of their waking hours engaged in sedentary behaviors.7 Studies have shown a link between sedentary behaviors and increased rates of obesity, independent of the overall level of physical activity.8,9,10 Higher levels of sedentary behavior are also associated with greater risk for all-cause mortality, CVD, CVD mortality, T2D, and cancers of the colon, endometrium, and lung.1 Thus, both increasing physical activity and decreasing sedentary behavior are important for overall health. As illustrated in Figure 6.1, the risk of all-cause mortality is associated with both behaviors. To summarize this figure, individuals would benefit from making efforts to increase levels of MVPA as well as decreasing sitting time.
TABLE 6.1 Summary of Key Recommendations From the 2018 Physical Activity Guidelines for Americans | |||||
|---|---|---|---|---|---|
|
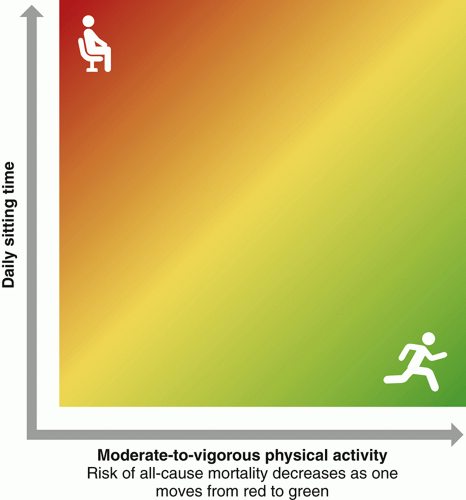 FIGURE 6.1 Relationship between moderate-to-vigorous physical activity (MVPA), sitting time, and risk of all-cause mortality in adults. Having high amounts of sitting time concomitantly with low amounts of MVPA is associated with the highest risk of all-cause mortality (indicated in red in upper left corner). As one increases MVPA, the risk associated with high amounts of sitting begins to decrease (indicated by orange color). Engaging in high amounts of MVPA is associated with lower risk of all-cause mortality even when combined with high amounts of sitting (indicated by green in the upper right corner). At the lowest levels of MVPA and the lowest levels of sitting time, there is still increased risk of all-cause mortality (indicated by orange in lower left corner). Risk of mortality increases with increased sitting. The highest levels of MVPA and lowest levels of sitting time are associated with the lowest risk of all-cause mortality (indicated by green in lower right corner). (Adapted from Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. U.S. Department of Health and Human Services; 2018. Adapted from data from Ekelund U, Steene-Johannessen J, Brown WJ, et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet. 2016;388(10051):1302-1310.) |
year.11 This annual weight gain places individuals at an increased risk for becoming overweight or obese with age. Physical activity has been postulated as a potential strategy for either attenuating or preventing this age-related weight gain. Several prospective, observational studies provide evidence that engaging in regular physical activity helps to prevent weight gain.12 Randomized trials have also examined the relationship between physical activity and weight gain with most studies suggesting that engaging in moderate-intensity physical activity is sufficient to prevent weight gain.12 In a study by Church et al., postmenopausal women who engaged in three different doses of supervised moderate-intensity aerobic activity (approximately 72, 136, and 194 minutes/week) over 6 months lost 3.0, 4.6, and 3.3 lb of body weight, respectively, compared with a 2 lb weight loss in the nonactive control group.13 In a similar study, McTiernan et al. found that men and women who participated in a facility-based and home-based physical activity program over 1 year lost 3.0 and 4.0 lb compared with 0.2 and 1.5 lb weight gain in nonactive controls.14 The combination of these studies and others suggest that a dose of approximately 150 to 250 minutes/week of moderate-intensity aerobic activity is effective for preventing weight gain and potentially eliciting modest weight loss.
TABLE 6.2 Physical Activity and Exercise Terminology | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
systematic review of studies lasting ≥12 months found that diet plus physical activity resulted in a mean weight loss of 8.8% compared with a weight loss of 6.9% from diet alone.19
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree