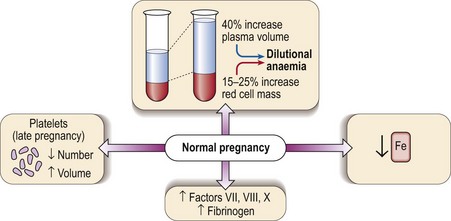
44 Several haematological changes occur in normal pregnancy (Fig 44.1). Beginning in the sixth week there is an increase in plasma volume accompanied by an increase in red cell mass. The plasma volume expansion peaks at around 24 weeks when it is approximately 40% greater than in a non-pregnant woman. As the increase in red cell mass is more modest (15–25%) a dilutional anaemia is inevitable. In practice the haematocrit and haemoglobin level start to fall at 6–8 weeks and reach a trough at around 20 weeks. It is unusual for the haemoglobin level to fall below 100 g/L and if this happens another cause for anaemia should be sought. Negative iron balance can be regarded as routine in pregnancy and as discussed below frank iron deficiency commonly occurs.
Pregnancy
Haematological changes
Oncohema Key
Fastest Oncology & Hematology Insight Engine