Introduction
There are few endocrine syndromes with as dramatic and systemic a clinical presentation as that seen with overt thyrotoxicosis. While even a young and previously healthy individual may experience a significantly diminished functionality with thyrotoxicosis, patients with pre-existing comorbidities such as ischemic heart disease may experience complications that threaten their survival. This chapter will provide an overview of systemic manifestations of overt thyrotoxicosis, with an emphasis on a complete clinical assessment of the thyrotoxic patient. It will serve as an introduction for the dedicated chapters on organ system manifestations of thyrotoxicosis that comprise this section.
Prevalence of Clinical Findings
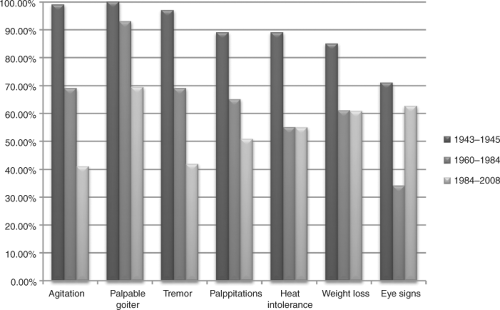
The prevalence of clinical manifestations in overt thyrotoxicosis depends on the etiology and severity of the disease, as well as the presence of important modifying factors, such as age and comorbidity (1,2,3). Patients with Graves’ disease are generally more likely to present with moderate or severe thyrotoxicosis than patients with other etiologies of thyrotoxicosis and therefore are more likely to have systemic complaints related to thyrotoxicosis. The effect of age and comorbid conditions on the clinical presentation is discussed below. Table 24.1 and Figure 24.1 show the relative prevalence of clinical manifestations in thyrotoxicosis and the manner in which the clinical presentation of thyrotoxicosis has changed from the 1940s through the present day concurrent with improvements in the sensitivity of testing for thyrotoxicosis.
Organ System–Specific Manifestations
Central Nervous System
The Senses
Varying degrees of sensory deficit corresponding to each of the five senses have been described as an effect of thyrotoxicosis and its treatment, or related to accompanying disease states. Visual disturbances in thyrotoxicosis occur primarily as a complication of Graves’ ophthalmopathy due to optic nerve compression at the apex of the orbit, diplopia related to extraocular muscle dysfunction, or rarely, damage to the cornea. Sensorineural hearing loss while common in hypothyroidism, occurs rarely in thyrotoxicosis, and has been attributed to an adverse drug effect of the thionamides (4,5). Olfactory toxicity has also been ascribed to methimazole use in laboratory animals, but similar data has not been published in humans. An altered sense of smell may occur as a complication of orbital decompression surgery in patients with Graves’ ophthalmopathy (6). Disorders of taste have been described in both hypothyroidism and hyperthyroidism (7). Peripheral neuropathy occurs in association with thyrotoxicosis, including symmetric distal sensory neuropathy (8), carpal tunnel syndrome (9), and due to coexistence of vitamin B12 deficiency (10).
Table 24.1 Prevalence of Clinical Findings in Patients with Overt Thyrotoxicosis by Perioda | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Neuromuscular Abnormalities
Tremor associated with thyrotoxicosis is most evident in the hands, but can occur elsewhere, such as in the tongue, trunk, and lower extremities. It is believed to be due to beta-adrenergic stimulation and responds dramatically to beta-adrenergic blocking agents. Chorea, which is a rapid, non-repetitive, random movement of the extremities or less commonly the facial muscles or trunk, has been described in thyrotoxic patients and resolves following successful treatment of the patient’s thyroid condition (11).
Myopathy occurs to some degree in the majority of patients with overt thyrotoxicosis. It is frequently proximal in location, and most commonly involves the pelvic girdle and shoulder muscles. In one prospective cohort, muscle complaints occurred in 67% of thyrotoxic patients, most of whom had demonstrable weakness by dynamometric testing in four or more muscle groups (8). Muscular weakness in this study correlated with serum-free T4 concentrations, and was not associated with creatine kinase enzyme elevations; it resolved an average of 3.6 months following therapy.
Myasthenia gravis occurs infrequently (less than 1%) in patients with Graves’ disease (12,13), but conversely, autoimmune thyroid disease occurs frequently in patients with myasthenia gravis. A retrospective review found that 7.7% of myasthenia gravis patients carried a diagnosis of Graves’ disease, and another 4.2% had a history of Hashimoto’s thyroiditis (14). Myasthenia gravis occurring in the setting of Graves’ disease in this study occurred at a younger age and was more likely to be associated with thymic hyperplasia.
Thyrotoxic periodic paralysis occurs as a result of an intracellular shift of potassium in a genetically and clinically susceptible patient. Occurring most frequently in Asian males,
patients with this disorder present with episodic paralysis following an episode of carbohydrate ingestion or intense physical exercise, and are noted to have clinical and laboratory evidence of thyrotoxicosis. Total body stores of potassium are normal in these individuals, but serum potassium during an episode of paralysis may be <1.5 mEq/L. Initial judicious therapy with intravenous potassium is often required, taking care to avoid rebound hyperkalemia. The addition of beta-adrenergic blocking agents reduces the frequency of repeat attacks while awaiting a return to euthyroidism. Interestingly, mutations within Kir2.6, an inward rectifier potassium channel, have recently been implicated in the susceptibility of at least one-third of thyrotoxic periodic paralysis patients (15).
patients with this disorder present with episodic paralysis following an episode of carbohydrate ingestion or intense physical exercise, and are noted to have clinical and laboratory evidence of thyrotoxicosis. Total body stores of potassium are normal in these individuals, but serum potassium during an episode of paralysis may be <1.5 mEq/L. Initial judicious therapy with intravenous potassium is often required, taking care to avoid rebound hyperkalemia. The addition of beta-adrenergic blocking agents reduces the frequency of repeat attacks while awaiting a return to euthyroidism. Interestingly, mutations within Kir2.6, an inward rectifier potassium channel, have recently been implicated in the susceptibility of at least one-third of thyrotoxic periodic paralysis patients (15).
Seizure and Stroke
Seizures are a well-recognized component of thyroid storm (16), but are only seen in a minority (<1%) of patients with moderate thyrotoxicosis. In a recent series of six patients with first seizures occurring in association with thyrotoxicosis, the subtype was generalized tonic–clonic in four patients, complex partial seizures with secondary generalized tonic–clonic seizures in two patients, and a focal seizure in one patient (17). Although the exact mechanism through which thyroid hormone elevation contributes to seizures is unknown, both seizures and electroencephalogram abnormalities resolve with correction of thyroid hormone levels in affected patients, and recur with subsequent episodes of thyrotoxicosis (17).
Behavioral Health Manifestations
Thyrotoxicosis is associated with a number of neuropsychiatric symptoms, including restlessness, irritability, agitation, emotional lability, anxiety, depression, and infrequently encephalopathy, psychosis, and coma. In a number of small studies, 30% to 100% of patients with overt thyrotoxicosis meet DSM-III criteria for one or more psychiatric disorders, with depression and generalized anxiety occurring most commonly (20). A recent case-control study found that among 31 patients with Graves’ hyperthyroidism, 18 had positive depression scores on a standardized scale, including one patient with severe depression requiring medical therapy, and 17 patients with mild-to-moderate depression (21). Likewise, 27 of 31 patients in this study received mild-to-moderate
anxiety scores on standardized testing, compared to none of 34 matched control patients.
anxiety scores on standardized testing, compared to none of 34 matched control patients.
Compared to anxiety and depression, psychosis is a rare manifestation of thyrotoxicosis. Among 18 patients hospitalized with concurrent thyrotoxicosis and psychosis at a single medical center over a 20-year period, 13 patients manifested delusional behavior, 8 experienced hallucinations, and 3 patients demonstrated suicidal behavior (22). Encephalopathy and coma are rare manifestations of life-threatening thyrotoxicosis or thyroid storm (16).
Cognitive impairment has been inconsistently identified in patients with thyrotoxicosis. In one recent study, thyrotoxic patients were more likely to report problems with memory or concentration than control patients, but the two groups had similar scores on neuropsychological testing (21).
Cardiovascular Manifestations
Among the many clinical manifestations of thyrotoxicosis, cardiovascular complications have the highest potential for life-threatening consequences. An increase in cardiovascular deaths has been repeatedly demonstrated among patients with a diagnosis of thyrotoxicosis (23,24). The increased metabolic demand associated with thyrotoxicosis leads to changes in a number of cardiovascular parameters with a net effect of 1) increasing cardiac oxygen demand and the risk of ischemia; 2) enhancing the risk of atrial arrhythmia, particularly fibrillation; and 3) promoting the development of congestive heart failure in susceptible individuals (25). While even patients without pre-existing cardiovascular disease may experience arrhythmia and associated thromboembolic phenomena, the greatest potential for morbidity and mortality occurs in patients with pre-existing cardiovascular disease, such as the elderly.
Pulmonary Manifestations
Dyspnea on exertion is a common manifestation of thyrotoxicosis. Contributing factors include respiratory muscle weakness (26,27), enhanced ventilatory drive (28), diminished lung compliance (29), and concurrent cardiovascular complications with respiratory consequences, such as congestive heart failure. Compared to the euthyroid state, thyrotoxicosis is associated with a relatively ineffective rapid and shallow breathing pattern, enhanced oxygen utilization and carbon dioxide output, and a lower anaerobic threshold (the point at which ATP demand outpaces oxygen-mediated ATP generation) (30). These changes correlate with the severity of thyrotoxicosis and are reversed with restoration of euthyroidism (30).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree