Summary of Key Points
- •
Discussed are tumor factors that affect treatment responses and outcome and host genetic elements that affect drug metabolism. Only pharmacogenomics elements that interact with chemotherapeutic agents are described.
- •
Prognostic biomarkers describe a specific tumor characteristic that allows for dichotomization of a cohort of patients into different groups based on an outcome that is independent of the treatment rendered.
- •
How biomarkers are measured and what is defined as positive or negative are crucial considerations pertinent to their use.
- •
At least 50% of patients with lung cancer have actionable driver mutations.
- •
Although the epidermal growth factor receptor (EGFR) signaling cascades are complex, tyrosine kinase in the EGFR intracellular domain is the key factor that triggers signaling.
- •
Anaplastic lymphoma kinase (ALK) activation occurs primarily via three different mechanisms: (1) fusion protein formation, (2) ALK overexpression, and (3) activating ALK point mutations.
- •
Crizotinib yields high response rates (exceeding 60%) and improves survival when used in patients with advanced nonsmall cell lung cancer who have ALK gene rearrangements and have progressed on previous therapy.
- •
The clinical uses of markers such as ERCC1 and RRM1 remain to be elucidated.
- •
KRAS mutational status is predictive of lack of therapeutic efficacy with EGFR tyrosine kinase inhibitors.
- •
MET and ROS1 genomic alterations are more rare driver mutations that, when detected, may enable more precise treatment for patients with lung cancer.
- •
Molecular biomarkers such as ERCC1 , RRM1 , BRCA1 , thymidylate synthase, and others remain investigational.
Effective treatment strategies for advanced stage lung cancer continue to be elusive despite substantial advances in the treatment of specific subsets of patients. Over the past decade, however, our understanding of the molecular mechanisms that underlie cellular transformation and the development of lung cancer has increased greatly. This knowledge has led to the development of therapeutic agents targeted against specific intracellular or extracellular targets presumed to be critical in the molecular pathways of carcinogenesis. For example, tyrosine kinase inhibitors, which have demonstrated increased efficacy and tolerability compared with chemotherapy in patients with metastatic lung cancer and epidermal growth factor receptor ( EGFR ) mutations or anaplastic lymphoma kinase ( ALK ) translocations, are now first-line treatment for patients with these tumor markers.
Host germline genetic variations can affect the pharmacokinetics and pharmacodynamics of individual drugs and thus affect patient outcomes. Thus, genetically determined pharmacokinetic variations may affect both the antitumor efficacy and host toxicities. In addition to genetic determinants in the host, environmental factors can affect the way drugs are metabolized, which in turn can affect their efficacy. In lung cancer, the primary example is smoking. Smoking is reported to alter the metabolism of several chemotherapeutic drugs and targeted agents, such as erlotinib. However, the extent of the effect smoking has on the pharmacokinetics of individual drugs may be determined by individual host genetics.
Researchers in the field of pharmacogenetics seek to gain a better understanding of the association between human/host genetics and drug response and toxicity. Advances in knowledge about tumor genomics, afforded by the genome-wide integrative analysis possible in the postgenomic era, when integrated with the field of pharmacogenetics, provide a modern basis for the field of pharmacogenomics. Thus, pharmacogenomic research is designed to determine host genetic variations, the genomic make-up of a tumor, the interaction between host genetic variations and tumor make-up, and the net effect on treatment responses and outcome. This chapter discusses tumor factors that affect treatment responses and outcome and host genetic elements that affect drug metabolism and its implications for routine clinical practice. As the title of the chapter indicates, only pharmacogenomics elements that interact with chemotherapeutic agents are described.
Tumor-Related Factors
Tumor-related molecular determinants are broadly divided into two categories: prognostic biomarkers and predictive biomarkers. Each of these characteristics of a molecular determinant can have therapeutic implications. A prognostic biomarker is an indicator of the innate aggressiveness of the tumor and is indicative of patient survival independent of treatment, whereas a predictive biomarker is an indicator of therapeutic efficacy. A prognostic biomarker describes a specific tumor characteristic that allows for the dichotomization of a cohort of patients into different groups based on outcome that is independent of the treatment rendered; for example, overall survival is better for patients with biomarker-positive tumors compared with patients with biomarker-negative tumors. Predictive biomarkers, on the other hand, suggest benefit or lack of benefit for a specific treatment based on the presence, absence, or overexpression or underexpression of the predictive biomarker, and thus, these biomarkers directly affect treatment decision-making. Some biomarkers may have both a prognostic and predictive function. Such so-called panoramic biomarkers make interpretation of data in different settings nuanced, and the dual prognostic-predictive value of the biomarker must be taken into account. Prototypic examples of biomarkers with both prognostic and predictive functions are excision repair cross-complementing 1 (ERCC1) and ribonucleotide reductase M1 (RRM1). In stage I and II nonsmall cell lung cancer (NSCLC), the prognostic function of ERCC1 and RRM1 may predominate, suggesting that overall survival will be better for patients with tumors positive for these markers after surgical resection than for patients with tumors negative for the markers. However, in stage IV NSCLC, the predictive function is most relevant, suggesting that tumors positive for ERCC1 or RRM1 will have inferior responses to cisplatin or gemcitabine, respectively, compared with cancers that are ERCC1- or RRM1-negative. Stage III NSCLC presents a challenge, as the dual function of ERCC1 and RRM1 makes interpretation of their significance difficult in a setting in which cisplatin is typically used, potentially in combination with other drugs such as paclitaxel, pemetrexed, or etoposide, as well as radiotherapy. It is unclear whether the prognostic function or the predictive function predominate or if a predominant function is relevant when additional treatment modalities are used. These issues have confounded and confused the interpretation of several studies done with these and other markers.
Measurement of Molecular Biomarkers
Another crucial consideration pertinent to the use of biomarkers, whether prognostic, predictive, or panoramic, is how they are measured and what is defined as positive or negative. For some biomarkers, it can be clearly discerned whether the marker is present or absent in the tumor; classic examples of this type of biomarker are mutations of the EGFR gene or translocations of the echinoderm microtubule-associated protein-like 4 ( EML4 ) and ALK genes. Because the molecular aberrations can be clearly and unambiguously measured, the effect of these mutations on patient outcomes is clear.
However, most biomarkers are present on a continuum in almost all tumors, and, as such, variations in measurement techniques and interpretation of values are more likely. Typically, a lower expression of these biomarkers is considered negative and a higher expression is considered positive. The challenge is that the level of expression corresponding to positive or negative is often arbitrary and, for ease of interpretation, the cutoff point is often the statistical median. This approach artificially renders a continuous variable into a discrete one, which potentially confounds the strength of the association being measured. The strength of the association may be particularly vulnerable around the median. Investigators have attempted to partially offset this problem by dichotomizing the results in a particular cohort into quartiles and examining the association between a marker and an outcome by comparing the highest quartile with the lowest quartile.
The measurement technique is crucial to successful incorporation of biomarkers into clinical decision-making. Discrete biomarkers (i.e., those that are either present or absent) are best measured at the DNA level. Mutations, translocations, and copy number gains fall into this category. Mutations and translocations are best measured by sequencing the gene of interest, preferably in its entirety, and this technique will identify common and rare mutations, as well as mutations that are as yet unidentified. Multiplexed polymerase chain reaction (PCR)-based techniques will identify common mutations but will only detect mutations for which the primers are included in the multiplex panel.
Nondiscrete biomarkers are best measured at the RNA or protein level. As an example, most epithelial tissue expresses the EGFR protein, with the expression higher in some tissues than in others. Increased EGFR expression is not a consequence of an abnormality of the EGFR gene at the DNA level but is most likely a consequence of increased transcription of the normal EGFR gene to RNA and then eventual translation of the RNA to protein. Thus, the increased expression of a particular gene may be measured at the RNA or the protein level.
Measurement at the RNA or protein level each is associated with advantages and disadvantages. Measurement at the RNA level is more technically complex and thus could be more challenging to accomplish in the routine clinical setting. The expression of a gene is measured relative to the expression of a housekeeping gene and expressed as a unitless ratio. The values derived also depend on the use of specific standardization techniques and procedures, which can vary from laboratory to laboratory. Because of this potential variation, numerically similar values may not be congruent across different laboratories and platforms. Additionally, the cutoff values for high versus low must be individually established for each laboratory and validated by clinical data. Nevertheless, measuring RNA through quantitative PCR, if done with proper controls and standardization procedures, is precise, reproducible, and quantifiable. Hence, despite the technical difficulties, quantitative PCR has been the favored approach by several investigators. Controversy also exists as to the optimal sample for quantitative PCR. Most investigators consider a fresh frozen sample to be ideal, but it is not practical to obtain fresh frozen biopsy specimens in the clinical setting, especially from patients with advanced NSCLC. However, most investigators now believe that good-quality mRNA can be extracted from formalin-fixed paraffin-embedded (FFPE) tissue, and thus, such samples can be used for quantitative PCR. However, the process used to make the FFPE samples may potentially alter the message, which raises questions about the relevance of quantitative PCR measurements in FFPE samples.
Immunohistochemistry (IHC) is most commonly used to measure protein levels in clinical samples. IHC has several advantages, including relative ease of use, widespread availability in most clinical pathology laboratories, and the capability of evaluating FFPE samples. The performance characteristics of IHC, however, are critically dependent on having a good antibody that effectively binds only to the antigen of interest. Additionally, the intensity of the staining is arbitrarily graded as 0 through 3 (0 = no staining, 1= weak staining, 2 = moderate staining, and 3 = strong staining) or by the H score (the H score is a product of staining intensity and the percent of cells stained; for example, if 50% of the slides show an intensity of more than 3, 20% show an intensity of more than 2, and 30% are negative, then the H score would be 150 + 40 = 190). Despite these scoring methods and the use of rigorous (positive and negative) controls, these techniques can still lead to variation in interpretation. The definition of positive is also arbitrary and if, for example, 2+ or higher is considered positive, the arbitrariness between a score of 1 or 2 thus jeopardizes the very definition of positive versus negative.
To partially counteract the arbitrary nature of IHC grading methods, the automated quantitative analysis of in situ protein expression (AQUA) method was developed. The AQUA method involves the use of fluorescent microscopic technology that measures the expression of proteins of interest by quantifying the intensity of antibody-conjugated fluorophores within a specific cellular compartment (such as the nucleus or cytoplasm) in a tumor. A quantitative score is thus generated based on the intensity of immunofluorescence. The AQUA method thus provides a more continuous scoring of protein expression in tissue samples. Even though the AQUA method eliminates some of the subjectivity in the interpretation of IHC, the method is still associated with some of the same challenges as IHC. For example, AQUA also depends on an antibody that binds only to the protein of interest and the cutoff point to define positive and negative is arbitrary.
Driver Mutations in Lung Adenocarcinomas
The recognition of EGFR and ALK oncogenes as predictive biomarkers in lung cancer has led an ongoing investigation to identify additional oncogenic drivers with predictive and prognostic importance. Certain subsets of NSCLC can now be further defined at a molecular level by driver mutations in multiple oncogenes that lead to constitutive activation of mutant signaling proteins, causing induction and sustaining tumorigenesis. Mutations can be detected in all NSCLC histologies, including adenocarcinoma, squamous cell carcinoma, and large cell carcinoma, and in current-, former-, and never-smokers (defined as individuals who smoked fewer than 100 cigarettes in a lifetime).
It is estimated that at least 50% of patients with lung cancer have actionable driver mutations. Actionable driver mutations are defined as molecular abnormalities with downstream effects that initiate or maintain the neoplastic process, which can be negated by agents directed against each genomic alteration. Some of the evidence of the driver mutations of significance in lung cancer comes from research conducted by the 14-member Lung Cancer Mutation Consortium (LCMC), which has investigated metastatic lung adenocarcinomas since 2009 to identify and study driver genomic alterations. Between 2009 and 2012 more than 1000 patients underwent genotyping to determine the frequency of oncogenic drivers in lung cancer and demonstrate the practicality of using routine genetic analyses to inform treatment with targeted therapies.
In the LCMC patient cohort actionable driver mutations were found in 64% of tumors from patients with lung adenocarcinomas. Table 47.1 lists the driver mutations the LCMC investigators identified. Most of these driver mutations were found in a small percentage of patients. The most common driver mutations detected were in the EGFR, KRAS, and ALK genes.
| Mutation | Incidence (%) |
|---|---|
| ALK rearrangements | 8 |
| BRAF | 2 |
| EGFR, sensitizing | 17 |
| EGFR, other | 4 |
| ERBB2, formerly HER2 | 3 |
| KRAS | 25 |
| MEK1 | <1 |
| MET amplification | <1 |
| NRAS | <1 |
| PIK3CA | <1 |
The ALK fusion oncogene and sensitizing EGFR mutations have become accepted predictive biomarkers in lung cancer. The National Comprehensive Cancer Network (NCCN) recommends genotyping for EGFR mutations and ALK rearrangements in its algorithm for patients with metastatic disease.
Epidermal Growth Factor Receptor
EGFR (also known as HER1) is a transmembrane receptor for the epidermal growth factor with intrinsic tyrosine kinase activity. It is encoded by a gene located on chromosome 7. EGFR belongs to a family of receptor tyrosine kinases, which upon activation result in stimulation of multiple downstream pathways within the cell, including those involved in cell survival, proliferation, and resistance to apoptosis.
In normal cells the tyrosine kinase activity of the EGFR is strictly regulated, and therefore cell growth is controlled. Although the EGFR signaling cascades are complex, tyrosine kinase in the EGFR intracellular domain is the key factor that triggers signaling. If tyrosine kinase activity is blocked (i.e., via a molecular targeted agent), EGFR is unable to transduce signals to the cell nucleus. In cancer cells, various mechanisms of EGFR activation have been identified, including receptor overexpression, ligand overexpression, and EGFR gene amplification.
EGFR Overexpression
EGFR expression refers to measurement of levels of receptor protein (either normal [wild-type] protein or abnormal [meaning from the mutated gene]) by IHC and is distinct from detection of an actual EGFR mutation. EGFR expression is detectable in approximately 80% to 85% of patients with NSCLC, although the levels of expression vary widely on a continual scale.
Approximately 40% to 80% of NSCLC tumors overexpress EGFR. This wide range in the frequency of EGFR overexpression may be due to differences in the techniques used to determine EGFR overexpression, the criteria used to define overexpression levels, and the differences in study populations. Wild-type is the term used to describe EGFR that is overexpressed but not mutated. The result of overexpression is an overabundance of receptors that are available to interact with ligands. Wild-type EGFR becomes activated by binding to ligands. Ligand binding induces receptor dimerization, and the ligand-bound EGFR activates tyrosine kinase-mediated signaling pathways, leading to tumor proliferation, survival, and resistance to apoptosis.
Tumor cells can overexpress EGFR as well as its ligands. Ligand overexpression increases EGFR dimerization, activation, and tyrosine kinase-mediated signaling, which can lead to uncontrolled tumor growth.
EGFR overexpression is more common in squamous cell carcinoma and adenocarcinoma, and to a lesser extent in large-cell carcinoma. Although the clinical significance of overexpression in NSCLC remains controversial, some investigators have found that overexpression of EGFR is associated with more aggressive tumors, a poor clinical prognosis, and, in certain tumor types, the development of resistance to radiation and cytoxic agents.
Among patients with NSCLC, wild-type EGFR is more common than mutated EGFR. Compared with mutated EGFR, patients who harbor wild-type EGFR show reduced benefit for EGFR tyrosine kinase inhibitors such as erlotinib and gefitinib. This may be because the wild-type EGFR typically sends a downstream signal that ultimately stimulates the growth of tumor cells that are dependent on the receptor, and gefitinib or erlotinib can modestly inhibit this relatively weak signal. In contrast, the mutated EGFR is constitutively activated with a prominent downstream signal that can be dramatically inhibited by gefitinib and erlotinib.
EGFR Mutations
Somatic mutations of EGFR genes can result in the production of mutated receptors. About 10% to 15% of Caucasian patients with NSCLC and 30% to 40% of Asian patients have tumor-associated EGFR mutations. These mutations occur within EGFR exons, which encode a portion of the EGFR kinase domain. The majority (about 90%) of these mutations are exon 19 deletions or exon 21L858R point mutations. Regardless of ethnicity, EGFR mutations are more often found in tumors from women, never-smokers (defined as less than 100 cigarettes in a patient’s lifetime), or former-smokers with adenocarcinoma histology.
Mutant EGFR does not require a ligand for receptor dimerization and activation. Thus, EGFRs that harbor mutations remain constitutively activated without ligand binding. Although the mutated receptor needs no growth factor for signaling, ligand binding increases receptor activity. Cancer cells harboring EGFR gene mutations often become highly dependent on the EGFR pathway, a state referred to as “oncogene addiction.”
There are several consequences of EGFR mutations, including: (1) constitutive activation of the EGFR tyrosine kinase activity and resulting hyperactivation of downstream targets; (2) diminished affinity for ATP; (3) increased sensitivity to tyrosine kinase inhibitors; or, conversely, (4) development of resistance to tyrosine kinase inhibitors for certain types of mutations.
EGFR-activating mutations are found to be favorable prognostic markers of survival and predictive markers of response in terms of tumor shrinkage. EGFR mutation status correlates strongly with the probability of response to an EGFR tyrosine kinase inhibitor, as well as a more favorable prognosis in patients with advanced lung adenocarcinoma.
This association between EGFR-activating mutations and increased clinical responses seen with EGFR tyrosine kinase inhibitors has been investigated in multiple clinical studies. Evidence shows that the growth and downstream signaling inhibition of cells with EGFR-activating mutations is consistently more sensitive to treatment with EGFR tyrosine kinase inhibitors than the signaling in cells with wild-type EGFR. Moreover, EGFR tyrosine kinase inhibitors bind with higher affinity to the mutant receptors compared with the wild-type receptor.
The randomized, phase, open-label Iressa Pan-Asia Study marked a seminal moment in the treatment of patients with EGFR-activating mutations. In this study of previously untreated patients with NSCLC, a significant interaction was found between treatment and EGFR gene mutation with respect to progression-free survival. In the subset of 261 patients with EGFR gene mutations, progression-free survival was significantly longer among patients receiving the tyrosine kinase inhibitor gefitinib than among those receiving chemotherapy (hazard ratio [HR] for progression or death, 0.48; 95% CI, 0.36–0.64; p < 0.001). Conversely, in the subgroup of 176 patients who were negative for the mutation, progression-free survival was significantly longer among those who received carboplatin–paclitaxel (HR for progression or death with gefitinib, 2.85; 95% CI, 2.05–3.98; p < 0.001).
Even though patients with lung cancer harboring EGFR gene mutations generally exhibit a favorable response to EGFR tyrosine kinase inhibitors, certain EGFR gene mutations are associated with resistance to tyrosine kinase inhibitors. The T790M mutation, which results in a substitution of methionine for threonine at position 790 of the EGFR tyrosine kinase domain, leads to biochemical and structural alteration that causes resistance to therapy with a tyrosine kinase inhibitor. The T790M mutation has been reported in about 60% of patients with disease progression after initial response to erlotinib, gefitinib, or afatinib. The T790M mutation also has been identified as an oncogenic mutation, promoting oncogenesis especially when the T790M mutation occurs in combination with other EGFR-activating mutations.
Other, less-common EGFR gene mutations (approximately 10%) located in the kinase domain that may have significance with regard to sensitivity and resistance to EGFR tyrosine kinase inhibitors have been identified ( Table 47.2 ).
| Mutation | Frequency (%) | Clinical Significance |
|---|---|---|
| Exon 21 mutation (L861X a ) | 2 | TKI sensitivity |
| Exon 18 mutation (G719X) | 3 | TKI sensitivity |
| Exon 19 insertion | 1 | TKI sensitivity |
| Exon 20 insertion | 4–9 | TKI resistance |
a The “X” is used to designate that several amino acid substitutions are possible at the site.
Anaplastic Lymphoma Kinase
The ALK gene encodes a tyrosine kinase receptor that is normally expressed in central and peripheral nervous systems, testes, skeletal muscle, basal layer keratinocytes, and the small intestine. ALK appears to function in neuronal development and differentiation during embyrogenesis and its expression falls to low levels at age three weeks and remains low throughout adult life.
ALK activation occurs primarily via three different mechanisms: (1) fusion protein formation, (2) ALK overexpression, and (3) activating ALK point mutations. In ALK translocations, the fusion partner regulates ALK expression levels, its subcellular location, and when it is expressed. Multiple different ALK gene rearrangements have been described in NSCLC. The majority of these ALK fusion variants are comprised of portions of the echinoderm microtubule-associated protein-like 4 ( EML4 ) gene. Dimerization of the ALK fusion product, which is mediated by the fusion partner, results in constitutive activation of the ALK tyrosine kinase. Signaling downstream of ALK fusions results in activation of cellular pathways known to be involved in cell growth and cell proliferation. An estimated 2% to 7% of patients with NSCLC have ALK gene rearrangements.
ALK gene rearrangements tend to occur mutually exclusive of EGFR mutations. Thus, the presence of ALK gene rearrangements is associated with resistance to EGFR tyrosine kinase inhibitors. Patients with ALK gene rearrangements have similar clinical characteristics to those with EGFR mutations (including adenocarcinoma histology and nonsmoking or light smoking histories) except they are more likely to be men and may be younger. Rarely are ALK gene rearrangements detected in patients with squamous cell carcinoma.
Crizotinib is a dual ALK/MET tyrosine kinase inhibitor approved for ALK-positive and ROS1-positive NSCLC. Crizotinib has been shown to yield very high response rates (exceeding 60%) and improve survival when used in patients with advanced NSCLC who have ALK gene rearrangements and have progressed on previous therapy, including those with brain metastases. The NCCN recommends crizotinib for first-line and subsequent therapy in patients with ALK-positive NSCLC. Ceritinib and alectinib are newer ALK inhibitors recommended for use in patients who progress on crizotinib or are intolerant of crizotinib.
KRAS
RAS binding proteins, including KRAS, are central mediators downstream of growth factor receptor signaling. In its mutated form, KRAS is constitutively active, able to transform immortalized cells and promote cell proliferation and survival.
KRAS gene mutations are detected in tumors from former-, current-, and never-smokers, although they are rarer in never-smokers. Approximately 25% of patients with lung adenocarcinoma in North America have KRAS mutations, making KRAS the most common mutation. The exact role of KRAS as a predictive or prognostic biomarker in metastatic lung cancer remains undetermined as few prospective trials have examined the utility of using KRAS mutational status to inform treatment with targeted agents. Nevertheless, KRAS gene mutations are predictive of lack of therapeutic efficacy with tyrosine kinase inhibitors that target EGFR, such as erlotinib and gefitinib. Moreover, patients with KRAS gene mutations appear to have a shorter survival than patients with wild-type KRAS. EGFR and KRAS mutations appear to occur mutually exclusive of each other.
MET
The MET gene encodes a receptor tyrosine kinase, which becomes activated upon binding of its ligand, hepatocyte growth factor. Consequently multiple downstream pathways within the cell become activated, including those involved in cell survival and proliferation. In cancer, aberrant signaling through the MET receptor promotes pleiotropic effects, including growth, survival, invasion, migration, angiogenesis, and metastasis.
In NSCLC, multiple mechanisms of MET activation have been reported, including both gene amplification and mutation. Overexpression of MET protein in tumor tissue relative to adjacent normal tissues occurs in 25% to 75% of NSCLC and is associated with a poor prognosis. Data suggest MET protein expression and activation predict poor response to subsequent treatment with EGFR tyrosine kinase inhibitors, despite the presence of tyrosine kinase inhibitor–sensitizing mutations within the EGFR gene.
ROS1
ROS1 is a receptor tyrosine kinase of the insulin receptor family that is involved in chromosomal translocations in lung cancer. ROS1 fusions, which have been found to be potential driver mutations in a NSCLC cell line, lead to constitutive kinase activity and are associated with sensitivity in vitro to tyrosine kinase inhibitors. Signaling downstream of ROS1 fusions results in activation of cellular pathways known to be involved in cell growth and cell proliferation. Approximately 2% of NSCLC tumors harbor alterations in the ROS1 gene. Patients positive for a ROS1 rearrangement have a typical clinical profile, including young age at onset and nonsmoking history. ROS1 fusions are associated with sensitivity to tyrosine kinase inhibitors that have “off-target” activity against ROS1; an example of this is crizotinib.
ERCC1 and RRM1
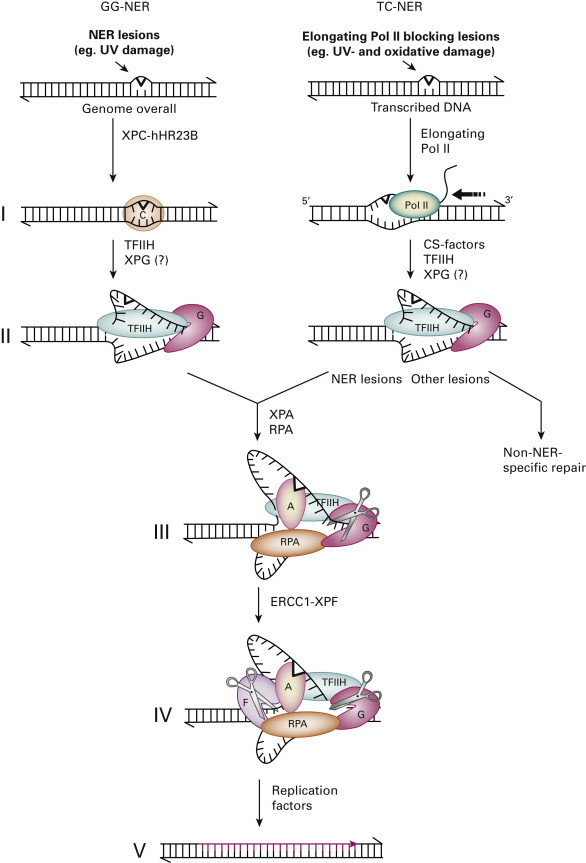
Cisplatin-based chemotherapy is the standard of care for all patients with advanced stage NSCLC and is also used as adjuvant treatment for patients with completely resected stage II and III NSCLC. Cisplatin impedes DNA replication by establishing DNA-platinum adducts. Breaks in the DNA strand occur when the DNA unwinds in anticipation of initiation of replication. ERCC1 belongs to the nucleotide excision repair (NER) family of proteins and is involved in the repair of these DNA strand breaks. The ERCC1 protein works with its partner protein xeroderma pigmentosum complementation group F (XPF) in the final step of the NER pathway that recognizes and removes cisplatin-induced DNA adducts, allowing the tumor DNA replication to continue. The NER pathway-mediated removal of platinum DNA reverses the tumoral DNA damage induced by cisplatin, thereby leading to cisplatin resistance ( Fig. 47.1 ). High expression of ERCC1 in the tumor thus predicts for cisplatin resistance and serves as a predictive molecular determinant for the efficacy of this chemotherapy agent.
The nature-envisioned purpose of ERCC1 is to effect DNA repair when DNA damage occurs after exposure to natural DNA-damaging entities, such as ionizing radiation and mutagenic compounds. A relatively preserved DNA repair mechanism, as suggested by high nuclear ERCC1 expression, therefore preserves genomic integrity. High tumoral levels of ERCC1 have therefore been associated with better outcomes in patients with early-stage disease who have had curative resection, presumably because of more indolent tumor behavior secondary to a relatively preserved genomic integrity. ERCC1 thus functions as a prognostic marker in patients with early-stage NSCLC.
RRM1 is the regulatory component of ribonucleotide reductase and is a nonredundant component of DNA synthesis. Its primary function is to generate nucleotides that can be used for DNA synthesis and repair. It is also the principal target of the commonly used cytotoxic agent, gemcitabine, and hence, high RRM1 levels predict for resistance to gemcitabine. Analogous to ERCC1, RRM1 has been associated with different survival outcomes in patients with NSCLC, with higher RRM1 levels predicting for a better prognosis and improved survival. In preclinical trials, increased RRM1 expression was shown to be associated with decreased invasion and migration and with an overall more indolent behavior. It is not entirely clear how RRM1 causes these effects, but it has been postulated that the effects are perhaps mediated through a direct correlation between RRM1 and expression of phosphatase and tensin homolog protein. RRM1 therefore has both a predictive and prognostic function.
The prognostic function of ERCC1 was first noted in a retrospective analysis of patients with NSCLC who had curative resection. ERCC1 was measured using reverse transcription (RT)-PCR, and its expression was normalized using 18SrRNA (a commonly used housekeeping gene) expression; therefore its levels were expressed as a unitless ratio. Using an ERCC1 value of 50 to dichotomize the cohort, researchers noted a significant difference in median survival for patients with ERCC1 expression of more than 50 in the tumor compared with patients with ERCC1 expression of less than 50 in the tumor (94.6 vs. 35.5 months; p = 0.01). In multivariate analysis, high ERCC1 expression was found to be an independent predictor of better prognosis.
Olaussen et al. further analyzed the prognostic value of ERCC1 in specimens obtained from the International Adjuvant Lung Trial (IALT). In the IALT study, patients with curatively resected NSCLC had been randomly assigned to receive adjuvant chemotherapy or no further therapy, as was the standard of care at that time. In the overall study population, adjuvant chemotherapy had improved 5-year survival by 4.1% ( p < 0.03). Olaussen et al. used IHC to analyze the tumor samples in that study for expression of ERCC1 (in addition to other markers) using an antibody that was then believed to stain for ERCC1 (murine antibody from clone 8F1; Neomarkers Inc, Fremont, CA, USA). Among patients with ERCC1-negative tumors, the 5-year overall survival rate was significantly longer for patients who received chemotherapy (47% vs. 39%; p = 0.002). However, among patients with ERCC1-positive tumors, overall survival did not differ between patients who received adjuvant chemotherapy and patients who did not. Of note, among patients who did not receive adjuvant chemotherapy, overall survival was significantly better for patients with ERCC1-positive tumors than for patients with ERCC1-negative tumors (adjusted HR for death, 0.66; 95% CI, 0.49–0.90; p = 0.009). This finding suggests an intrinsic prognostic function for ERCC1.
Given these results, the authors conducted a comprehensive analysis to compare various methods to measure ERCC1, as well as several antibodies used to measure ERCC1 by IHC. They obtained 494 tumor specimens from two independent phase III trials (the National Cancer Institute of Canada Clinical Trials Group JBR.10 and the Cancer and Leukemia Group B 9633 trial from the Lung Adjuvant Cisplatin Evaluation Biology project). The researchers also repeated the staining of all 589 specimens in the original set of samples from the IALT study. They mapped the epitope recognized by 16 commercially available ERCC1 antibodies and investigated the capacity of the different ERCC1 isoforms to repair platinum-induced DNA damage. The investigators noted that ERCC1 was positive in 77% of the samples in the current study compared with 44% of the samples in the IALT study. Additionally, ERCC1 was no longer a predictive biomarker of the efficacy of chemotherapy ( p = 0.53 for interaction). The 8F1 antibody used in the current study was different from that used in the initial analysis, and they concluded that there was a shift in the activity of the 8F1 antibody. Unfortunately the 8F1 antibody used in the IALT study had been totally consumed and was therefore not available for comparison.
Another significant finding was that each of the 16 antibodies tested could detect all of the four known isoforms of ERCC1. Because the epitopes are common in these four isoforms (201, 202, 203, and 204), none of the currently available antibodies could distinguish between them. For the purposes of RT-PCR, separate primers can be made for ERCC1 isomers 201 and 203; however, because of substantial homology, primers cannot be separately made against 202 and 204. Thus, these two polymorphisms were measured in unison and there was no detectable difference in ERCC1-positive or ERCC1-negative samples in terms of overall or progression-free survival. However, in cell line experiments only the ERCC1 202 polymorphism seemed to predict for resistance to cisplatin; thus, this polymorphism may be the functional one. The authors concluded that measuring the clinically relevant functional ERCC1 202 polymorphism may be the better predictor of benefit for cisplatin in patients with NSCLC. Measuring the specific ERCC1 202 polymorphism will, however, be challenging because the high percentage of sequence homology among the four protein isoforms makes the generation of an ERCC1 202-specific antibody technically difficult. Making ERCC1 202-specific primers is onerous for the same reason. However, the ERCC1 202 polymorphism may be detectable by sequencing at the DNA level, which would convert this nondiscrete biomarker into a discrete one.
To study the association between ERCC1 and RRM1, Zheng et al. estimated the expression of ERCC1 and RRM1 at the protein level by AQUA and at the RNA level by RT-PCR and correlated the findings with survival. RRM1 expression was directly correlated with ERCC1 expression. Furthermore, patients who had tumors with high expression of RRM1 also had superior survival compared with patients who had tumors with low expression of RRM1 (disease-free survival, more than 120 vs. 54.5 months; HR, 0.46; p = 0.004; and overall survival, more than 120 vs. 60.2 months; HR, 0.61; p = 0.02). Other investigators also showed that patients who had tumors with high expression of both biomarkers had superior overall survival compared with patients who had tumors with low expression of either one of the biomarkers or both.
The Southwest Oncology Group conducted a trial to assess the feasibility of selecting treatment based on in situ tumor levels of ERCC1 and RRM1 in a cooperative group setting. Patients with stage I lung cancer were enrolled. ERCC1 and RRM1 expression were determined at the protein level with use of AQUA (range of expression, 1–255), and the level was classified as high or low based on previously established cutoff values of 65.0 for ERCC1 and 40.0 for RRM1. The treatment regimen consisted of cisplatin and gemcitabine (80 mg/m 2 on day 1 and 1 g/m 2 on days 1 and 8) for patients who had tumors with a low level of ERCC1 or RRM1 or both. Patients who had tumors with a high level of ERCC1 or RRM1 were followed up with observation, which is essentially the standard of care. In the protocol, feasibility was defined as the assignment of treatment within 12 weeks after surgery in at least 75% of the enrolled patients. Eighty-five patients were accrued between March 2009 and April 2011. ERCC1 and RRM1 levels were successfully determined in 83 patients, and 72 patients (87%) were successfully assigned appropriate therapy within the 12-week time frame. Of the 83 patients, 64 (77%) were assigned to chemotherapy and 19 (23%) to observation. ERCC1 levels ranged from 4.3 to 211.2 (median, 44.7), and RRM1 levels ranged from 2.5 to 234.4 (median, 39.3). The authors therefore concluded that assignment of chemotherapy was feasible in a multi-institutional cooperative group setting.
In the advanced stage NSCLC setting, Rosell et al. analyzed samples from 100 patients to evaluate the association between expression of ERCC1 and RRM1 and survival. Patients in the study were treated with either gemcitabine and cisplatin; gemcitabine, cisplatin, and vinorelbine; or gemcitabine and vinorelbine followed by vinorelbine and ifosfamide. ERCC1 and RRM1 expression at the mRNA level was determined by RT-PCR in FFPE samples that had been obtained bronchoscopically. Again, a strong correlation between the expression of ERCC1 and RRM1 was noted ( p < 0.001). Among patients treated with gemcitabine and cisplatin, the median survival was significantly longer for patients who had tumors with low RRM1 mRNA expression than for patients who had tumors with high RRM1 mRNA expression (13.7 vs. 3.6 months; p = 0.009). In addition, the median survival was significantly longer for patients who had tumors with low expression of RRM1 and ERCC1 than among patients who had high levels of both genes ( p = 0.016). These results essentially corroborated the earlier findings by the same group in a smaller cohort of patients in which ERCC1 mRNA expression was significantly associated with response to cisplatin and gemcitabine in patients with advanced stage NSCLC.
The Genomic International Lung Trial (GILT) was the first prospective randomized trial designed to show clinical benefit of customizing chemotherapy. In this phase III trial, 444 patients with previously untreated advanced NSCLC were randomly assigned in a 1:2 ratio to either a control arm of docetaxel and cisplatin or a genotypic arm in which treatment was assigned based on the level of ERCC1 mRNA expression in the tumor, as measured by RT-PCR. In the genotypic arm, patients received docetaxel and cisplatin if their tumors expressed ERCC1 mRNA levels lower than the median or received docetaxel and gemcitabine if the tumors expressed ERCC1 mRNA levels higher than the median. The study reached its primary end point of response, with a significantly better response rate in the genotypic arm than in the control arm (51.2% vs. 39.3%; p = 0.02). In multivariate analysis, low ERCC1 expression was an independent predictor of tumor response to cisplatin. The study was not powered to show survival differences, but neither progression-free survival nor overall survival was significantly different between the control and genotypic arms; the median progression-free survival was 6.1 months for the genotypic arm compared with 5.2 months for the control arm (HR, 0.9; p = 0.30), and the median overall survival was 9.9 months compared with 9.8 months for the genotypic and control arms, respectively (HR, 0.9; p = 0.59). Within the genotypic arm, relatively similar response rates were noted for patients with ERCC1-negative tumors treated with docetaxel and cisplatin (53%) and patients with ERCC1-positive tumors treated with docetaxel and gemcitabine (47%), with a median progression-free survival of 6.7 and 4.7 months, respectively, and a median overall survival of 10.3 and 9.4 months, respectively. In retrospect, given that expression of ERCC1 and RRM1 correlates with each other, a fact that was not known to the investigators at the time GILT was designed, cisplatin and gemcitabine would have been optimal treatment for patients who had tumors with low ERCC1 expression, and docetaxel with vinorelbine (rather than gemcitabine) would possibly be more desirable for patients who had tumors with high ERCC1 expression (because the presence of high ERCC1 expression suggests concomitant high expression of RRM1 and high RRM1 expression predicts for resistance to gemcitabine). The reason for the strong correlation between high ERCC1 and RRM1 expression is not clear but it is postulated that a steady supply of nucleotides, which are generated by RRM1, is necessary for efficient repair, which is carried out by ERCC1.
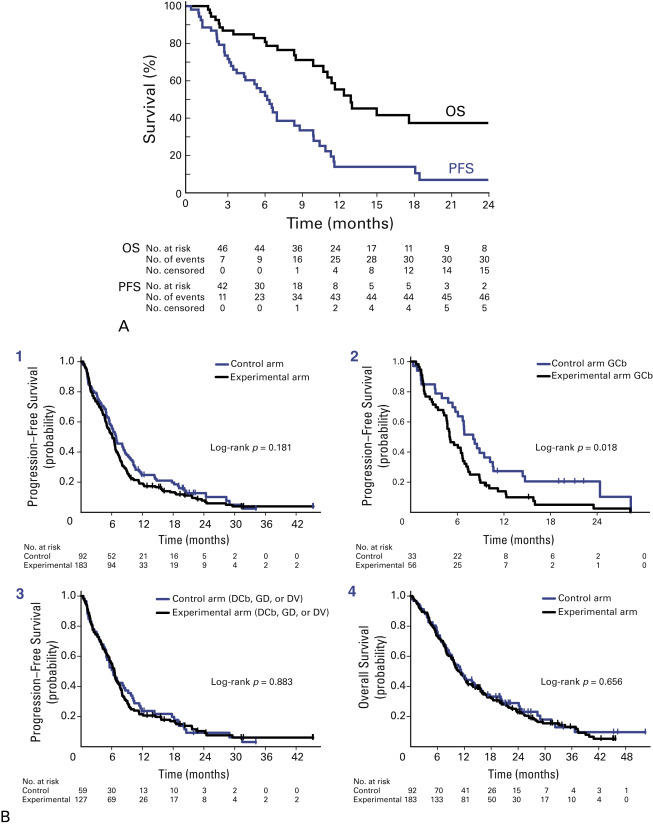
In an attempt to accelerate the application of this research to clinical practice, a prospective phase II trial, Molecular Analysis-Directed Individualized Therapy (MADe IT), assigned combination chemotherapy according to expression of ERCC1 and RRM1 (as measured by RT-PCR), with a primary end point of feasibility. Patients who had tumors with low ERCC1 expression were treated with carboplatin, and patients who had tumors with low RRM1 expression were treated with gemcitabine; patients who had tumors with high expression of either marker were treated with docetaxel. Therefore, based on the expression of ERCC1 and RRM1, patients could be assigned to one of four treatment groups: gemcitabine and carboplatin (low expression of both RRM1 and ERCC); gemcitabine and docetaxel (low RRM1 expression and high ERCC1 expression); docetaxel and carboplatin (high RRM1 expression and low ERCC1 expression); or docetaxel and vinorelbine (high expression of both RRM1 and ERCC1). The response rate was 44%, with an overall survival of 13.3 months and a progression-free survival of 6.6 months ( Fig. 47.2 ).