PARATHYROID GLAND AND CALCIUM HOMEOSTASIS
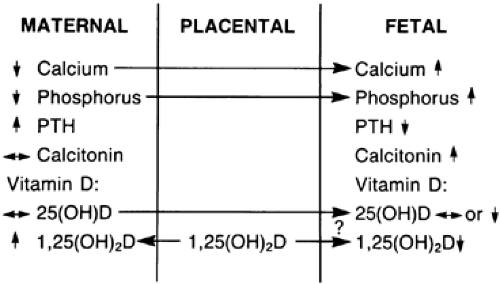
The calcium levels in the fetus are regulated largely by transfer from the maternal compartment across the placenta. The maternal compartment undergoes a number of adjustments that ultimately permit a net transfer of sufficient calcium to sustain fetal bone growth. These changes include increases in maternal dietary intake, in circulating maternal vitamin D [1,25(OH)2D], and in circulating parathyroid hormone (PTH). Serum calcitonin levels increase (see Chap. 53). The levels of total calcium and phosphate decline, but ionized calcium levels remain unchanged.96 The “placental calcium pump” creates a positive gradient of calcium and phosphorus to the fetus (Fig. 108-7). Circulating fetal calcium and phosphate levels increase steadily throughout gestation, and fetal levels of total and ionized calcium as well as of phosphate exceed maternal levels at term. The active transport of calcium to the fetus increases from 50 mg per day at 20 weeks to 350 mg per day by 35 weeks, and the total accumulation of calcium in the fetus is about 30 g.97
The fetal parathyroid gland contains PTH, and the gland can secrete hormone by 10 to 12 weeks’ gestation.98 The fetal plasma levels of PTH are low and increase after delivery. Likewise, the fetal thyroid contains calcitonin, and serum calcitonin levels in the fetus are elevated.96,99 Because there is no transfer of PTH or calcitonin across the placenta, the consequences of the changes in these hormones on fetal calcium are consistent with an adaptation to conserve and stimulate bone growth within the fetus. Parathyroid hormone–related protein (PTHrP) is localized in the fetal parathyroid gland and plays a major role in fetal bone development and calcium homeostasis.100 PTHrP knock-out mice die at birth with a number of skeletal anomalies.101
The levels of the various forms of vitamin D are lower in the fetus than in the maternal compartment. The placenta and decidua are capable of 1α-hydroxylation and of formation of the active metabolite 1,25(OH)2D. However, the role, if any, of this hormone in the fetus is unknown, since its principal effect is on intestinal absorption of calcium.102
Serum calcium and phosphate levels fall in the neonate. Serum PTH levels begin to rise 48 hours after birth, and calcium and phosphate levels increase gradually over the following several days and are dependent on dietary intake of milk. Neonatal hypocalcemia, defined as a serum calcium concentration below 7 mg/dL, is a common complication of premature delivery, maternal diabetes, and birth asphyxia. The rare neonatal hypercalcemia may be caused by excessive maternal intake of calcium or vitamin D. Also, inadequate treatment of maternal hypoparathyroidism with resultant hypocalcemia may cause fetal hyperparathyroidism and elevated calcium levels early in neonatal life.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree