and Christian Waldherr1
(1)
Bern, Switzerland
7.1 Case 1
General Information/Clinical Issues
Patient was a 62-year-old female; breast-conserving therapy on left side medial in 2011, S-vacuum-assisted biopsy (S-VAB) in 2012.
Mammographic Analysis on 2D (Synthetic) and 3D
Breast density ACR I. 2D (synthetic) (Fig. 7.1a, b) and 3D (Fig. 7.2a, b and Fig. 7.3 [3D magnification, same figure as Fig. 7.2b]) in 2012 show an extensive oval irregularly shaped nonspecific density that may be due to postoperative scar; also persistent seroma with additional lucent round oil cyst or fat necrosis and associated dystrophic calcifications; BI-RADS 0. Follow-up 2D (synthetic) (Fig. 7.4a, b) and 3D (Figs. 7.5a, b and Fig. 7.6 [3D magnification, same figure as Fig. 7.5b]) in 2013 show a decrease in size and density after S-VAB; BI-RADS 2.
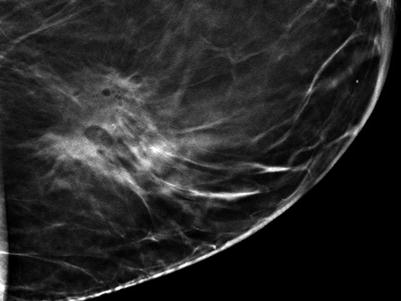
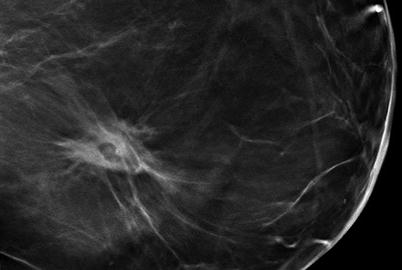
Fig. 7.1
(a, b) 2D synthetic (a) obl and (b) cc in 2012
Fig. 7.2
(a, b) 3D (a) obl and (b) cc in 2012
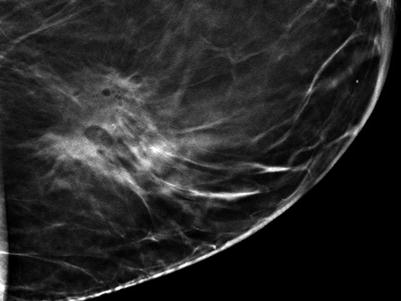
Fig. 7.3
3D Magnification in 2012
Fig. 7.4
(a, b) 2D synthetic (a) obl and (b) cc in 2013
Fig. 7.5
(a, b) 3D (a) obl and (b) cc in 2013
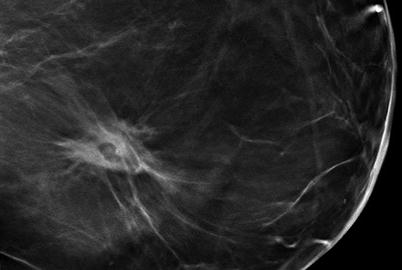
Fig. 7.6
3D Magnification in 2013
Differential Diagnosis on 2D (Synthetic)
In the situation of previously treated breast cancer, benign scarring, persistent seroma, oil cysts, fat necrosis, and dystrophic calcifications are common; risk of recurrence increases with positive margins (R1) and without radiation therapy (BI-RADS 0).
Conclusion/Diagnosis with 3D
3D may avoid unnecessary biopsies due to its more detailed morphology of scar and fat necrosis (BI-RADS 2).
Recommendation
Additional US, no S-VAB recommended in this case (S-VAB was the explicit request of the patient in 2012).
US
Benign scar with partial posterior shadowing and associated absorbed seroma on follow-up (Fig. 7.7)
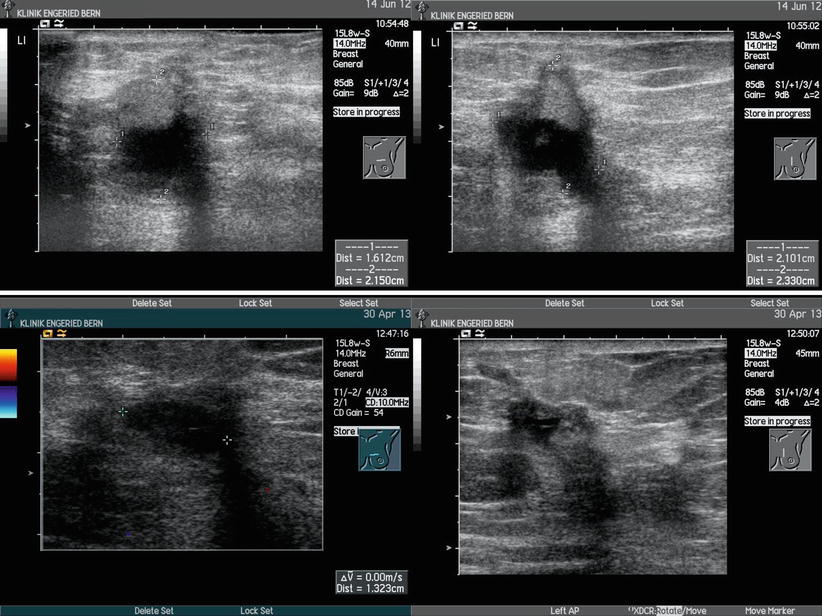
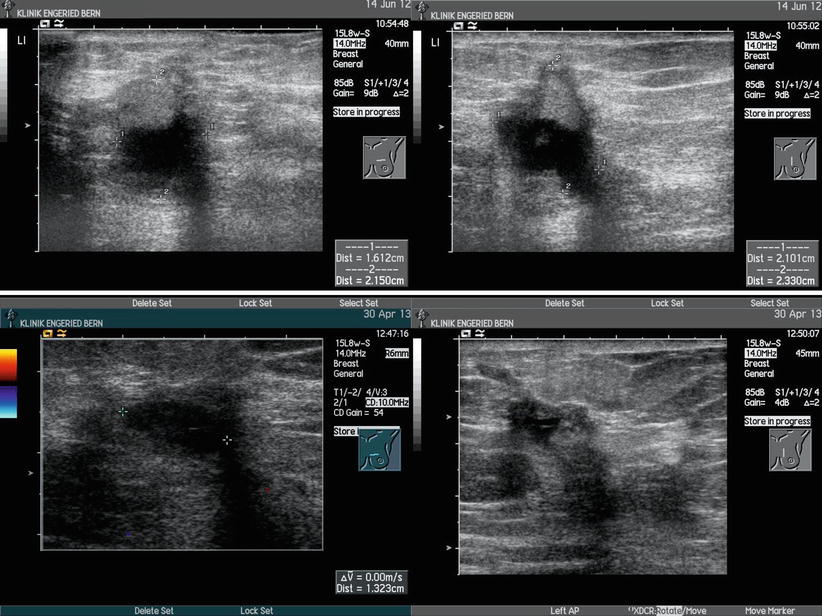
Fig. 7.7
US in 2012 and 2013
Histology After S-VAB
Granulated calcified fat necrosis and extensive scarred areas; B2 (Fig. 7.8).
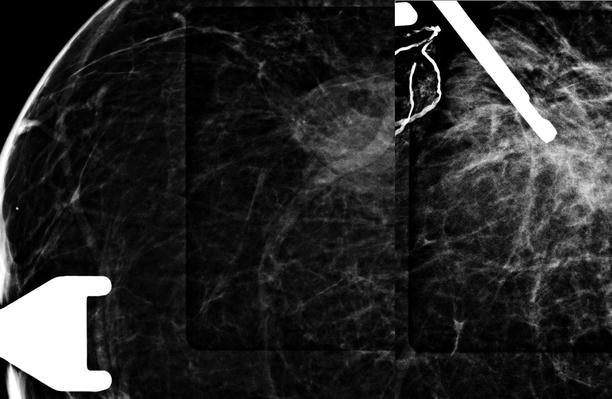
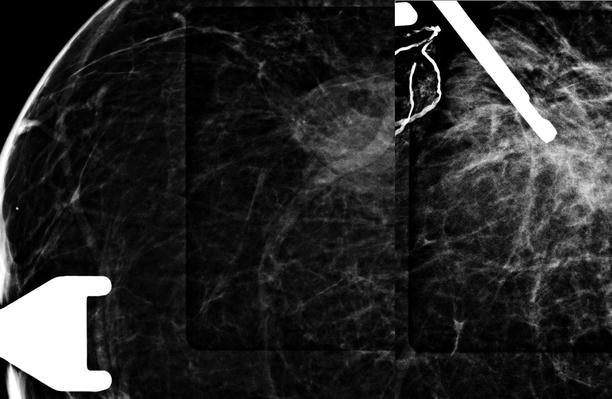
Fig. 7.8
S-VAB in 2012
Further Imaging/Further Diagnostic
In diagnostic uncertainty perform MRI and distinguish scar from recurrence.
7.2 Case 2
General Information/Clinical Issues
Patient was a 67-year-old female; breast-conserving therapy in 2006 on right side at 11–12 o’clock.
Mammographic Analysis on 2D and 3D
Breast density ACR III. Preoperative situation on conventional 2D (Fig. 7.9a, b) in 2006 BI-RADS 4. Postoperative situation on conventional 2D (Fig. 7.10a, b) in 2008 BI-RADS 2; follow-up situation with digital 2D (Fig. 7.11a, b) in 2009 BI-RADS 2. 3D Lcc slices (Fig. 7.12a, b and Fig. 7.20 [3D magnification, same figure as 7.12a]) show additional architectural distortion in the medial part of the breast at 1–2 o’clock; BI-RADS 0/4.
Fig. 7.9
(a, b) 2D (a) obl and (b) cc in 2006
Fig. 7.10
(a, b) 2D (a) obl and (b) cc in 2008
Fig. 7.11
(a, b) 2D (a) obl and (b) cc in 2009
Fig. 7.12
(a, b) 3D slices cc (a) and (b) in 2009
Fig. 7.13
3D Magnification Rcc
Fig. 7.14
MRI in 2009
Differential Diagnosis on 2D
Typical imaging findings after breast-conserving therapy include lucent round oil cyst or fat necrosis, distortion of adjacent normal breast tissue, post-surgical scar, typical trabecular thickening, skin thickening, retraction, and dystrophic calcifications (BI-RADS 2).
Conclusion/Diagnosis with 3D
Additional suspicious changes outside the former tumor area in the medial part of the breast, diagnostic work-up required (BI-RADS 0/4).
Recommendation
US guided biosy or MRI.
US
No internal US.
Histology After US Guided Biopsy
Fat necrosis and scarred areas; B2.
Further Imaging/Further Diagnostic
In diagnostic uncertainty perform MRI and distinguish scar from recurrence, even fat necrosis can mimic recurrence; MRI in 2009 without signs of a relapse, fat necrosis at 11 and 1 o’clock (Fig. 7.14).
7.3 Case 3
General Information/Clinical Issues
Patient was a 58-year-old female; lumpectomy craniolateral left side in 1999.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree