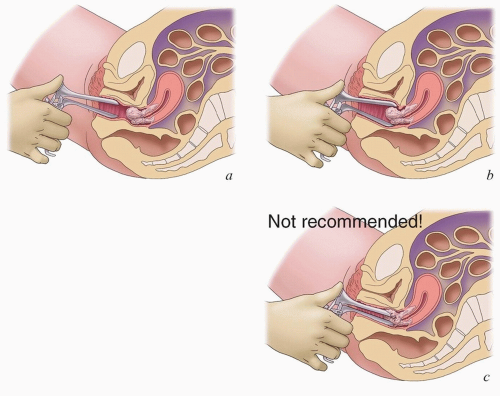
Speculum examination. The purpose of speculum examination is to visualize the cervix and vaginal surfaces. The speculum should be gradually opened as it is inserted in the vagina until the cervix appears between the anterior and posterior blade, taking care to avoid inserting the speculum directly into an exophytic lesion or scraping the speculum blades against friable tumor (Fig. 4.2). The open speculum should then be gradually withdrawn while visualizing the vaginal walls. In some cases, the anterior and posterior walls can be better visualized if the speculum is rotated while it is withdrawn. Any vaginal lesions should be described in terms of their longitudinal location (proximal, middle, or distal third), distance from the apex or hymenal ring, and their circumferential (o’clock) location. In postoperative patients, the state of the healing vaginal incision should be noted.
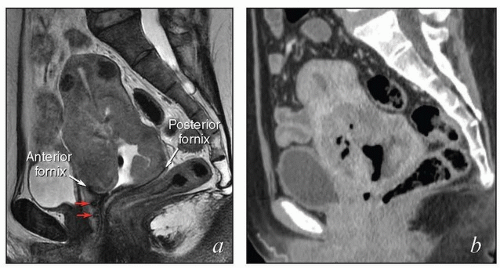
Digital vaginal examination. If there is a friable cervical or vaginal lesion, the vagina should be entered carefully with one or two fingers, avoiding direct contact with the tumor (Fig. 4.3); the examining finger(s) should be advanced to the fornix or apex of the vagina and then
rotated with the palmar surface of the fingers in contact with the vaginal walls, assessing for any abnormal lesions. The relationship between the distal tumor extent and the introitus is important for determining the distal border of radiation therapy fields. However, palpation of tumor near the introitus does not necessarily mean that the distal vagina has been infiltrated by tumor (Fig. 4.4). The size of exophytic cervical tumors can be assessed between two intravaginal fingers (Fig. 4.5). However, the size of endocervical tumor can be assessed only by rectovaginal examination.
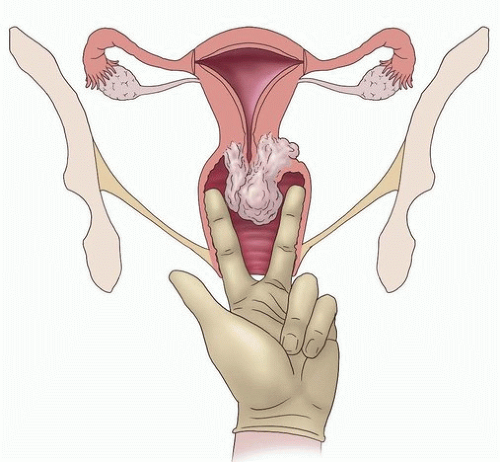
Rectovaginal examination. The purpose of rectovaginal examination is to assess the diameter of the cervix, the mobility of pelvic tumor, the presence or absence of paracervical or paravaginal involvement, and the presence of disease in the rectovaginal septum. Rectovaginal examination is typically performed with an index finger in the vagina and middle finger in the rectum (Fig. 4.6). Righthanded examination tends to give better appreciation of the right parametrium and vice versa. The diameter of the cervix is estimated by comparing it with the diameter of the pelvis (usually about 12 cm). Tumor in the perineum can be effectively evaluated with one index finger in the distal vagina and the other in the anus.
Bimanual examination. The size of the uterus and the size and mobility of the ovaries may be assessed by capturing these structures between one hand on the lower abdomen and two fingers in the vagina. This part of the examination is impossible in obese patients, and the status and size of uterus and ovaries are often better evaluated with ultrasound or tomographic imaging.
In some cases, pain, anxiety, obesity, or other factors make it difficult to obtain a satisfactory examination in clinic. In these cases, examination under anesthesia may be needed to determine the extent of disease and to define a treatment plan. We recommend examination under anesthesia for most patients with vaginal cancer and many patients with locally advanced vulvar cancers. Where appropriate, such examination can be accompanied by cystoscopy, proctoscopy, or placement of fiducial markers (discussed below).
Diagnostic Imaging Studies
This discussion focuses on some general principles and on some potential pitfalls associated with the use of diagnostic imaging studies, particularly for the assessment of possible regional metastases from gynecologic cancers. Disease site-specific diagnostic imaging strategies, particularly evaluation of the primary site, are discussed in detail in Chapters 10,11,12,13,14 and 15.
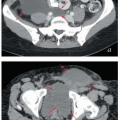
Evaluation of Regional Lymph Nodes
Gynecologic cancers commonly involve regional lymph nodes. However, even patients who have extensive regional metastases can frequently be cured if the treatment volume fully encompasses the region at risk for nodal metastasis and if the radiation dose is sufficient to control metastatic sites.
The volume of regional treatment is based on an understanding of locoregional anatomy as discussed in Chapter 5.
The volume of regional treatment is based on an understanding of locoregional anatomy as discussed in Chapter 5.
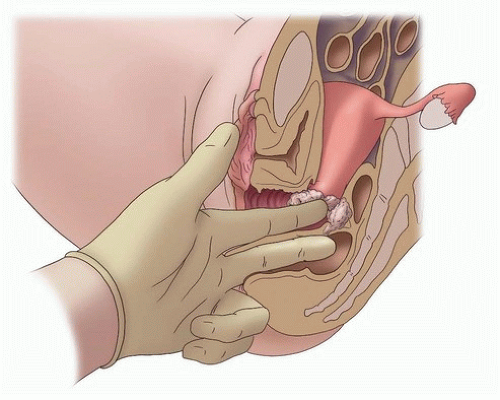 FIGURE 4.6 Rectovaginal examination. Rectovaginal examination permits evaluation of paracervical tissues, specifically the cardinal and uterosacral ligaments, which may be infiltrated by tumor. The index finger should be placed lateral to any exophytic cervical tumor in the vaginal fornix. The rectal finger is then used to palpate any nodularity that may be present superior to the fornix in the paracervical space. It is important to confirm that the rectal finger is high enough to palpate the paracervical tissues; nodular intravaginal tumor that is felt by the rectal finger should not be confused with parametrial tumor infiltration.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|