Definition: Palliative medicine is a specialized medical care for people w/serious or life-threatening illnesses. It improves the QoL of pts & their families by focusing on tx of pain & other physical sx as well as relief of the psychosocial & spiritual distress that comes w/a dx of a serious illness.
The palliative care IDT includes physicians, nurse practitioners, nurses, pharmacists, social workers, case managers, psychiatrists, psychologists, & spiritual care counselors who work together w/the pt’s 1° doctor(s) to provide an extra layer of support
Palliative care is appropriate at any age & at any stage of a serious illness & can be provided along w/curative or palliative tx in an outpatient clinic, hospital, nursing home, skilled facility, or at a pt’s home
Hospice care is a delivery system that provides palliative care to terminally ill pts
Request a palliative care consult for assistance w/pain & sx management, advance directives, capacity assessment, establishing GOC, breaking bad news, prognostication, withdrawal of life-sustaining tx, disposition planning, addressing end-of-life nutritional support, initiating family meetings, identifying existential distress, addressing spiritual & cross-cultural issues, making appropriate hospice referrals & evaluation for bereavement care
Assessment is focused on what the pt feels are the most important sx/issues that they need assistance w/
Respect for the dignity of both the pt & caregivers
Alleviation of pain & other physical sx
Assess & manage the psychological, social, & spiritual difficulties
Provide access to therapies that may realistically improve the pt’s QoL, including alternative or nontraditional tx
Respect the pt’s right to refuse tx
Offer continuity of care (ie, pt should be able to be cared for by his or her 1° care and/or specialist provider)
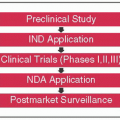
Promote clinical & evidence-based research on providing care at the end of life
Provide access to palliative care & hospice care
The main purpose of a family meeting is to improve communication & address any conflicting goals & values between the clinicians, pt, & families. It is a key instrument in sharing medical info, disclosing prognosis, establishing GOC based on the pt’s desires, discussing advance directives & disposition planning in conjunction w/what is medically feasible. This serves as an extra layer of support for the pt, the family, & the medical team.
Please see “SPIKES” model for breaking bad news
| ||||||||||||||||
Physicians tend to be optimistic when determining prognosis & can overestimate by a factor of five (BMJ 2000;320(7233):469-472)
Pts & physicians make different care decisions based on prognosis so it is essential that it is as accurate as possible
There are certain common s/s typical indicative of end-stage illnesses (Am J Soc 1992;93:663, Cancer 1984;53:2002)
| ||||||||||
Nociceptive pain
Somatic pain: Due to nociceptors activation in body surface or musculoskeletal tissues (ie, met bone disease, soft tissue tumors)
Visceral pain: Due to activation of receptors from compression, obstruction, infiltration, ischemia, stretching, or inflammation of the thoracic, abdominal, or pelvic viscera; not well localized (ie, bowel obstruction, bulky liver mets, urinary retention)
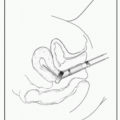
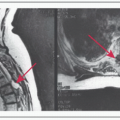
Neuropathic pain: Due to direct injury or dysfunction of peripheral or CNS
tissues (ie, compression radiculopathy, postmastectomy & postthoracotomy pain, postherpetic neuralgia)
Pain emergency: Pain crisis, spinal cord compression, bone fracture, bowel obstruction, & sev. mucositis
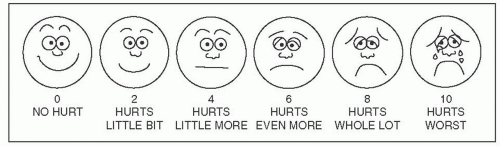
The pt, not the observer, should complete the scale
Measure pain w/a numeric pain intensity scale of 0-10, verbal rating scale, or a visual analog scale can be used for children or adults
Step 1: For mild pain, use acetaminophen, NSAIDs, or another adjuvant analgesic
Step 2: For mild-to-mod. pain, or persistent pain, add a lower potency opioid (codeine) or a low dose of a stronger opioid (morphine)
Step 3: For mod. -to-sev. pain, or worsening pain, use strong opioids (morphine, hydromorphone, or fentanyl) (World Health Organization. Cancer Pain Relief with a Guide to Opioid Availability, 2nd ed. Geneva, Switzerland: World Health Organization; 1996)
For mod.-to-sev. pain (w/close supervision):
In opioid naïve, start w/prn IV morphine 2.5-5 mg (or an equivalent); in opioid-tolerant, start w/20% of the daily dose IV every 15 min-2h prn
After determining the effective & tolerated daily dose (sum of all doses given w/in the last 24 h), give the opioid around the clock & 10-20% total daily dose q1-2h prn
Adjust baseline upward daily based on total amount of prn
When converting from one opioid to another, reduce the equianalgesic dose by 1/3-1/2 (see table for rotation to methadone)
Consider multidisciplinary team approach & a consultation w/an addiction specialist
Manifestations: Respirations <6/min, myoclonic twitching, constricted pupils, skeletal muscle flaccidity, cold or clammy skin
Stop administering opioids, wait for the medication to wear off, stimulate pt
| |||||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree