Types
Subtypes
Percentage
Malignant
Epithelial
75
Tubulopapillary nonglandular (solid)
13
Sarcomatous
6
Biphasic (mixed)
6
Undifferentiated
Very rare
Desmoplastic
Very rare
Lymphohistiocytic
Very rare
Small cell
Very rare
Deciduoid
Very rare
Borderline/low malignant
Well-differentiated papillary
Rare
Multicystic
Rare
Sarcomatoid DMPM can show the histologic patterns produced by any softtissue tumor. A mixture of sarcomatoid and epithelial components gives rise to biphasic or mixed variants (Fig. 17.1), which are usually aggressive tumors. Occasionally, sarcomatous areas may be markedly hypocellular, resulting in small biopsy specimens being misinterpreted as reactive fibrosis [17, 18].
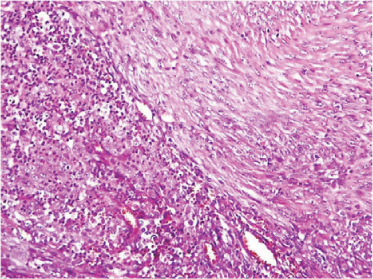
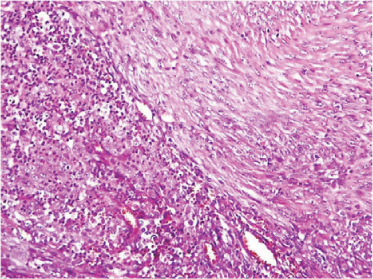
Fig. 17.1
Biphasic diffuse malignant peritoneal mesothelioma (DMPM) histology: combination of an epithelial and a sarcomatoid cells
It must be emphasized that conventional pathological techniques have low sensitivity and specificity in the diagnosis of DMPM. Thus, misdiagnosis between neoplasms originating from other abdominal organs is relatively common. Therefore, immunohistochemical studies play an important role in the diagnostic workup. In particular, DMPM must be distinguished from benign reactive lesions and metastatic carcinoma. At present, a specific marker for mesothelioma is not available, and diagnosis relies on the combination of positive [calretinin, cytokeratin (CK)-5/6, monoclonal antibody (MAb) D2-40, podoplanin, mesothelin, and Wilms tumor-1 (WT1)] and negative [claudin-4, carcinoembryonic antigen (CEA), MAbs MOC-31 and B72.3, and antihuman epithelial antigen (Ber-EP4) markers [17].
Thyroid transcription factor 1 (TTF-1) can assist in distinguishing DMPM from lung carcinoma, homeobox protein CDX-2 from colon carcinoma, and cytokeratin (CK)-7 and paired-box (PAX)-8 from ovarian carcinoma or serous papillary peritoneal carcinoma. Renal cell carcinoma marker (RCC-Ma) may be helpful in establishing renal origin [19, 20].
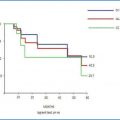
Gathering data from eight international centers, a new tumor/node/metastasis (TNM) staging system for DMPM was recently proposed. Peritoneal cancer index (PCI) was categorized into T1 (PCI 1ȃ10), T2 (PCI 11–20), T3 (PCI 21–30), and T4 (PCI 30–39). T1 N0 M0 was defined as stage I, T2/T3 N0 M0 as stage II, and T4 and/or N1 and/or M1 as stage III. The 5-year survival associated with stage I, II, and III disease was 87 %, 53 %, and 29 %, respectively [21].
17.4.3 Serum Tumor Markers
Although mesothelin and osteopontin showed their potential usefulness in diagnosing and assessing prognosis of pleura mesothelioma patients, no information is available for DMPM [22]. The clinical role of serum markers was studied in 60 patients with DMPM treated at the Istituto Nazionale Tumori (INT) in Milan, Italy. Baseline diagnostic sensitivity was 53.3 % for cancer antigen (CA)125, 0 for CEA, 3.8 % for CA19.9, and 48.5 % for CA15.3 [23]. These data may help in the initial evaluation of peritoneal tumors from unknown site of origin. When therapy response was assessed, CA125 normalized after adequate CRS plus HIPEC in 21/22 patients with elevated baseline levels. CA125 remained high in all patients with persistent macroscopic disease after surgery. Also, CA125 became positive in 12/12 patients with elevated baseline levels, developing disease progression after adequate CRS plus HIPEC. A borderline prognostic significance for baseline CA125 levels was observed only in individuals not previously treated with systemic chemotherapy (sCHT).
17.5 Treatment Results
17.5.1 Systemic Chemotherapy
In our institution, we investigated the role of sCHT in 116 DMPM patients treated with CRS plus HIPEC. No significant survival difference was seen among three subsets of patients: (1) those treated by sCHT before CRS plus HIPEC (n = 60), (2) patients who had sCHT after CRS plus HIPEC (n=30), and (3) the group receiving no sCHT (n = 26). However, administration of platinum compounds plus pemetrexed was related with a statistically significant borderline survival advantage (p = 0.09) [24]. Even looking at other centers’ experiences, no high-quality clinical data to define the role of sCHT in DMPM management is available.
DMPM is a poorly chemoresponsive tumor. A systematic meta-analysis of all prospective clinical trials published up to 2001 involving pleural or peritoneal mesothelioma demonstrated that cisplatin was the most active single agent and that cisplatin with doxorubicin was the most active combination in terms of treatment response [25]. However, these results should be interpreted with caution, as comparisons were not made in a randomized framework.
In a German series and the pemetrexed expanded access program, DMPM response rates were comparable with those observed for pleural disease [26, 27]. Other agents showing activity in DMPM are vinorelbine and gemcitabine, either alone or combined with platinum compounds. In historical case series, standard therapy with palliative surgery and systemic/intraperitoneally administered chemotherapy (IP-CHT) was associated with a median survival of ∼ 1 year [4]. However, the hypothesis that chemotherapeutic drugs have limited efficacy seems to be confirmed by the poor median survival, ranging from 9 to 15 months, observed in individuals affected by DMPM who receive sCHT alone [2].
17.5.2 Cytoreductive Surgery plus Hyperthermic Intraperitoneal Chemotherapy
The 2006 Milan Consensus Conference on Peritoneal Surface Malignancies concluded that the standard treatment of DMPM is based on the integration of CRSHIPEC and sCHT [6].
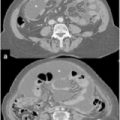
The aim of CRS is complete removal of all neoplastic implants from the abdominal cavity, which is possible only by peritonectomy (PRT) procedures and multivisceral resections. The pattern of DMPM dissemination implies complete distribution on peritoneal surfaces, and most cases are diagnosed with widespread tumor (Fig. 17.2). Also, microscopic disease is frequently identified at pathological examination, even when no evidence of disease is noted at macroscopic intraoperative examination. Therefore, we recommend complete parietal PRT for this disease [28]. Conversely, organ resections are indicated only in case of their massive involvement.


Fig. 17.2
Intraoperative high Peritoneal Cancer Index (PCI) in diffuse malignant peritoneal mesothelioma (DMPM): typical omental cake, peritoneal thickening, abdominal mass, and mesenterial thickening
With the aim of consolidating macroscopic CRS, locoregional treatment allowing high peritoneal (and low systemic) drug concentration is used. This procedure, HIPEC, combines the pharmacological advantage with moderate hyperthermia. CRS is performed according to the technique originally described by Sugarbaker, with minor variations [29, 30] (Fig. 17.3) HIPEC is performed according to the closed-abdomen technique with cisplatin (45 mg/L perfusate) and doxorubicin (15 mg/L perfusate) for 90 min at a temperature of 42.5 C, based on a recent dose-finding study [31]. Perfusate volume is 4–6 L, and mean flow is 700 ml/min. The extracorporeal circulation device, Performer LRT® (RAND, Medolla, Italy), is used.
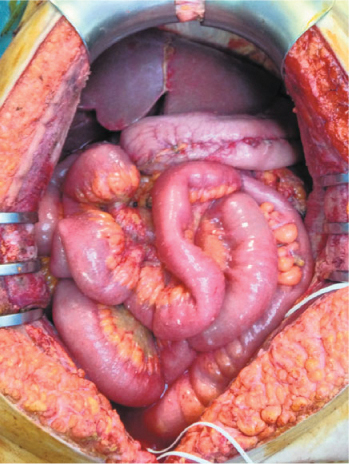
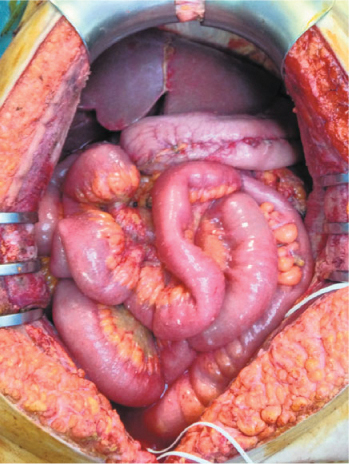
Fig. 17.3
High Peritoneal Cancer Index (PCI) diffuse malignant peritoneal mesothelioma (DMPM): result after mesenteric peritonectomy
Analysis of published data allows us to conclude that median survival grew from 12 months with sCHT to 53 months with CRS plus HIPEC plus sCHT [32–34]. In our institutional experience, postoperative quality of life (QoL) was satisfactory, related morbidity and mortality acceptable, and financial cost-effectiveness reasonable [35, 36].
