Study [Reference]
No. (PSM origin)
Drugs
Operative time (min)
HIPEC duration (min)
Hospital stay (days)
Mortality
Morbidity
Ascites resolution
Median survival (months)
Chang et al. 2001 [33]
2 (1 MPM, 1 BL)
CDDP
282
90
3–8
0
No
50 %
–
Facchiano et al. 2008 [34]
5 (GI)
MMC + CDDP
–
60–90
23
0
1 (delayed GI emptying
100 %
3
Patriti et al. 2008 [35]
1 (PM)
CDDP + DOXO
–
60
7
0
No
100 %
6
Valle et al. 2009 [36]
52 (15 GI, 11 colon, 13 ovarian, 8 breast lobular
CDDP + DOXO
147
90
2.3
0
3 (2 wound infection, 1 deep vein thrombosis
94 %
3
Ba et al. 2010 [37]
16 (GI)
5-FU + OXA
80
90
NR
0
1 (grade 2 bone marrow suppression)
100 %
5
Graziosi et al. 2009 [38]
1 (PM)
CDDP + DOXO
–
60
7
0
1 (hyponatremia)
100 %
11
De Mestier et al. 2012 [39]
2 (1 GI, 1 OC)
MMC + CDDP
120
25
–
0
–
100 %
7 GI, 3 OC
Di Giorgio 2013 (unpublished)
13 (4 GI, 1 PMP, 8 OC)
MMC, 5-FU + OXA CDDP
157
60
5
0
No
92.3 %
8 OC, 4 GI, 2 PMP
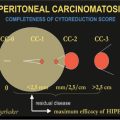
New drugs and new IP administration modalities are being studied: Kobold et al. reviewed current evidence suggesting that IP administration of the antivascular endothelial growth factor (VEGF) antibody, bevacizumab, might prevent local fluid accumulation [45–48]. Other studies considered the possibility drug delivery using a nebulized aerosol driven throughout the abdominal cavity by the pneumoperitoneal pressure [pressurized IP aerosol chemotherapy (PIPAC)]. Tempfer et al. applied compassionate treatment to 18 patients affected by unresectable PC from platinum-resistant OC, primary malignant peritoneal (PMP), and fallopian-tube cancers: Ten underwent PIPAC only; in eight, CRS was associated. Cisplatin at 7.5 mg/m2 and doxorubicin at 1.5 mg/m2 were perfused for 30 min at 37°C. In eight patients, PIPAC was repeated up to six times. Treatment was well tolerated and achieved an objective tumor response in six of eight patients who underwent more than one PIPAC treatment, although the rate of ascites control was not reported [49]. These results match with other, similar studies, on CRC, GC, and appendiceal cancers, suggesting PIPAC is a feasible and promising new modality of IP drug delivery [50, 51].
In conclusion, in patients with PC and MA who are not candidates for CRS, laparoscopic HIPEC can be safely and effectively administered, achieving satisfactory results, good MA control, and improved QoL. Other benefits are short hospitalization and very low morbidity and mortality rates, but there is no survival benefit. New drugs and new perfusion modalities are being studied to improve these promising results.
23.3 Palliative Surgery and Managing Bowel Obstruction in Peritoneal Carcinomatosis
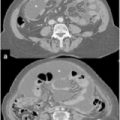
Malignant bowel obstruction is a common event in patients with locally advanced cancers, reaching an incidence of 28 % in GI cancer and 51 % in OC [1, 2]. Symptoms are related to the level of obstruction and usually include severe abdominal pain and distension, nausea, vomiting, and inability to pass gas and stool [52]. In patients with advanced or end-stage digestive or gynecological cancers, the onset of bowel obstruction may be insidious, evolving over several weeks and presenting spontaneous remissions between acute relapses [53]. Malignant bowel obstruction may have both mechanical and functional origin: the former is related to direct compression or infiltration by tumor masses of bowel loops, and the latter is related to impaired intestinal motility, resulting from tumor infiltration of mesenteries, nerves involved in intestinal motility, massive ascites, or chronic opioid therapies. Computed tomography is the gold standard for diagnosing malignant bowel obstruction, as it has a specificity and sensitivity > 90 % [54]. CT can exclude nonneoplastic causes of obstruction, which can occur in 15–30 % of patients with carcinomatosis and are mostly related to adhesions, hernias, and eventration [55, 56]. It can also identify the presence of a surgical emergency, such as perforation, volvulus, or strangulation, all of which are surgical indications even for palliative care. Decision making is very difficult in these patients. Medical conservative treatment is often not effective to relieve symptoms, and major surgical procedures should be avoided in patients who have limited life expectancy and who are poor surgical candidates because of malnutrition and underlying disease [57]. A large review by Laval et al. proposed recommendations and practical clinical guidelines to guide decision making, reserving surgery for patients with nonneoplastic mechanical obstruction, emergency situations, and limited obstruction with no indications to endoscopic prosthesis. Conservative medical management is preferred for patients with single stenosis suitable for endoscopic treatment, in poor general condition, or with extensive carcinomatosis, multiple areas of stenosis, or mesentery-root invasion. Age, comorbidities, nutritional status, previous radiotherapy, and level of obstruction are also identified as poor prognostic factors for surgical treatment [52] (Table 23.2).
Table 23.2
Prognostic factors influencing surgical treatment of malignant bowel obstruction in unresectable peritoneal carcinomatosis
– | Advanced age |
– | Presence of comorbidities |
– | Poor performance status |
– | Extent of peritoneal carcinomatosis; particularly, presence of multiple levels of obstruction |
– | Small-bowel rather than large-bowel obstruction |
– | Previous abdominal or pelvic radiotherapy |
Conservative management of patients with malignant bowel obstruction includes fasting, intravenously delivered rehydration, total parenteral nutrition, nasogastric tube (NGT) placement, and antiemetic, antisecretory, analgesic, and corticosteroid drug administration. Antisecretory drugs, which reduce digestive secretions such as octreotide, are particularly important in relieving patient distress; if vomiting does not stop, a venting gastrostomy rather than long-term NGT may be considered [52]. Endoscopic prosthesis must be preferred to surgery when technically possible due to its lower morbidity and mortality rates; PC must not be considered a contraindication to stent placement in patients with a single-site bowel obstruction [58]. Complications are rare and include perforation (0.5–4 %) and stent migration (8–12 %) and obstruction (0.5–10 %). Technical failure is more frequent in long-standing stenosis [59].
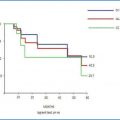
A surgical approach should be carefully considered when conservative treatment fails or is not possible. Surgical procedures include ostomies (colostomy, ileostomy, jejunostomy), small- or large-bowel resections and/or bypass, and lysis of either malignant or inflammatory adhesions. Surgical strategy is determined upon intraoperative findings, and no standard guidelines are available. Several studies demonstrated benefits in symptoms relief with resumption of oral intake after palliative surgery for malignant bowel obstruction in 32–100 % of patients [60–66]. QoL measures are not reported by any available study. The literature reports that perioperative morbidity and mortality and rates are high, ranging from 7 % to 44 % and from 6 % to 32 %, respectively [60–62, 65, 67–69]. A frequent complication, occurring in from 6 % to 47 % of patients, is reobstruction [61–63, 66, 69]. Furthermore, duration of symptom relief may be short [66, 69] and hospital stay considerable in relation to patients life expectancy, which ranges from 1 to 94 days [70]. When obstructive symptom resolution is achieved and is long lasting, survival advantage may be significant, rising from 26 to 36 days to 154 to 192 days in some series [62, 71]. Table 23.3 summarizes the most relevant experiences and results in surgical treatment of malignant bowel obstruction in patients with PC. Authors experience is detailed in Table 23.4: overall median survival was 96.1 days (OC 100.3 days, GI cancer 83.5 days, CRC 104.5 days), and mean hospital stay was 9.6 days (range 6–14). Operative mortality occurred in two patients (17 %): one died after reoperation for bleeding, and reobstruction occurred in one, who died after 28 days.
Table 23.3
Malignant bowel obstruction in peritoneal carcinomatosis: outcomes (%) of palliative surgery
Study [Reference] | No. | Primary | Symptom relief | 30-day mortality | Morbidity | 60–90 days reobstruction |
|---|---|---|---|---|---|---|
McCarthy [60] | 12 | OC 7, GI 5 | 75 | 25 | 25 | NR |
Turnbull et al. [61] | 89 | GI 84, HPB 5 | 74 | 13 | 43 | 38 |
Lau and Laurentz [62] | 30 | GI 30 | 57–63 | 17 | 27 | 47 |
Van Ooijen et al. [71] | 59 | GYN 46, GI 8, HPB 1, other 4 | 34–76 | NR | NR | 15 |
Blair et al. [67] | 63 | GI 44, HPB 5, other 14 | 45 | 21 | 44 | NR |
Legendre et al. [72] | 109 | GYN 37, GI 46, other 26 | 61 | NR | NR | NR |
Abbas and Merrie [68] | 79 | GI 34, GYN 19, other 25 | NR | 10 | 35 | NR |
Piver et al. [73] | 60 | OC 60 | NR | 17 | 31 | NR |
Lund et al. [63] | 25 | OC 25 | 32 | 32 | 32 | 38 |
Rubin et al. [74] | 52 | OC 52 | 65–87 | 17 | 15 | NR |
Bais et al. [75] | 19 | OC 19 | 68 | 11 | 32 | 21 |
Jong et al. [64] | 53 | OC 53 | 68 | 32 | NR | 40 |
Pothuri et al. [76] | 64 | OC 64 | 58 | 6 | 22 | 6 |
Mangili et al. [65] | 47 | OC 47 | 59 | 22 | 33 | NR |
Chi et al. [66] | 14 | OC 14 | 100 | NR | 7 | 29–36 |
Kim et al. [77] | 23 | OC 23 | 48 | NR | 13 | NR |
Kolomainen et al. [69] | 90 | OC 90 | 66 | 18 | 27 | 17 |
Di Giorgio (unpublished) | 12 | OC 6, GI 6 | 100 | 17 | 25 | 8 |
Table 23.4
Palliative surgery for malignant bowel obstruction in peritoneal carcinomatosis: personal experience
Patient no. | Primary tumor | PCI (mean = 26) | Surgical procedure | Morbidity | Hospital stay (days) mean = 9.6 | Survival (days) Mean = 96.1 |
|---|---|---|---|---|---|---|
1 | GI | 24 | Mesenteric implants resections | None | 14 | 94 |
2 | OC | 27 | Left colostomy | None | 6 | 112 |
3 | OC | 28 | Adhesiolysis | Reobstruction | 13 | 28 |
4 | OC | 26 | Right ileostomy | None | 13 | 163 |
5
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|