Chapter 55 Penile Cancer
Early-stage, well-differentiated cancers of the penis can be effectively managed with local therapy, and attention should be paid to preservation of penile function and morphology. Primary surgical management is effective but can be associated with considerable psychosexual morbidity. Even partial penectomy can have a profound effect on sexual health and self-image.1 Suicide or attempted suicide after partial penectomy has been reported.2,3 EBRT or interstitial RT is an organ-sparing alternative that preserves penile morphology and function without compromising disease control or survival in selected patients. Unfortunately, many urologists do not routinely offer this penis-conserving option.4 Quality of life and sexual health after surgery is infrequently studied or reported.5 Sexuality and expectations should be discussed with the patient and partner when deciding on primary management. Advanced or poorly differentiated tumors require a multimodality approach.
Etiology And Epidemiology
Carcinoma of the penis is rare, with an estimated incidence of 1 case per 100,000 men in North America and Europe, where it accounts for 0.4% to 0.6% of cancers. Higher incidences are seen in parts of Asia, Africa, and South America, where it represents up to 10% of malignancies in male patients.6 The peak incidence is in the sixth decade in developed countries but earlier where the incidence is higher.
Case-control studies have identified important risk factors (odds ratio [OR] >10) to be phimosis, chronic inflammatory conditions such as lichen sclerosis, treatment with psoralens and ultraviolet A photochemotherapy (PUVA), smoking (dose-dependent association), and a history of genital condylomata (threefold to fivefold increase in risk). Neonatal circumcision is associated with a threefold decrease in risk of penile carcinoma. Circumcised men with a history of human papillomavirus (HPV) infection remain at increased risk7; and, in some series, up to 20% of patients have been circumcised neonatally. HPV types 16 and 18 have been identified in about 50% of invasive penile cancers.8,9
Prevention And Early Detection
Infant circumcision is highly effective in prevention of this disease, but it is no longer recommended on these grounds alone. The emphasis is instead on education, the promotion of good hygiene for the normally retractile foreskin, and surgical correction of phimosis. Men should be made aware of the association between certain HPV subtypes, venereal warts,7 and cancer, as well as the premalignant nature of conditions such as lichen sclerosis, which may precede the diagnosis of cancer by many years.
Biologic Characteristics And Molecular Biology
The overall incidence of HPV in penile carcinoma is 40% to 45%, as detected by polymerase chain reaction (PCR) amplification of DNA. HPV-16 and HPV-18 are the most frequent subtypes detected.10,11 The frequency of HPV detection depends on the histopathologic subtype of penile cancer. HPV association is seen in 80% to 100% of basaloid and warty penile cancers but in only approximately 35% of verrucous or squamous cell carcinomas. The difference in prevalence of HPV in these two groups suggests different pathogenesis. HPV presence in a tumor does not appear to confer a worse prognosis.
TP53 positivity is found in 41% to 75% of invasive penile cancers.12,13 In multivariate analysis, TP53 positivity and lymphatic embolization are predictive of lymph node metastases.12,14
Pathology And Pathways Of Spread
Premalignant lesions are associated with invasive cancers in 20% to 30% of cases. Intraepithelial neoplasia such as bowenoid papulosis, Bowen disease, and erythroplasia of Queryat15 are precursor lesions of warty and basaloid penile cancers. Lichen sclerosis (balanitis xerotica obliterans) is associated with non-HPV variants of penile carcinoma.16,17 Condylomata, Buschke-Löwenstein disease, Kaposi sarcoma, and leukoplakia are also associated with penile cancer.
Clinical Manifestations, Patient Evaluation, And Staging
General Approach
Because of the rarity of carcinoma of the penis, reported series often span several decades. Three different staging systems are encountered in a review of the literature of the past two decades18–20 (Table 55-1).
TABLE 55-1 Staging Systems for Carcinoma of the Penis
| Stage | Description |
|---|---|
| Jackson Staging System* | |
| 1 | Tumor limited to the glans or prepuce |
| 2 | Tumor extending into the shaft or corpora but without node involvement |
| 3 | Tumor confined to the shaft but with malignant but operable lymph nodes |
| 4 | Invasion beyond the shaft with inoperable lymph nodes or distant metastases |
| TNM (UICC, 1978)† | |
| Tis | Carcinoma in situ |
| T1 | Tumor ≤ 2 cm |
| T2 | Tumor > 2 cm and ≤ 5 cm |
| T3 | Tumor > 5 cm or deep invasion including urethra |
| T4 | Tumor invades adjacent structures |
| N1 | Metastases in unilateral inguinal lymph nodes |
| N2 | Metastases in bilateral inguinal lymph nodes |
| N3 | Fixed inguinal lymph nodes |
| TNM (UICC, 1987-2002)‡ | |
| T1 | Tumor in subepithelial connective tissue |
| T2 | Tumor in corpus spongiosum/cavernosum |
| T3 | Tumor in urethra/prostate |
| T4 | Tumor in other adjacent structures |
| N1 | Tumor in one superficial inguinal lymph node |
| N2 | Tumor in multiple/bilateral superficial inguinal lymph nodes |
| N3 | Tumor in deep inguinal or pelvic lymph nodes |
UICC, International Union Against Cancer (Union Internationale Contre le Cancer).
* From Jackson S: The treatment of carcinoma of the penis, Br J Surg 53:33-35, 1966.
† From Harmer M: Penis (ICD-0187). In TNM Classification of Malignant Tumours, ed 3, Berlin, 1978, Springer-Verlag, pp 126-128.
‡ From Hermanek PS, Sobin LH: Penis (ICD-0187). In Hermanek PS, Sobin LH, editors: TNM Classification of Malignant Tumours, ed 4, Berlin, 1987, Springer-Verlag, pp 130-132.
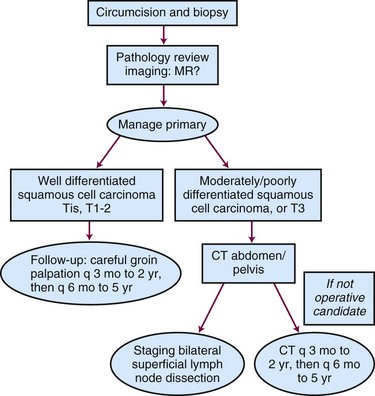
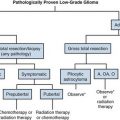
Clinical staging of carcinoma of the penis is very subjective, and it may be difficult to distinguish T1 (i.e., invasion of subepithelial connective tissue) from T2 (i.e., invasion of corpus spongiosum or cavernosum). For this reason, techniques that treat less than the full thickness of the penis must be restricted to very carefully selected cases. MRI may be helpful in cases that are difficult to stage clinically, with a positive predictive value for invasion of the corpora cavernosa of 75% (6 of 8 patients).21 When combined with artificial erection, MRI-guided staging showed good agreement with ultimate pathologic stage.22,23 Any patient who presents with phimosis and chronic discharge, bleeding, balanitis, or swelling in the region of the coronal sulcus or glans under an unretractable foreskin should have a dorsal slit of the foreskin to allow inspection of the glans and should preferably have a full circumcision. Any suspicious lesions should be sampled. Figure 55-1 shows the diagnostic algorithm for a clinically node-negative patient.
Lymph Node Assessment: The N0 Patient
Management of the patient with clinically negative groins remains controversial. Although the gold standard treatment for invasive penile cancer has been amputation and bilateral groin dissection,12 many RT series have advocated a “wait and see” policy, with no systematic staging investigations such as CT or fine-needle aspiration cytology.3,24–27 Because only about 20% of clinically negative nodes have micrometastases, staging lymph node dissection is not warranted for all patients. Furthermore, inguinal node dissection may be complicated in one third of cases by infection, skin flap necrosis, deep vein thrombosis, or severe leg edema.28,29,30
Nodal status is, however, the strongest predictive factor for OS.3,31,32 Lymph node dissection may be curative for men with microscopic regional spread. Several surgical series have identified that therapeutic node dissection confers an inferior survival compared with prophylactic node dissection.33 McDougal34 found a 5-year survival after inguinal node dissection of 92% for clinically N0 patients, compared with 33% for those with clinically involved nodes. Modified inguinal lymphadenectomy, sparing the saphenous vein and limiting the dissection laterally, distally, and proximally, may reduce morbidity.28
Stage and histopathologic factors should be used to identify patients at high risk for microscopic regional spread to selectively offer surgical staging of lymph nodes. Grade is predictive for regional failure, which occurs with 30% of well-differentiated and 81% of moderately to poorly differentiated tumors.29 T stage and lymphovascular invasion are also predictive for nodal relapse.31 McDougal34 reported that patients with clinically negative nodes but with poorly differentiated cancers or invasion of the corpora had a 78% rate of node positivity after inguinal dissection, compared with 4% for moderately or well-differentiated tumors and no invasion of the corpora.
The difficulty with applying this information to decision making in RT is that the primary tumor is not available for complete histopathologic examination. Invasion of the corpora may be underappreciated clinically. Diagnostic biopsies are often superficial and unreliable in determining the depth of invasion, the presence of lymphovascular invasion, or the ultimate tumor grade.35 However, if the biopsy shows the presence of lymphovascular invasion or moderate to poor differentiation, surgical assessment of regional lymph nodes is warranted.36 The specificity and sensitivity of CT are not sufficiently reliable for staging,37 although ultrasound-guided fine-needle aspiration cytology is a valuable tool to evaluate suspicious inguinal nodes.38
Dynamic sentinel lymph node mapping using a gamma probe after intradermal injection of technetium-99m around the primary tumor is becoming more widely available in the detection of early lymph node involvement.37 False-negative rates have fallen to 2% to 11% in the recent literature.39,40,41,42 The use of single proton emission computed tomography may decrease the risk of false-negative results from tumor blockage and rerouting of lymphatics,43 but superficial inguinal lymph node dissection remains the gold standard.
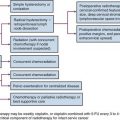
In summary, for patients with clinically negative nodes and a favorable primary tumor (Tis, Ta G1 to G2, T1 G1), observation of the inguinal regions is appropriate. For G2 to G3 or T2 disease, either a staging modified inguinal lymph node dissection or dynamic sentinel lymph node biopsy is recommended.44
Primary Therapy
Surgery
Circumcision is the first step in all cases. Small tumors that are limited to the prepuce can be treated by circumcision alone. Penis-conserving surgical techniques such as laser or Mohs surgery may be suitable for selected tumors. Mohs surgery45 for carcinoma in situ or very superficial tumors involves excision of tissue in successive layers with complete microscopic scanning of each horizontally cut layer to identify any tumor outgrowths that may extend beyond the visible or palpable lesion. Successive layers are removed until margins are histologically clear.
Laser surgery using carbon dioxide or neodymium:yttrium-aluminum-garnet (Nd:YAG) lasers has been reported to provide a superior functional and cosmetic result compared with standard surgical techniques for selected premalignant and malignant lesions.46,47,48,49 Most tumors appropriate for this modality are Tis or T1, the recurrence rate being unacceptable for T2 disease.46 Windahl and Andersson47 reported a 19% local recurrence rate for 67 patients, although 50% of failures could be re-treated with laser. Extended, careful follow-up is required because only 57% of local recurrences occur within the first 2 years, 30% between 6 and 10 years, and 15% after 10 years. Whether these late failures represent true local recurrences or new primary tumors is unknown.
Selected cases, especially those involving only skin, can be treated by wide excision, but local wedge excision is associated with a high recurrence rate. Glansectomy and reconstruction with a split-thickness skin graft preserves a greater length of penile shaft than traditional partial penectomy.50,51 Total or partial penectomy is indicated for larger or more invasive tumors. Traditionally, an adequate resection margin is considered to be 2 cm, but closer margins of 10 mm or less may be acceptable if tumor-free on frozen section.52 Partial penectomy is possible when the tumor involves the glans or the distal shaft, and the penile remnant will allow the patient to direct the urinary stream. Total amputation is indicated for larger or proximal tumors and requires a perineal urethrostomy.
Radiation Therapy
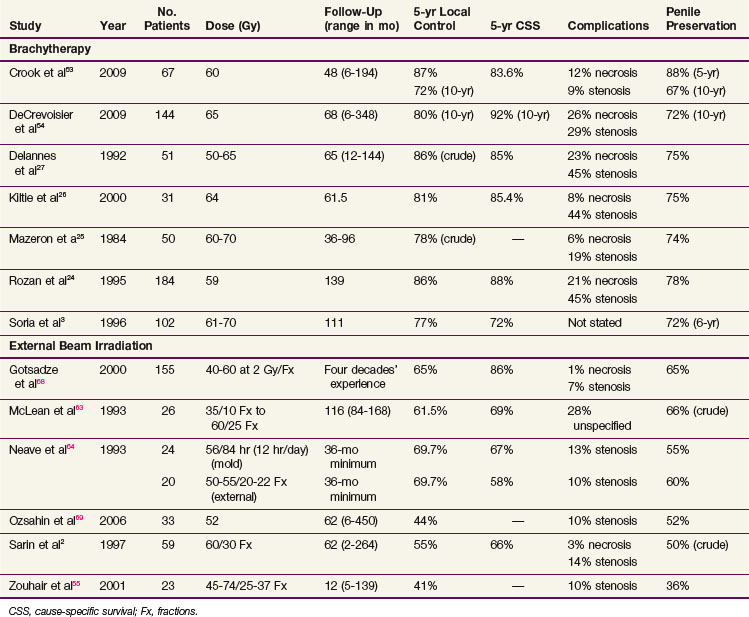
Radical RT in the form of brachytherapy or EBRT is effective in achieving local control in a high percentage of patients (Table 55-2). Often, series span several decades, during which time treatment techniques and dose prescriptions evolve. Staging systems have also undergone significant modifications (see Table 55-1).
Interstitial brachytherapy yields a 5-year local tumor control rate of 77% to 87%, with penile preservation rates at 5 years ranging from 72% to 88%. For EBRT, local control rates are less favorable, 41% to 70% at 5 years. The increased need for surgical salvage decreases penile preservation rates to 36% to 66%. Careful extended follow-up is recommended because local failures can occur several years after treatment. Crook and colleagues53 found that although five of eight local failures in a series of 67 men occurred in the first 2 years, the remaining three occurred at 4.5, 7, and 8 years. Similarly, Mazeron and associates25 reported that 18% of local failures occurred between years 5 and 8, and de Crevoisier and colleagues54 reported that 20% of the local failures occurred after 8 years. This late recurrence pattern is strikingly similar to that seen after penile-conserving laser treatment47 and necessitates careful long-term follow-up because the majority can be successfully salvaged.