According to our most recent study, median overall (OS) and progression-free (PFS) survival were 63.2 and 25.1 months in 108 patients undergoing complete CRS plus HIPEC (residual tumor < 2.5 mm). The survival curve reached a plateau after 7 years, suggesting that patients surviving > 7 years may be cured. Actual cure rate was 19/39 patients with potential follow-up of 7 years (43.6 %) [37].
17.6 Prognostic Factors
In a large collaborative study, the most significant prognostic factors were epithelial subtype, no node metastases, completeness of cytoreduction (CC), and administration of HIPEC [33]. In pattern-of-failure analysis, the small bowel was the site most commonly involved at recurrence; residual tumor > 2.5 mm was the only independent risk factor for recurrence [38]. CC has consistently been one of the most predominant prognostic factors. It is related to the extent of peritoneal involvement and surgeon skill to remove all peritoneal disease [1–3, 32–34]. Lymph node metastases are rare in DMPM but correlate with poor outcome. This supports the necessity that any suspicious node be systematically removed during the CRS procedure [32, 33].
Biphasic and sarcomatoid histological variants are correlated with poor prognosis, although their clinical utility as prognostic factors is limited by their rarity [1]. Other pathological prognostic variables are nuclear/nucleolar size, depth of tumor invasion, and mitotic count.
In the above-mentioned series, a Ki67-positive cell rate < 10 % correlated at multivariate analysis with better OS and PFS [37]. The role of proliferative index for prognostic stratification was confirmed in an exhaustive clinicopathological analysis by Deraco et al. (personal communication) using the technology of tissue microarray (TMA), results of which were presented at the Ninth International Symposium on Locoregional Cancer Therapies, Steamboat Springs, CO, USA, 15–17 February 2014.
17.7 Molecular Biology
In DMPM, molecular and cellular mechanisms underlying the proliferative potential and resistance to therapy are still poorly understood. The biology of this disease has been thoroughly investigated by clinical and basic science researchers at Milan INT during the last decade. It has been demonstrated that p16 expression is frequently absent or reduced in patients with DMPM and that EGFR overexpression is more common in peritoneal than in pleural forms. However, no correlation with prognosis of overexpression of EGFR and matrix metalloproteases (MMP)-2 and -9 was found in patients treated in our institution [39].
Telomerase activity (TA) is expressed in the majority of DMPM and negatively impacts prognosis [40]. In DMPM specimens from 38 patients undergoing various therapies; we assessed TA using the telomeric repeat amplification protocol. The alternative lengthening of telomeres (ALT) mechanisms were studied by assaying ALT-associated promyelocytic leukemia nuclear bodies. ALT or TA alone was found in 18.2 % and 63.6 % of cases, respectively; both ALT and TA were positive in two cases. In the overall series, TA expression was significantly associated with disease relapse (p = 0.018) and cancer-related death (p =0.045); ALT was not associated with outcome. In a subset analysis, the prognostic relevance of TA was confirmed in patients uniformly treated by CRS plus HIPEC.
Overexpression of cytoprotective factors, including survivin and members of the inhibitors of apoptosis protein (IAP) family, were demonstrated by Zaffaroni et al. [5]. Those authors analyzed DMPM proliferative and apoptotic features and tested a survivin knockdown approach in a human DMPM cell line. DMPM cells were transfected with small-interfering RNA (siRNA) targeting survivin messenger RNA (mRNA). Survivin expression, growth rate, and ability to undergo spontaneous and drug-induced apoptosis was measured, showing low proliferation rates and poor apoptotic activity in DMPM cells. Survivin was expressed in 91 % of cases and the other IAPs in 69–100 %. Transfection of DMPM cells with survivin siRNA resulted in a survivin inhibition, a timedependent cell-growth decrease, and an enhancement of spontaneous and druginduced apoptosis. These results suggest that survivin may be a potential target for biological treatments in DMPM.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree