Pneumonectomy
CRITICAL ELEMENTS
Patient Selection
Technical Aspects
Avoidance of Intra- and Postoperative Complications
1. PATIENT SELECTION
Recommendation: Proper preoperative evaluation with appropriate tests and imaging studies are essential to determine candidacy for pneumonectomy.
Type of Data: Retrospective.
Strength of Recommendation: Weak.
Rationale
Pneumonectomy is considered in patients who can physiologically tolerate the operation and whose disease cannot be cleared with lesser resections such as lobectomy, bilobectomy, or sleeve lobectomy. Patients for whom pneumonectomy is considered should first undergo careful evaluation to ensure that they can tolerate such an extensive lung resection. Preoperative pulmonary function tests, exercise testing, and room air arterial blood gas measurement, as well as imaging studies, can be used to assess a patient’s candidacy for pneumonectomy.1,2,3,4 In general, pneumonectomy is indicated for the resection of lung cancer that cannot be removed by lobectomy or sleeve resection. Examples include central tumors involving the main bronchus (Fig. 12-1) and central tumors that involve the proximal vasculature or interlobar vasculature or cross the fissure(s). Although many consider hilar lymph node involvement to be an indication for pneumonectomy, there is no survival advantage offered by pneumonectomy over sleeve lobectomy in this scenario.5
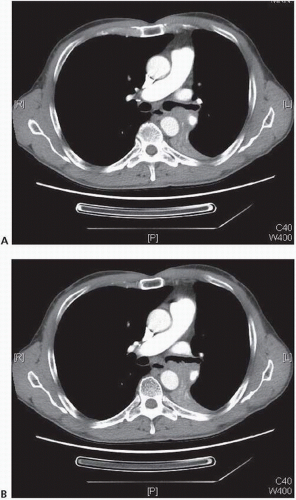 FIGURE 12-1 A,B: Axial CT images displaying proximal left main bronchus involvement by squamous cell cancer; left pneumonectomy was required for R0 resection. (Courtesy of Linda Martin, MD, MPH.) |
The role of pneumonectomy in patients with N2 disease (Fig. 12-2) is controversial. Several authors presenting single-institution series have reported no overall increase in perioperative morbidity and mortality among patients undergoing induction therapy followed by pneumonectomy.6,7,8 However, these same studies reported an increased incidence of postoperative morbidity and mortality for patients undergoing right pneumonectomy.6,7
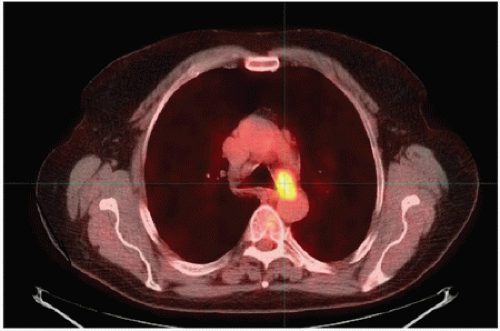 FIGURE 12-2 PET/CT image of malignant 4L lymph node, SUV of 4.9. “Confirmatory” endobronchial ultrasound biopsy of this node yielded squamous cell carcinoma. (Courtesy of Linda Martin, MD, MPH.) |
One randomized multicenter study found no difference in survival between patients with stage III disease who underwent induction chemoradiotherapy followed by pneumonectomy and those who underwent induction chemoradiotherapy followed by additional radiation therapy.9 However, these results were from an exploratory data analysis and not preplanned analyses. Another randomized trial of surgery versus radiotherapy in the setting of persistent N2 disease following induction chemotherapy failed to demonstrate any survival advantage for pneumonectomy patients.10 However, these results were also the products of exploratory analyses. Given findings earlier, pneumonectomy can be safely performed from a technical standpoint but does not appear to offer an oncologic advantage in patients with stage IIIA disease in the setting of persistent N2 disease following induction chemotherapy or chemoradiotherapy.
Preoperative Imaging
Preoperative imaging should be used to assist the surgeon with staging of the tumor. Positron emission tomography (PET)/computed tomography (CT) should be performed to rule out distant metastatic disease such as liver, adrenal, and bone metastases.11 For patients with proximal tumors, CT with intravenous contrast should be used to evaluate for tumor extension into vascular structures, including the pulmonary veins and main pulmonary artery. Tumor invasion into the proximal pulmonary vein may mandate intrapericardial dissection of the vessel at the time of surgery. Tumor invasion into the left atrium via the pulmonary vein indicates T4 disease. In some cases, cardiac magnetic resonance imaging (MRI) can be used to assess potential mediastinal or cardiac invasion if CT findings are equivocal. In addition, intraoperative transesophageal echocardiography can sometimes be helpful in assessing the degree of atrial involvement if visual inspection or palpation does not clearly demonstrate whether the tumor can be resected.
Bronchoscopic Evaluation of the Airway
Prior to or at the time of pneumonectomy, bronchoscopic evaluation of the airway is conducted. Although it should be performed before any kind of resection for lung cancer, this evaluation is especially important when pneumonectomy is being considered. The proximal location of the tumor in relation to both the mainstem bronchus and the carina should be noted to ensure that standard pneumonectomy is both necessary and feasible. In some patients with very proximal tumors, bronchoscopy may be optimally done on a date prior to the planned pneumonectomy to allow adequate time for pathologic analysis of bronchial and carinal biopsy samples to ensure that negative margins can be achieved with standard pneumonectomy. The surgeon should also take particular note of any anatomic abnormalities, such as a tracheal bronchus. Although they are uncommon,12,13 such anomalies may alter the operative plan.
Evaluation of the Mediastinum
Prior to any exploration of the pleural space, the mediastinal lymph nodes should be thoroughly evaluated. In a center with reliable on-site frozen pathologic evaluation services, mediastinoscopy may be performed at the time of pneumonectomy and may be advantageous in terms of avoiding scar tissue or immobility of the mediastinum and hilum due to mediastinoscopy in a separate setting. The specifics of mediastinal nodal evaluation are discussed elsewhere in the manual.
Pneumonectomy versus Sleeve Lobectomy
Although no prospective randomized studies comparing pneumonectomy to sleeve resection have been performed, several studies have compared both the short- and longterm outcomes between the two techniques. Recent studies, including meta-analyses, have demonstrated that the two techniques are associated with similar rates of perioperative morbidity; importantly, however, sleeve lobectomy is associated with a lower rate of perioperative mortality.14,15,16,17 From an oncologic perspective, the rates of locoregional recurrence in patients undergoing sleeve lobectomy are similar to those in patients undergoing pneumonectomy. However, patients undergoing sleeve lobectomy have higher rates of 5-year survival.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree