PATHOGENESIS OF HYPOOSMOLALITY
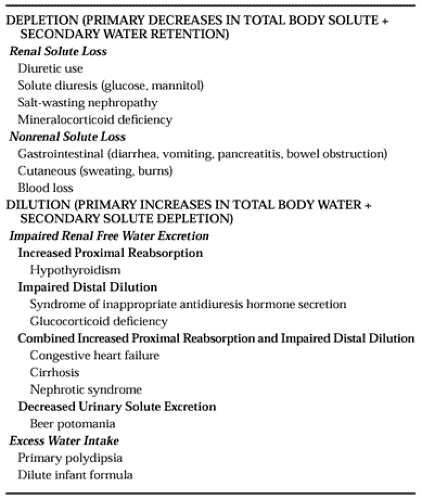
The presence of true hypoosmolality always signifies an excess of water relative to solute in the ECF. Because water moves freely across most cell membranes between the ICF and ECF, this usually also implies an excess of total body water relative to total body solute. As shown in Table 27-1, an imbalance between water and solute can be generated either by a depletion of total body solute in excess of concurrent body water losses, or by a dilution of total body solute secondary to increases in total body water. This classification represents an obvious oversimplification, because most hypoosmolar states have components of both solute depletion and water retention. Nonetheless, it represents a valid starting point for understanding the mechanisms underlying the pathogenesis of hypoosmolality and also provides a useful framework for discussing the treatment of hypoosmolar disorders.
SOLUTE DEPLETION
Depletion of body solute can result from any significant ECF losses. Whether by renal or nonrenal routes, the fluid loss itself rarely causes hypoosmolality because excreted or secreted fluid usually is isotonic or hypotonic relative to serum. Therefore, when hypoosmolality accompanies ECF losses, it is generally the result of replacement of the fluid losses by hypotonic solutions, causing dilution of the remaining body solutes. This usually occurs when patients drink only water in response to ongoing solute and water losses, but it can also occur when hypotonic fluids are administered intravenously to hospitalized patients. When solute losses are marked, these patients show obvious signs of volume depletion (e.g., addisonian crisis; see Chap. 76). However, such patients often have a more deceptive clinical picture because their volume deficits may be partially replaced. Moreover, they may not manifest signs or symptoms of cellular dehydration because osmotic gradients act to draw water into the relatively hypertonic ICF compartment, causing cellular volume expansion. Consequently, although clinical evidence of hypovolemia strongly supports solute depletion as the cause of plasma hypoosmolality, the absence of clinically evident hypovolemia never completely eliminates this possibility. Although ECF solute loss is responsible for most cases of depletion-induced hypoosmolality, ICF solute loss can also lead to hypoosmolality as a result of osmotic water shifts into the ECF. This mechanism likely contributes to the hypoosmolality that is observed in some cases of diuretic-induced hypoosmolality in which marked depletion of total body potassium occurs.8
WATER RETENTION
Despite the importance of solute depletion in some patients, most cases of clinically significant hypoosmolality are caused by increases in total body water rather than by losses of extra-cellular solute. Theoretically, this can occur because of either impaired renal free water excretion or excessive free water intake. However, the former accounts for most hypoosmolar disorders because normal kidneys have sufficient diluting capacity to allow excretion of 20 to 30 L per day of free water.9 Intakes of this magnitude are occasionally seen in psychiatric patients, but not in most patients with primary polydipsia. Furthermore, studies have demonstrated that psychotic patients with polydipsia and hyponatremia also have abnormalities of free water excretion.10 Consequently, dilutional hypoosmolality usually implies an abnormality of renal free water excretion. The renal mechanisms responsible for impairments in free water excretion are commonly classified according to whether the major effect occurs in the proximal or distal nephron (see Table 27-1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree