OVULATION INDUCTION
Michael A. Thomas
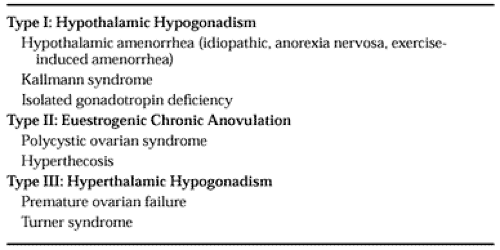
Ovulation induction is the primary method of ovarian stimulation in the 20% of infertile women who have an ovulatory defect. The World Health Organization (WHO) classifies those women with an inability to ovulate into three categories (Table 97-1).1 Women for whom hypothalamic amenorrhea (HA) is the cause of their dysfunction comprise WHO type I. Such individuals, who generally have low to low-normal gonadotropin secretion with estradiol concentrations in the postmenopausal range, do not have withdrawal bleeding when administered exogenous progestin and have normal prolactin levels. Disorders in this category include Kallmann syndrome, isolated gonadotropin dysfunction, and some secondary causes of amenorrhea (anorexia nervosa, psychogenic or exercise-induced amenorrhea). Conception can be achieved most easily with pulsatile administration of gonadotropin-releasing hormone (GnRH) or administration of exogenous gonadotropins.
Individuals with WHO type II ovarian dysfunction are euestrogenic with an abnormal ratio of luteinizing hormone (LH) to follicle-stimulating hormone (FSH), although the gonadotropin levels are usually in the normal range. Most of these patients
have polycystic ovary syndrome (PCOS) with accompanying symptoms of obesity, hirsutism, and anovulation (see Chap. 95 and Chap. 96). The most commonly used agents for ovulation induction in this group are clomiphene citrate and exogenous gonadotropins (see Chap. 96 and Chap. 101). Investigators have used insulin receptor–sensitizing agents like metformin and troglitazone (no longer available) to increase the possibility of monofollicular development. This approach must be viewed as experimental.
have polycystic ovary syndrome (PCOS) with accompanying symptoms of obesity, hirsutism, and anovulation (see Chap. 95 and Chap. 96). The most commonly used agents for ovulation induction in this group are clomiphene citrate and exogenous gonadotropins (see Chap. 96 and Chap. 101). Investigators have used insulin receptor–sensitizing agents like metformin and troglitazone (no longer available) to increase the possibility of monofollicular development. This approach must be viewed as experimental.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree