Peripheral Nerve Physiology, Anatomy, and Pathology
Shikha Sethi
Brian J. Harley
Christian Custodio
Michael Stubblefield
A comprehensive understanding of peripheral nerve anatomy and physiology is essential for understanding peripheral nerve pathophysiology and mechanisms of peripheral nerve injury and regeneration. Understanding peripheral nerve injury and cellular repair is critical to clinical management of operative nerve injury, microsurgical nerve repair, and emerging applications that target intrinsic nerve cell functions to assist in nerve regeneration.
Peripheral Nerve Anatomy
Gross Anatomy
General Organization
31 mixed spinal nerves emerge from the spinal cord:
8 cervical
12 thoracic
5 lumbar
5 sacral
1 coccygeal
Nerves emerge from the foramen of the vertebral bodies after the union of ventral and dorsal roots.
Autonomic, sensory, and motor fibers travel together in peripheral nerves to their destinations.
Nerves branch into dorsal and ventral rami upon exiting the foramen.
Dorsal rami
Small-caliber branches
Provide segmental innervation to dorsal paraspinal area
Ventral rami
Large-caliber branches
Cervical, lumbar, and sacral roots join together to form nerve plexuses to innervate the extremities.
Thoracic spinal nerves (except T1) do not form plexuses but instead provide segmental innervation to large areas of the ventral trunk.
Nerve Plexus
Coalescence of multiple spinal nerve ventral rami
Fairly consistent anatomic connections and exchanges within plexuses
Each root level still innervates specific dermatomal and myotomal segments.
At the distal aspect of the plexus, peripheral nerves form with representations from multiple spinal levels.
Four consistent locations
Cervical plexus
First four cervical roots
Brachial plexus
Lower four cervical and first thoracic ventral rami
Lumbar plexus
First three and a part of the fourth lumbar ventral rami
Sacral plexus
All sacral rami along with the fifth and a part of the fourth lumbar ventral rami
Peripheral Nerves
Each nerve may contain any combination of three possible nerve types:
Motor efferent fibers
Cell bodies in the spinal cord
Transmit motor information to muscles about when and how to act
Motor unit: individual motor neuron and the specific group of muscle fibers it innervates
Sensory afferent fibers
Cell bodies in dorsal root ganglia
Convey modality or quality, intensity, duration, and location of a stimulus from the periphery
Arise from specialized pain, thermal, tactile, and stretch (proprioceptive) receptors in the periphery
Terminal axons and presynaptic terminals for sensory fibers may be at the spinal level of the corresponding dorsal root ganglion or deeper in the central nervous system.
Sympathetic fibers
Originate in the intermediolateral cell column in the thoracic and upper lumbar spinal cord
Synapse at variable levels of the paravertebral sympathetic ganglion and then travel as fibers within mixed spinal nerves to end organs such as sweat glands, blood vessels, and erector pili
Fibers join the spinal nerve and can then branch into ventral and dorsal primary rami.
Microanatomy
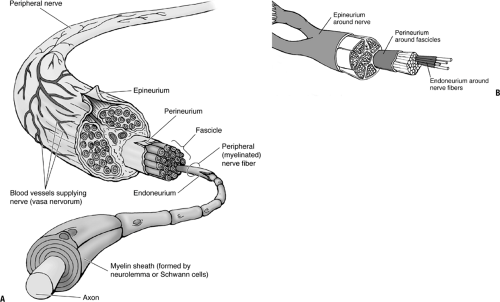
Nerves (Fig. 25-1)
The normal peripheral nerve is composed of blood vessels, nerve fibers, and three levels of connective tissue within which the fibers and vessels lie.
Epineurium
Outermost connective tissue layer
Represents up to 50% of the cross-sectional area of the nerve trunk
Loose meshwork of collagen and elastin fibers and is generally thicker where a nerve crosses a joint
Well-developed vascular plexus runs within the epineurium.
Functions to protect the nerve fiber bundles, called fascicles, within the nerve
Tough external epineurium surrounds periphery of nerve.
Loose internal epineurium occupies space between fascicles.
Perineurium
Thin, dense, multilayered connective tissue sheath that surrounds each fascicle
Tight basement membranes within the perineurium protect the endoneurial space by serving as a diffusion barrier.
Tensile strength of the perineurium helps maintain intrafascicular pressures.
Vascular structures traverse the perineurium obliquely to enter the endoneurial space.
Endoneurium
Delicate collagenous matrix with fibroblasts, mast cells, and a capillary network
Surrounds individual myelinated nerve fibers or groups of unmyelinated nerve fibers within a fascicle
Fascicles
All neurons within a peripheral nerve are bundled together into structures termed fascicles.
Fascicles are located within the internal epineurium.
Bounded by the perineurium
Fascicles are often grouped together into a larger unit.
Inner interfascicular epineurium bounds grouped fascicles.
Grouped fascicles can be easily divided along internal epineurial planes.
Major peripheral nerves will contain many grouped fascicles.
There is constant redistribution of fascicular organization along a peripheral nerve.
Interfascicular plexuses allow for interconnections.
Fascicles are more numerous and smaller where a nerve crosses a joint.
Smaller fascicles and more internal epineurium between them allows for increased protection of nerve fibers from external trauma and deformation.
As the nerve gives off branches along its course, the fascicles divide (see Fig. 25-1).
Small terminal nerves contain only one or two fascicles.
Example: digital nerve
Cellular Anatomy and Physiology
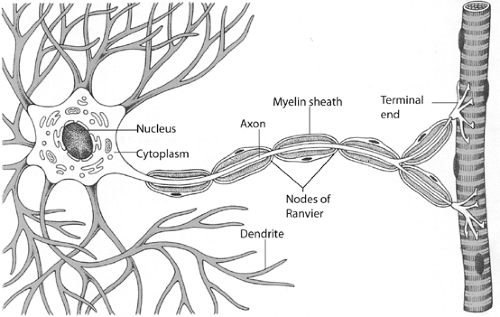
Neurons (Fig. 25-2)
Individual nerve fibers within the endoneurium of a peripheral nerve are termed neurons.
Neurons are extensions of a single nerve cell body.
Neurons are broken down into four distinct regions:
Cell body
Contains the nucleus of the nerve cell
Metabolic center of the nerve cell
Dorsal root ganglion contains the cell body for sensory nerve fibers.
Motor nerve cell bodies are found in the anterior horn cells of the spinal cord.
Dendrites
Thin processes that branch off the cell body
Receive inhibitory or stimulatory synaptic input from other cells
Synapse with both central and peripheral nervous systems
This input allows modulation of peripheral nerve function.
Axons
Each cell body gives rise to a single axon at its axon hillock.
Propagate electrical signals known as action potentials
Convey information over distances from cell bodies to nerve terminus
Axons may act at great distances from their cell bodies.
Example: Signal to extend great toe is generated in the motor cell bodies of the anterior horn cells of spinal nerve roots L5 and S1 and runs to the distal portion of the lower leg to innervate the extensor hallucis.
Presynaptic nerve terminal
Located at the distal end of the axon
Action potential causes changes in ion exchange at terminus.
Release of neurotransmitter at the synaptic cleft or neuromuscular junction results.
Schwann Cells and Myelin Sheaths
Specialized macroglial cells are called Schwann cells.
Surround peripheral nerve axons and produce myelin
70% lipid
30% protein
High concentration of cholesterol and phospholipids
Myelin provides electrical insulation for the electrical impulse.
Allows propagation of electrical impulses at faster speeds and at higher frequencies
Myelinated Axons
Wrapped throughout their length by concentric, tight spirals of layers of the Schwann cell membrane
Schwann cells line up end to end along the course of a single axon.
Entire length of the axon is surrounded.
Small spaces (up to 1.0 mm) between adjacent Schwann cells called nodes of Ranvier
Up to 500 Schwann cells may myelinate a single axon.
Unmyelinated Axons
Surrounded as a group by processes of a single Schwann cell
Conduction through these axons is comparatively slower.
Peripheral Nerves
Contain both myelinated and unmyelinated fibers in an average ratio of 4:1 traveling within each fascicle
Pathologic processes that disrupt the myelin sheath can slow conduction or cause focal conduction block.
Axoplasmic Transport
Specialized transport processes within a nerve cell
All cellular proteins and neurotransmitters are produced in cell body.
Cell body may be at a significant distance from the terminal axon.
Multiple transport mechanisms
Fast and slow anterograde transport
Move cellular proteins from the cell body to the axon
Fast retrograde transport
Removes debris and breakdown products from the distal axon back to the cell body
Mechanisms proposed consist of carrier proteins binding to microtubules within the nerve cell.
Electrophysiology of Peripheral Nerves
Nerve cells communicate via electrical and chemical impulses. Ion exchanges between the microenvironment inside and around a nerve fiber create electrical potential differences in the nerve cell. When certain threshold levels are reached, events such as release of neurotransmitter vesicles, or initiation of an action potential, occur.
Resting Cell Membrane and Electrical State
Neurons at rest have a negative potential within the cell between -50 and -80 mV.
Na+ and Cl– are concentrated on the outside of the neuron.
K+ and organic anions are concentrated on the inside.
Cell membrane is essentially impermeable to charged ions, except where specialized ion channels allow transit of charged ions.
Net ion flux across the membrane at rest is zero.
Actively maintained by the Na +/K+ pump
Excitatory and inhibitory neurons induce graded potentials in the nerve cell.
Act at cell body and dendrites
Membrane potential can become more or less negative as a result.
If sum of electrical activity received and processed reaches threshold, nerve depolarizes.
Depolarization
Depolarizing “all-or-nothing” initiation of an action potential
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree